J Dent Anesth Pain Med.
2016 Sep;16(3):185-191. 10.17245/jdapm.2016.16.3.185.
Effects of airway evaluation parameters on the laryngeal view grade in mandibular prognathism and retrognathism patients
- Affiliations
-
- 1Department of Dental Anesthesiology, Seoul National University Dental Hospital, Seoul, Korea. stone90@snu.ac.kr
- 2Department of Anesthesiology and Pain Medicine, Seoul National University, College of Medicine, Seoul, Korea.
- 3Division of Oral and Maxillofacial Surgery, Department of Dentistry, College of Medicine, Hanyang University, Seoul, Korea.
- KMID: 2354653
- DOI: http://doi.org/10.17245/jdapm.2016.16.3.185
Abstract
- BACKGROUND
Failure to maintain a patent airway can result in brain damage or death. In patients with mandibular prognathism or retrognathism, intubation is generally thought to be difficult. We determined the degree of difficulty of airway management in patients with mandibular deformity using anatomic criteria to define and grade difficulty of endotracheal intubation with direct laryngoscopy.
METHODS
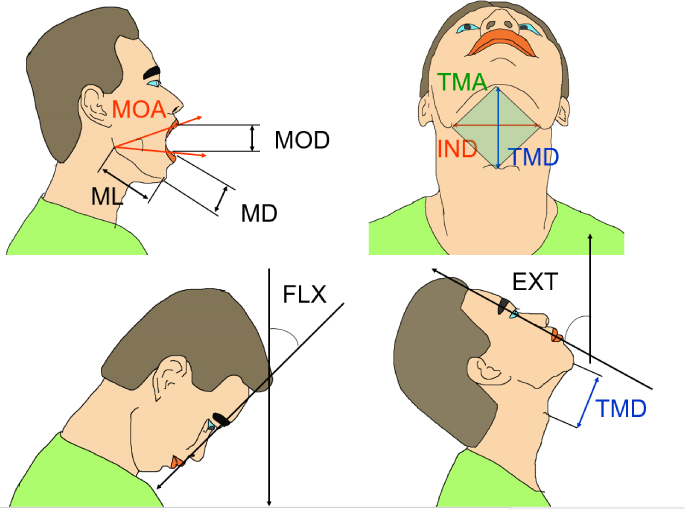
Measurements were performed on 133 patients with prognathism and 33 with retrognathism scheduled for corrective esthetic surgery. A case study was performed on 89 patients with a normal mandible as the control group. In all patients, mouth opening distance (MOD), mandibular depth (MD), mandibular length (ML), mouth opening angle (MOA), neck extension angle (EXT), neck flexion angle (FLX), thyromental distance (TMD), inter-notch distance (IND), thyromental area (TMA), Mallampati grade, and Cormack and Lehane grade were measured.
RESULTS
Cormack and Lehane grade I was observed in 84.2%, grade II in 15.0%, and grade III in 0.8% of mandibular prognathism cases; among retrognathism cases, 45.4% were grade I, 27.3% grade II, and 27.3% grade III; among controls, 65.2% were grade I, 26.9% were grade II, and 7.9% were grade III. MOD, MOA, ML, TMD, and TMA were greater in the prognathism group than in the control and retrognathism groups (P < 0.05). The measurements of ML were shorter in retrognathism than in the control and prognathism groups (P < 0.05).
CONCLUSIONS
Laryngoscopic intubation was easier in patients with prognathism than in those with normal mandibles. However, in retrognathism, the laryngeal view grade was poor and the ML was an important factor.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Authors' Reply to Letter to the Editor “Effects of airway evaluation parameters on the laryngeal view grade in mandibular prognathism and retrognathism patients”
Myong-Hwan Karm, Kwang-Suk Seo
J Dent Anesth Pain Med. 2017;17(1):79-80. doi: 10.17245/jdapm.2017.17.1.79.Letter to the Editor: Effects of airway evaluation parameters on the laryngeal view grade in mandibular prognathism and retrognathism patients
Jaegyok Song
J Dent Anesth Pain Med. 2017;17(1):77-78. doi: 10.17245/jdapm.2017.17.1.77.
Reference
-
1. Caplan RA, Posner KL, Ward RJ, Cheney FW. Adverse respiratory events in anesthesia: A closed claims analysis. Anesthesiology. 1990; 72:828–833.
Article2. Krohner RG. Anesthetic considerations and techniques for oral and maxillofacial surgery. Int Anesthesiol Clin. 2003; 41:67–89.
