Ann Surg Treat Res.
2016 Sep;91(3):133-138. 10.4174/astr.2016.91.3.133.
Evaluation of postoperative lymphocele according to amounts and symptoms by using 3-dimensional CT volumetry in kidney transplant recipients
- Affiliations
-
- 1Department of Surgery, Korea University Anam Hospital, Seoul, Korea. cwjung@korea.ac.kr
- 2Department of Radiology, Korea University Anam Hospital, Seoul, Korea.
- 3Department of Internal Medicine, Korea University Anam Hospital, Seoul, Korea.
- 4Department of Surgery, Korea University College of Medicine, Seoul, Korea.
- KMID: 2350540
- DOI: http://doi.org/10.4174/astr.2016.91.3.133
Abstract
- PURPOSE
To analyze the risk factors for postoperative lymphocele, for predicting and preventing complications.
METHODS
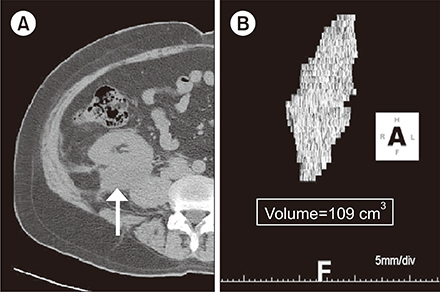
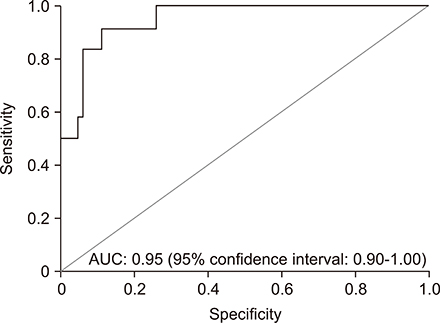
We evaluated 92 kidney transplant recipients with multidetector CT (MDCT) at 1-month posttransplantation. From admission and 1-month postoperative records, data including diabetes, dialysis type, immunosuppressant use, steroid pulse therapy, and transplantation side were collected. Lymphocele volume was measured with 3-dimensional reconstructed, nonenhanced MDCT at one month postoperatively. The correlations between risk factors and lymphocele volume and between risk factors and symptomatic lymphocele (SyL) were analyzed. The cutoff was calculated by using the receiver operating characteristic (ROC) curve for SyL volume.
RESULTS
Among 92 recipients, the mean volume was 44.53 ± 176.43 cm³ and 12 had SyL. Univariable analysis between risk factors and lymphocele volume indicated that donor age, retransplantation, and inferiorly located lymphocele were statistically significant. The ROC curve for SyL showed that 33.20 cm³ was the cutoff, with 83.3% sensitivity and 93.7% specificity. On univariable analysis between risk factors and SyL, steroid pulse, inferiorly located lymphocele, and >33.20 cm³ were statistically significant. Multivariable analysis indicated that steroid pulse, >33.20 cm³, and serum creatinine level at one month were significant factors.
CONCLUSION
Risk factors including donor age, retransplantation, steroid pulse therapy, and inferiorly located lymphocele are important predictors of large lymphoceles or SyL. In high-risk recipients, careful monitoring of renal function and early image surveillance such as CT or ultrasound are recommended. If the asymptomatic lymphocele is >33.20 cm³ or located inferiorly, early interventions can be considered while carefully observing the changes in symptoms.
Keyword
MeSH Terms
Figure
Reference
-
1. Zietek Z, Sulikowski T, Tejchman K, Sienko J, Janeczek M, Iwan-Zietek I, et al. Lymphocele after kidney transplantation. Transplant Proc. 2007; 39:2744–2747.2. Ebadzadeh MR, Tavakkoli M. Lymphocele after kidney transplantation: where are we standing now? Urol J. 2008; 5:144–148.3. Ulrich F, Niedzwiecki S, Fikatas P, Nebrig M, Schmidt SC, Kohler S, et al. Symptomatic lymphoceles after kidney transplantation - multivariate analysis of risk factors and outcome after laparoscopic fenestration. Clin Transplant. 2010; 24:273–280.4. Thompson TJ, Neale TJ. Acute perirenal lymphocele formation 8 years after renal transplantation. Aust N Z J Surg. 1989; 59:583–585.5. Chajes V, Biessy C, Ferrari P, Romieu I, Freisling H, Huybrechts I, et al. Plasma elaidic acid level as biomarker of industrial trans fatty acids and risk of weight change: report from the EPIC study. PLoS One. 2015; 10:e0118206.6. Zagdoun E, Ficheux M, Lobbedez T, Chatelet V, Thuillier-Lecouf A, Bensadoun H, et al. Complicated lymphoceles after kidney transplantation. Transplant Proc. 2010; 42:4322–4325.7. Gomes AS, Scholl D, Feinberg S, Simmons RL, Amplatz K. Lymphangiography and ultrasound in management of lymphoceles. Urology. 1979; 13:104–108.8. Sollinger HW, Starling JR, Oberley T, Glass NR, Belzer FO. Severe “weeping” kidney disease after transplantation: a case report. Transplant Proc. 1983; 15:2157–2160.9. Chedid MF, Muthu C, Nyberg SL, Lesnick TG, Kremers WK, Prieto M, et al. Living donor kidney transplantation using laparoscopically procured multiple renal artery kidneys and right kidneys. J Am Coll Surg. 2013; 217:144–152.10. Singh D, Lawen J, Alkhudair W. Does pretransplant obesity affect the outcome in kidney transplant recipients? Transplant Proc. 2005; 37:717–720.11. Khauli RB, Stoff JS, Lovewell T, Ghavamian R, Baker S. Post-transplant lymphoceles: a critical look into the risk factors, pathophysiology and management. J Urol. 1993; 150:22–26.12. Nashan B, Citterio F. Wound healing complications and the use of mammalian target of rapamycin inhibitors in kidney transplantation: a critical review of the literature. Transplantation. 2012; 94:547–561.13. Adani GL, Baccarani U, Bresadola V, Lorenzin D, Montanaro D, Risaliti A, et al. Graft loss due to percutaneous sclerotherapy of a lymphocele using acetic acid after renal transplantation. Cardiovasc Intervent Radiol. 2005; 28:836–838.14. Giuliani S, Gamba P, Kiblawi R, Midrio P, Ghirardo G, Zanon GF. Lymphocele after pediatric kidney transplantation: incidence and risk factors. Pediatr Transplant. 2014; 18:720–725.15. Krol R, Kolonko A, Chudek J, Ziaja J, Pawlicki J, Mały A, et al. Did volume of lymphocele after kidney transplantation determine the choice of treatment modality? Transplant Proc. 2007; 39:2740–2743.16. Abou-Elela A, Reyad I, Torky M, Meshref A, Morsi A. Laparoscopic marsupialization of postrenal transplantation lymphoceles. J Endourol. 2006; 20:904–909.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnostic performance of multidetector computed tomography for symptomatic lymphoceles in kidney transplant recipients
- Lymphocele Presenting by Scrotal Swelling after Kidney Transplantation
- Laparoscopic Intraperitoneal Drainage of Lymphocele Developed Adjacent to the Kidney Transplanted
- A Concept Analysis of Compliance in Kidney Transplant Recipient Including Compliance with Immunosuppressive Medication
- Liver Regeneration and Factors Influencing Liver Regeneration in Donors and Recipients of Adult Living Donor Liver Transplantation Using Right Lobe Graft