Korean J Orthod.
2016 Sep;46(5):323-330. 10.4041/kjod.2016.46.5.323.
Quantitative evaluation of midpalatal suture maturation via fractal analysis
- Affiliations
-
- 1Department of Orthodontics, Dental Research Institute, Pusan National University Dental Hospital, Yangsan, Korea. softid@pusan.ac.kr
- 2Department of Orthodontics, School of Dentistry, Pusan National University, Yangsan, Korea.
- 3Department of Oral and Maxillofacial Surgery, Pusan National University Dental Hospital, School of Dentistry, Pusan National University, Yangsan, Korea.
- 4Institute of Translational Dental Sciences, Pusan National University Dental Hospital, Yangsan, Korea.
- KMID: 2352294
- DOI: http://doi.org/10.4041/kjod.2016.46.5.323
Abstract
OBJECTIVE
The purpose of this study was to determine whether the results of fractal analysis can be used as criteria for midpalatal suture maturation evaluation.
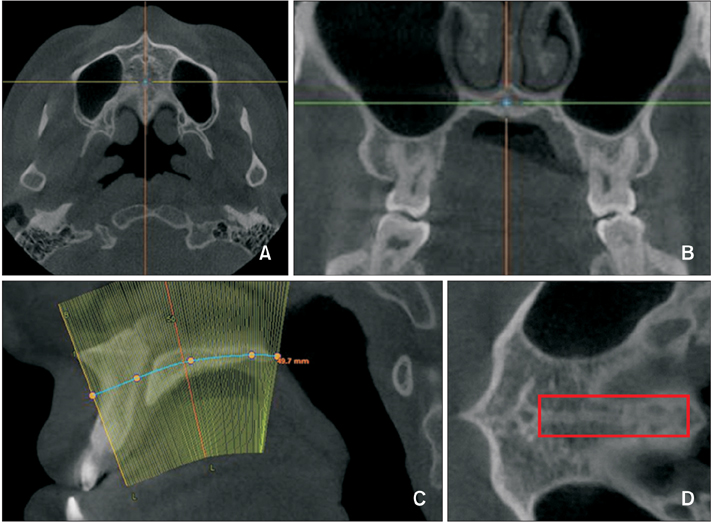
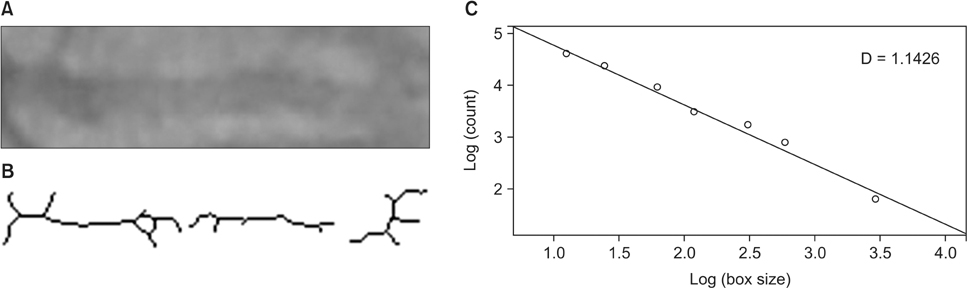
METHODS
The study included 131 subjects aged over 18 years of age (range 18.1-53.4 years) who underwent cone-beam computed tomography. Skeletonized images of the midpalatal suture were obtained via image processing software and used to calculate fractal dimensions. Correlations between maturation stage and fractal dimensions were calculated using Spearman's correlation coefficient. Optimal fractal dimension cut-off values were determined using a receiver operating characteristic curve.