Article3. Schmitt H, Buchfelder M, Radespeil-Troger M, Fahlbusch R. Difficult intubaton in acromegalic patients. Incidence and predictability. Anesthesiology. 2000; 93:110–114.
Article4. Voyagis GS, Kyriakis KP, Dimitriou V, Vrettou I. Value of oropharyngeal mallampati classification in predicting difficult. Eur J Anaesthesiol. 1998; 15:330–334.
Article5. Mallampati SR, Gatt SP, Gugino LD, Desai SP, Waraksa B, Liu PL, et al. A clinical sign to predict difficult tracheal intubation: A prospective. Can Anaesth Soc J. 1985; 32:429–434.6. Frerk CM. Predicting difficult intubation. Anaesthesia. 1991; 46:1005–1008.7. Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Predicting difficult intubation. Br J Anaesth. 1988; 61:211–216.
Article8. Lee A, Fan LTY, Gin T, Karmakar MK, Ngan Kee WD. A systematic review (meta-analysis) of the accuracy of the mallampati. Anesth Analg. 2006; 102:1867–1878.
Article9. Samsoon GL, Young JR. Difficult tracheal intubation: A retrospective study. Anaesthesia. 1987; 42:487–490.
Article10. Lee SJ, Kim HJ, Yum KW. Airway evaluation for endotracheal intubation of mandibular prognathic patient. J Korean Dent Soc Anesthesiol. 2003; 3:28–33.
Article11. Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984; 39:1105–1111.
Article12. Julien F, Biebuyck MB, Phil D. Management of the difficult adult airway. Anaesthesiology. 1991; 75:1087–1110.
Article13. Tiret L, Desmonts JM, Hatton F, Vourc'h G. Complications associated with anaesthesia--a prospective survey in france. Can Anaesth Soc J. 1986; 33:336–344.
Article14. Bavitz JB, Collicott PE. Bilateral mandibular subcondylar fractures contributing to airway obstruction. Int J Oral Maxillofac Surg. 1995; 24:273–275.
Article15. Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Perdicting difficult intubation. Br J Anaesth. 1988; 61:211–216.16. Oates JDL, Macleod AD, Oates PD, Pearsall FJ, Howie JC, Murray GD. Comparison of two methods for predicting difficult intubation. Br J Anaesth. 1991; 66:305–309.17. Tham EJ, Gildersleve CD, Sanders LD, Mapleson WW, Vaughan RS. Effects of posture, phonation and observer on mallampati classification. Br J Anaesth. 1992; 68:32–38.18. Savva D. Prediction of difficult tracheal intubation. Br J Anaesth. 1994; 73:149–153.19. Ochroch EA, Hollander JE, Kush S, Shofer FS, Levitan RM. Assessment of laryngeal view: Percentage of glottic opening score vs cormack and lehane grading. Can J Anaesth. 1999; 46:987–990.
Article20. Katakura N, Umino M, Kubota Y. Morphologic airway changes after mandibular setback osteotomy for prognathism with and without cleft palate. Anesth Pain Control Dent. 1993; 2:22–26.
Article21. Enacar A, Aksoy AU, Sencift Y, Haydar B, Aras K. Changes in hypopharyngeal airway space and in tongue and hyoid bone positions following the surgical correction of mandibular prognathism. Int J Adult Orthodon Orthognath Surg. 1994; 9:285–290.
Article22. Kawamata A, Fujishita M, Ariji Y, Ariji E. Three-dimensional computed tomographic evaluation of morphologic airway changes after mandibular setback osteotomy for prognathism. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 89:278–287.
Article23. Tselnik M, Pogrel MA. Assessment of the pharyngeal airway space after mandibular setback surgery. J Oral Maxillofac Surg. 2000; 58:282–285.
Article24. Singh PK, Prabhakar H. Airway management in a patient with occipital encephalocele with retrognathia and complete bilateral cleft palate. J Anesth. 2008; 22:335–336.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter to the Editor: Effects of airway evaluation parameters on the laryngeal view grade in mandibular prognathism and retrognathism patients
- Authors' Reply to Letter to the Editor “Effects of airway evaluation parameters on the laryngeal view grade in mandibular prognathism and retrognathism patientsâ€
- Skeletal structure of asymmetric mandibular prognathism and retrognathism
- Airway Evaluation for Endotracheal Intubation of Mandibular Prognathic Patient
- Comparison of cranial base morphology between the mandibular prognathism and maxillary retrognathism in skeletal class III patients