J Bone Metab.
2016 Aug;23(3):175-182. 10.11005/jbm.2016.23.3.175.
Proximal Femoral Geometry as Fracture Risk Factor in Female Patients with Osteoporotic Hip Fracture
- Affiliations
-
- 1Department of Orthopeadics, Ajou University School of Medicine, Suwon, Korea.
- 2Department of Orthopaedics, Cheil General Hospital and Women's Healthcare Center, Dankook University College of Medicine, Cheonan, Korea. mhhahn@unitel.co.kr
- KMID: 2350814
- DOI: http://doi.org/10.11005/jbm.2016.23.3.175
Abstract
- BACKGROUND
Proximal femoral geometry may be a risk factor of osteoporotic hip fractures. However, there existed great differences among studies depending on race, sex and age of subjects. The purpose of the present study is to analyze proximal femoral geometry and bone mineral density (BMD) in the osteoporotic hip fracture patients. Furthermore, we investigated proximal femoral geometric parameters affecting fractures, and whether the geometric parameters could be an independent risk factor of fractures regardless of BMD.
METHODS
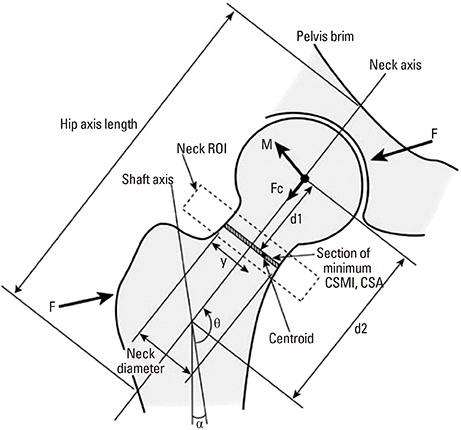
This study was conducted on 197 women aged 65 years or more who were hospitalized with osteoporotic hip fracture (femur neck fractures ; 84, intertrochanteric fractures; 113). Control group included 551 women who visited to check osteoporosis. Femur BMD and proximal femoral geometry for all subjects were measured using dual energy X-ray absorptiometry (DXA), and compared between the control and fracture groups. Besides, proximal femoral geometric parameters associated with fractures were statistically analyzed.
RESULTS
There were statistically significant differences in the age and weight, cross-sectional area (CSA)/length/width of the femoral neck and BMD of the proximal femur between fracture group and control group. BMD of the proximal femur in the control group was higher than in the fracture group. For the femoral neck fractures group, the odds ratio (OR) for fractures decrease in the CSA and neck length (NL) of the femur increased by 1.97 times and 1.73 times respectively, regardless of BMD. The OR for fractures increase in the femoral neck width increased by 1.53 times. In the intertrochanteric fracture group, the OR for fractures increase in the femoral neck width increased by 1.45 times regardless of BMD.
CONCLUSIONS
We found that an increase of the femoral neck width could be a proximal femoral geometric parameter which plays important roles as a risk factor for fracture independently of BMD.
MeSH Terms
Figure
Reference
-
1. Ström O, Borgström F, Kanis JA, et al. Osteoporosis: burden, health care provision and opportunities in the EU: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2011; 6:59–155.
Article2. Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002; 359:1761–1767.
Article3. Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006; 17:1726–1733.
Article4. Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997; 7:407–413.
Article5. Fox KM, Magaziner J, Hebel JR, et al. Intertrochanteric versus femoral neck hip fractures: differential characteristics, treatment, and sequelae. J Gerontol A Biol Sci Med Sci. 1999; 54:M635–M640.
Article6. Svejme O, Ahlborg HG, Nilsson JÅ, et al. Low BMD is an independent predictor of fracture and early menopause of mortality in post-menopausal women--a 34-year prospective study. Maturitas. 2013; 74:341–345.
Article7. Johnell O, Kanis JA, Oden A, et al. Predictive value of BMD for hip and other fractures. J Bone Miner Res. 2005; 20:1185–1194.
Article8. Faulkner KG, Cummings SR, Black D, et al. Simple measurement of femoral geometry predicts hip fracture: the study of osteoporotic fractures. J Bone Miner Res. 1993; 8:1211–1217.
Article9. Yoshikawa T, Turner CH, Peacock M, et al. Geometric structure of the femoral neck measured using dual-energy x-ray absorptiometry. J Bone Miner Res. 1994; 9:1053–1064.
Article10. Beck TJ. Extending DXA beyond bone mineral density: understanding hip structure analysis. Curr Osteoporos Rep. 2007; 5:49–55.
Article11. LaCroix AZ, Beck TJ, Cauley JA, et al. Hip structural geometry and incidence of hip fracture in postmenopausal women: what does it add to conventional bone mineral density? Osteoporos Int. 2010; 21:919–929.
Article12. Kim KM, Brown JK, Kim KJ, et al. Differences in femoral neck geometry associated with age and ethnicity. Osteoporos Int. 2011; 22:2165–2174.
Article13. Cummings SR, Cauley JA, Palermo L, et al. Racial differences in hip axis lengths might explain racial differences in rates of hip fracture. Study of Osteoporotic Fractures Research Group. Osteoporos Int. 1994; 4:226–229.
Article14. Cheng SY, Levy AR, Lefaivre KA, et al. Geographic trends in incidence of hip fractures: a comprehensive literature review. Osteoporos Int. 2011; 22:2575–2586.
