Investig Magn Reson Imaging.
2016 Sep;20(3):181-184. 10.13104/imri.2016.20.3.181.
A Potential Diagnostic Pitfall in the Differentiation of Hemorrhagic and Fatty Lesions Using Short Inversion Time Inversion Recovery: a Case Report
- Affiliations
-
- 1Department of Radiology, Chungbuk National University Hospital, Cheongju, Korea. quartet0@hanmail.net
- 2Department of Radiology, College of Medicine and Medical Research Institute, Chungbuk National University, Cheongju, Korea.
- KMID: 2354799
- DOI: http://doi.org/10.13104/imri.2016.20.3.181
Abstract
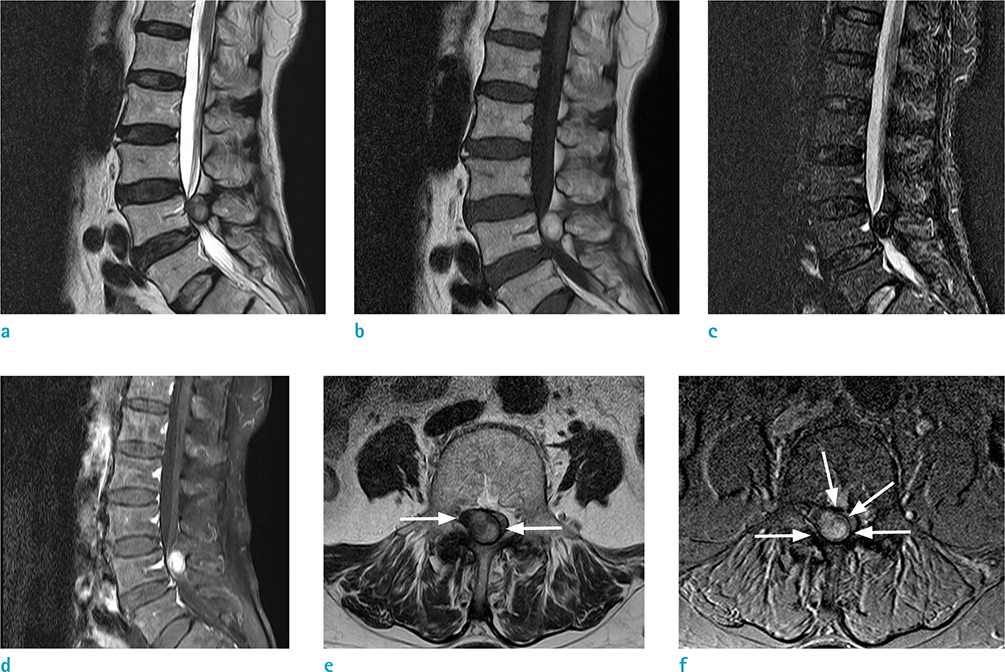
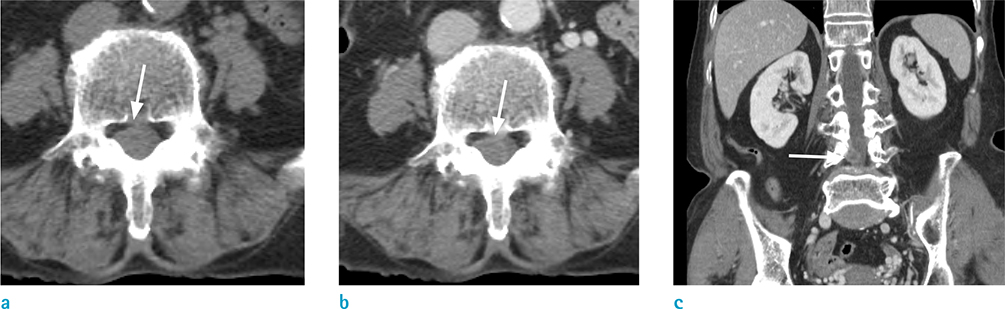
- Short inversion time inversion recovery (STIR) is widely used for spinal magnetic resonance imaging (MRI) because the pulse sequence of STIR is insensitive to magnetic field inhomogeneity and can be used to scan a large field of view. In this case report, we present a case of spinal epidural hematoma with unexpected signal decrease on a STIR image. The MRI showed an epidural mass that appeared with high signal intensity on both T1- and T2-weighted images. However, a signal decrease was encountered on the STIR image. This nonspecific decrease of signal in tissue with a short T1 relaxation time that is similar to that of fat (i.e., hemorrhage) could lead to a diagnostic pitfall; one could falsely diagnose this decrease of signal as fat instead of hemorrhage. Awareness of the nonselective signal suppression achieved with STIR pulse sequences may avert an erroneous diagnosis in image interpretation.
MeSH Terms
Figure
Reference
-
1. Lövblad KO, Baumgartner RW, Zambaz BD, Remonda L, Ozdoba C, Schroth G. Nontraumatic spinal epidural hematomas. MR features. Acta Radiol. 1997; 38:8–13.2. Krinsky G, Rofsky NM, Weinreb JC. Nonspecificity of short inversion time inversion recovery (STIR) as a technique of fat suppression: pitfalls in image interpretation. AJR Am J Roentgenol. 1996; 166:523–526.3. Delfaut EM, Beltran J, Johnson G, Rousseau J, Marchandise X, Cotten A. Fat suppression in MR imaging: techniques and pitfalls. Radiographics. 1999; 19:373–382.4. Bradley WG Jr. MR appearance of hemorrhage in the brain. Radiology. 1993; 189:15–26.5. Froehlich JM, Metens T, Chilla B, Hauser N, Hohl MK, Kubik-Huch RA. MRI of the female pelvis: a possible pitfall in the differentiation of haemorrhagic vs. fatty lesions using fat saturated sequences with inversion recovery. Eur J Radiol. 2012; 81:598–602.6. Khaladkar SM, Kamal A, Kamal V, Kumar S, Singh G, Kalra R. Pitfall in differentiation of hemorrhagic vs. fatty lesions in female pelvis using fat saturated sequences with inversion recovery - role of T1 FATSAT sequence - a case report with radiological review. IOSR-JDM. 2015; 14:86–90.7. Lee YS, Kwon ST, Kim JO, Choi ES. Serial MR imaging of intramuscular hematoma: experimental study in a rat model with the pathologic correlation. Korean J Radiol. 2011; 12:66–77.8. Wu J, Lu L-Q, Gu J-P, Yin X-D. The application of fat-suppression MR pulse sequence in the diagnosis of bone-joint disease. Int J Med Phys, Clin Eng and Radiat Onco. 2012; 1:88–94.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- T1-, T2-weighted, and FLAIR Imaging: Clinical Application
- Spontaneous Restoration of Unrecognized Uterine Inversion
- Replacement of Uterine Inversion by the Induction of General Anesthesia: A case report
- Incidence and Karyotypes According to Each Chromosome in 13 Cases with Inversion
- Usefulness of Combined Fat- and Fluid-Suppressed SPIR-FLAIR Images in Optic Neuritis: Comparison with Fat-Suppressed SPIR or STIR Images or STIR images