RESULTS
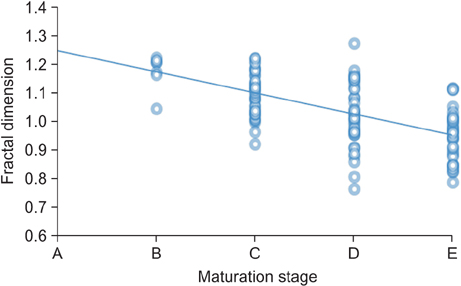
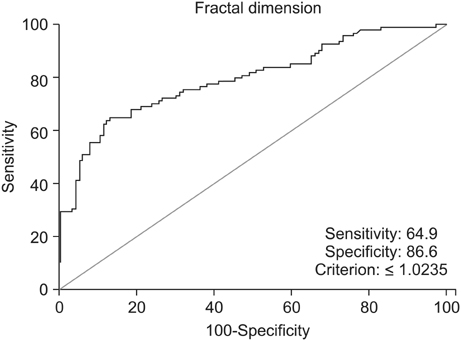
The distribution of maturation stages of the midpalatal suture according to the cervical vertebrae maturation index was highly variable, and there was a strong negative correlation between maturation stage and fractal dimension (−0.623, p < 0.001). Fractal dimension was a statistically significant indicator of dichotomous results with regard to maturation stage (area under curve = 0.794, p < 0.001). A test in which fractal dimension was used to predict the resulting variable that splits maturation stages into ABC and D or E yielded an optimal fractal dimension cut-off value of 1.0235.
CONCLUSIONS
There was a strong negative correlation between fractal dimension and midpalatal suture maturation. Fractal analysis is an objective quantitative method, and therefore we suggest that it may be useful for the evaluation of midpalatal suture maturation.
MeSH Terms
Figure
Cited by 2 articles
-
Relationship between maturation indices and morphology of the midpalatal suture obtained using cone-beam computed tomography images
Hong-Ik Jang, Sang-Cheol Kim, Jong-Moon Chae, Kyung-Hwa Kang, Jin-Woo Cho, Na-Young Chang, Keun-Young Lee, Jin-Hyoung Cho
Korean J Orthod. 2016;46(6):345-355. doi: 10.4041/kjod.2016.46.6.345.Stability of dental, alveolar, and skeletal changes after miniscrew-assisted rapid palatal expansion
Hyun-Mook Lim, Young-Chel Park, Kee-Joon Lee, Kyung-Ho Kim, Yoon Jeong Choi
Korean J Orthod. 2017;47(5):313-322. doi: 10.4041/kjod.2017.47.5.313.
Reference
-
1. Angell EH. Treatment of irregularity of the permanent or adult teeth. Dental Cosmos. 1860; 1:540–544.2. Doruk C, Sökücü O, Sezer H, Canbay EI. Evaluation of nasal airway resistance during rapid maxillary expansion using acoustic rhinometry. Eur J Orthod. 2004; 26:397–401.
Article3. Baldawa RS, Bhad WA. Stress distribution analysis during an intermaxillary dysjunction: A 3-D FEM study of an adult human skull. Ann Maxillofac Surg. 2011; 1:19–25.
Article4. Carmen M, Marcella P, Giuseppe C, Roberto A. Periodontal evaluation in patients undergoing maxillary expansion. J Craniofac Surg. 2000; 11:491–494.
Article5. Koudstaal MJ, Smeets JB, Kleinrensink GJ, Schulten AJ, van der Wal KG. Relapse and stability of surgically assisted rapid maxillary expansion: an anatomic biomechanical study. J Oral Maxillofac Surg. 2009; 67:10–14.
Article6. Lehman JA Jr, Haas AJ. Surgical-orthodontic correction of transverse maxillary deficiency. Dent Clin North Am. 1990; 34:385–395.7. Mehra P, Cottrell DA, Caiazzo A, Lincoln R. Life-threatening, delayed epistaxis after surgically assisted rapid palatal expansion: a case report. J Oral Maxillofac Surg. 1999; 57:201–204.
Article8. Silverstein K, Quinn PD. Surgically-assisted rapid palatal expansion for management of transverse maxillary deficiency. J Oral Maxillofac Surg. 1997; 55:725–727.
Article9. Korn EL, Baumrind S. Transverse development of the human jaws between the ages of 8.5 and 15.5 years, studied longitudinally with use of implants. J Dent Res. 1990; 69:1298–1306.