Article15. Cooper C, Cole ZA, Holroyd CR, et al. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int. 2011; 22:1277–1288.
Article16. Nelson DA, Beck TJ, Wu G, et al. Ethnic differences in femur geometry in the women's health initiative observational study. Osteoporos Int. 2011; 22:1377–1388.
Article17. Im GI, Lim MJ. Proximal hip geometry and hip fracture risk assessment in a Korean population. Osteoporos Int. 2011; 22:803–807.
Article18. Li Y, Lin J, Cai S, et al. Influence of bone mineral density and hip geometry on the different types of hip fracture. Bosn J Basic Med Sci. 2016; 16:35–38.
Article19. Pulkkinen P, Eckstein F, Lochmuller EM, et al. Association of geometric factors and failure load level with the distribution of cervical vs. trochanteric hip fractures. J Bone Miner Res. 2006; 21:895–901.
Article20. Duboeuf F, Hans D, Schott AM, et al. Different morphometric and densitometric parameters predict cervical and trochanteric hip fracture: the EPIDOS Study. J Bone Miner Res. 1997; 12:1895–1902.
Article21. Maeda Y, Sugano N, Saito M, et al. Comparison of femoral morphology and bone mineral density between femoral neck fractures and trochanteric fractures. Clin Orthop Relat Res. 2011; 469:884–889.
Article22. Panula J, Sävelä M, Jaatinen PT, et al. The impact of proximal femur geometry on fracture type--a comparison between cervical and trochanteric fractures with two parameters. Scand J Surg. 2008; 97:266–271.
Article23. Compston JE, Flahive J, Hosmer DW, et al. Relationship of weight, height, and body mass index with fracture risk at different sites in postmenopausal women: the Global Longitudinal study of Osteoporosis in Women (GLOW). J Bone Miner Res. 2014; 29:487–493.
Article24. Broy SB, Cauley JA, Lewiecki ME, et al. Fracture risk prediction by non-BMD DXA measures: the 2015 ISCD official positions part 1: hip geometry. J Clin Densitom. 2015; 18:287–308.
Article25. Frisoli A Jr., Paula AP, Pinheiro M, et al. Hip axis length as an independent risk factor for hip fracture independently of femural bone mineral density in Caucasian elderly Brazilian women. Bone. 2005; 37:871–875.
Article26. Faulkner KG, Wacker WK, Barden HS, et al. Femur strength index predicts hip fracture independent of bone density and hip axis length. Osteoporos Int. 2006; 17:593–599.
Article27. Iolascon G, Moretti A, Cannaviello G, et al. Proximal femur geometry assessed by hip structural analysis in hip fracture in women. Aging Clin Exp Res. 2015; 27:Suppl 1. S17–S21.
Article28. Leslie WD, Lix LM, Morin SN, et al. Adjusting hip fracture probability in men and women using hip axis length: the manitoba bone density database. J Clin Densitom. 2016; 19:326–331.
Article29. Leslie WD, Lix LM, Morin SN, et al. Hip axis length is a FRAX- and bone density-independent risk factor for hip fracture in women. J Clin Endocrinol Metab. 2015; 100:2063–2070.
Article30. Kaptoge S, Dalzell N, Loveridge N, et al. Effects of gender, anthropometric variables, and aging on the evolution of hip strength in men and women aged over 65. Bone. 2003; 32:561–570.
Article31. Gnudi S, Sitta E, Pignotti E. Prediction of incident hip fracture by femoral neck bone mineral density and neck-shaft angle: a 5-year longitudinal study in post-menopausal females. Br J Radiol. 2012; 85:e467–e473.
Article32. Gnudi S, Ripamonti C, Lisi L, et al. Proximal femur geometry to detect and distinguish femoral neck fractures from trochanteric fractures in postmenopausal women. Osteoporos Int. 2002; 13:69–73.
Article33. El-Kaissi S, Pasco JA, Henry MJ, et al. Femoral neck geometry and hip fracture risk: the Geelong osteoporosis study. Osteoporos Int. 2005; 16:1299–1303.
Article34. Gregory JS, Aspden RM. Femoral geometry as a risk factor for osteoporotic hip fracture in men and women. Med Eng Phys. 2008; 30:1275–1286.
Article35. Peacock M, Buckwalter KA, Persohn S, et al. Race and sex differences in bone mineral density and geometry at the femur. Bone. 2009; 45:218–225.
Article36. Wang MC, Aguirre M, Bhudhikanok GS, et al. Bone mass and hip axis length in healthy Asian, black, Hispanic, and white American youths. J Bone Miner Res. 1997; 12:1922–1935.
Article37. Yan L, Crabtree NJ, Reeve J, et al. Does hip strength analysis explain the lower incidence of hip fracture in the People’s Republic of China? Bone. 2004; 34:584–588.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Osteoporotic Hip Fracture: How We Make Better Results?
- Prediction of Risk Factors in Hip Fractures from Simple Radiographic Measurements of the Proximal Femur
- Clinical Efficacy of Korean FRAX(R) Model in Patients with Hip Fracture
- Femoral Fracture in Non-Cemented hip Arthroplasty
- Periprosthetic Femoral Fractures after Hip Arthroplasty