Article10. Persson M, Thilander B. Palatal suture closure in man from 15 to 35 years of age. Am J Orthod. 1977; 72:42–52.
Article11. Knaup B, Yildizhan F, Wehrbein H. Age-related changes in the midpalatal suture. A histomorphometric study. J Orofac Orthop. 2004; 65:467–474.12. Korbmacher H, Schilling A, Püschel K, Amling M, Kahl-Nieke B. Age-dependent three-dimensional microcomputed tomography analysis of the human midpalatal suture. J Orofac Orthop. 2007; 68:364–376.
Article13. Melsen B. Palatal growth studied on human autopsy material. A histologic microradiographic study. Am J Orthod. 1975; 68:42–54.14. Angelieri F, Cevidanes LH, Franchi L, Gonçalves JR, Benavides E, McNamara JA Jr. Midpalatal suture maturation: classification method for individual assessment before rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2013; 144:759–769.
Article15. Tian Y, Liu F, Sun H, Lv P, Cao Y, Yu M, et al. Alveolar bone thickness around maxillary central incisors of different inclination assessed with conebeam computed tomography. Korean J Orthod. 2015; 45:245–252.
Article16. Yu JC, Wright RL, Williamson MA, Braselton JP 3rd, Abell ML. A fractal analysis of human cranial sutures. Cleft Palate Craniofac J. 2003; 40:409–415.
Article17. Kauffman SA. Part I. 5. Self organization and adaptation in complex systems. In : Kauffman SA, editor. The origins of order: self-organization and selection in evolution. New York: Oxford University Press;1993. p. 173–235.18. Long CA. Intricate sutures as fractal curves. J Morphol. 1985; 185:285–295.
Article19. Russell AP, Thomason JJ. Mechanical analysis of the mammalian head skeleton. In : Hanken J, Hall BK, editors. The skull. Vol. 3. Chicago: University of Chicago Press;1993. p. 345–383.20. Hartwig WC. Fractal analysis of sagittal suture morphology. J Morphol. 1991; 210:289–298.
Article21. White SC, Rudolph DJ. Alterations of the trabecular pattern of the jaws in patients with osteoporosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 88:628–635.
Article22. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174.
Article23. Mommaerts MY. Transpalatal distraction as a method of maxillary expansion. Br J Oral Maxillofac Surg. 1999; 37:268–272.
Article24. Alpern MC, Yurosko JJ. Rapid palatal expansion in adults with and without surgery. Angle Orthod. 1987; 57:245–263.25. Capelozza Filho L, Cardoso Neto J, da Silva Filho OG, Ursi WJ. Non-surgically assisted rapid maxillary expansion in adults. Int J Adult Orthodon Orthognath Surg. 1996; 11:57–66.26. Sánchez I, Uzcátegui G. Fractals in dentistry. J Dent. 2011; 39:273–292.
Article27. Lee RL, Dacre JE, James MF. Image processing assessment of femoral osteopenia. J Digit Imaging. 1997; 10:3 Suppl 1. 218–221.
Article28. Majumdar S, Lin J, Link T, et al. Fractal analysis of radiographs: assessment of trabecular bone structure and prediction of elastic modulus and strength. Med Phys. 1999; 26:1330–1340.
Article29. Southard TE, Southard KA, Jakobsen JR, Hillis SL, Najim CA. Fractal dimension in radiographic analysis of alveolar process bone. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996; 82:569–576.
Article30. Geraets WG, van der Stelt PF. Fractal properties of bone. Dentomaxillofac Radiol. 2000; 29:144–153.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of Midpalatal Suture Maturation by Skeletal Maturity on Hand Wrist Radiographs
- Evaluation of the Midpalatal Suture Maturation in Young Koreans Using Cone-Beam Computed Tomography
- Evaluation of Midpalatal Suture Maturation using Cone-Beam Computed Tomography in Children and Adolescents
- An experimental study on gross reactions of surrounding maxillary sutures to the widening of midpalatal suture in the dog
- Relationship between maturation indices and morphology of the midpalatal suture obtained using cone-beam computed tomography images