Allergy Asthma Immunol Res.
2016 Nov;8(6):499-504. 10.4168/aair.2016.8.6.499.
Factors Affecting Recovery Time of Pulmonary Function in Hospitalized Patients With Acute Asthma Exacerbations
- Affiliations
-
- 1Department of Allergy and Clinical Immunology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. yscho@amc.seoul.kr
- KMID: 2349989
- DOI: http://doi.org/10.4168/aair.2016.8.6.499
Abstract
- PURPOSE
Prolonged recovery time of pulmonary function after an asthma exacerbation is a significant burden on asthmatics, and management of these patients needs to be improved. The aim of this study was to evaluate factors associated with a longer recovery time of pulmonary function among asthmatic patients hospitalized due to a severe asthma exacerbation.
METHODS
We retrospectively reviewed the medical records of 89 patients who were admitted for the management of acute asthma exacerbations. The recovery time of pulmonary function was defined as the time from the date each patient initially received treatment for asthma exacerbations to the date the patient reached his or her previous best FEV1% value. We investigated the influence of various clinical and laboratory factors on the recovery time.
RESULTS
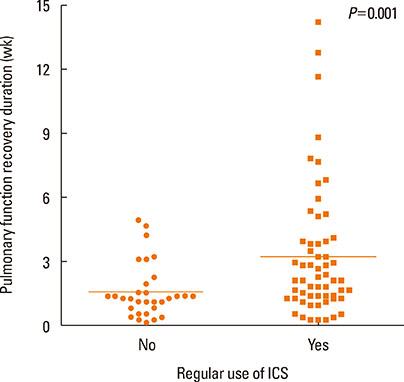
The median recovery time of the patients was 1.7 weeks. Multiple linear regression analysis revealed that using regular inhaled corticosteroids (ICS) before an acute exacerbation of asthma and concurrent with viral infection at admission were associated with the prolonged recovery time of pulmonary function.
CONCLUSIONS
The prolonged recovery time of pulmonary function after a severe asthma exacerbation was not shown to be directly associated with poor adherence to ICS. Therefore the results indicate that an unknown subtype of asthma may be associated with the prolonged recovery of pulmonary function time after an acute exacerbation of asthma despite regular ICS use. Further prospective studies to investigate factors affecting the recovery time of pulmonary function after an asthma exacerbation are warranted.
MeSH Terms
Figure
Reference
-
1. Global Initiative for Asthma. Global strategy for asthma management and prevention [Internet]. place unknown: Global Initiative for Asthma;2014. updated 2015 Aug 12. cited 2015 Nov 25. Available from: http://www.ginasthma.org/.2. Ye YM, Kim SH, Hur GY, Kim JH, Park JW, Shim JJ, et al. Addition of montelukast to low-dose inhaled corticosteroid leads to fewer exacerbations in older patients than medium-dose inhaled corticosteroid monotherapy. Allergy Asthma Immunol Res. 2015; 7:440–448.3. Rodrigo GJ, Rodrigo C, Hall JB. Acute asthma in adults: a review. Chest. 2004; 125:1081–1102.4. Martinez FD, Vercelli D. Asthma. Lancet. 2013; 382:1360–1372.5. O'Byrne PM, Pedersen S, Lamm CJ, Tan WC, Busse WW. START Investigators Group. Severe exacerbations and decline in lung function in asthma. Am J Respir Crit Care Med. 2009; 179:19–24.6. Song WJ, Cho SH. Challenges in the management of asthma in the elderly. Allergy Asthma Immunol Res. 2015; 7:431–439.7. Guilbert TW, Denlinger LC. Role of infection in the development and exacerbation of asthma. Expert Rev Respir Med. 2010; 4:71–83.8. Cohn L, Woodruff PG. Update in asthma 2013. Am J Respir Crit Care Med. 2014; 189:1487–1493.9. Donahue JG, Weiss ST, Livingston JM, Goetsch MA, Greineder DK, Platt R. Inhaled steroids and the risk of hospitalization for asthma. JAMA. 1997; 277:887–891.10. Debley JS, Cochrane ES, Redding GJ, Carter ER. Lung function and biomarkers of airway inflammation during and after hospitalization for acute exacerbations of childhood asthma associated with viral respiratory symptoms. Ann Allergy Asthma Immunol. 2012; 109:114–120.11. Peters SP, Ferguson G, Deniz Y, Reisner C. Uncontrolled asthma: a review of the prevalence, disease burden and options for treatment. Respir Med. 2006; 100:1139–1151.12. Racusin DA, Fox KA, Ramin SM. Severe acute asthma. Semin Perinatol. 2013; 37:234–245.13. Szefler SJ, Martin RJ, King TS, Boushey HA, Cherniack RM, Chinchilli VM, et al. Significant variability in response to inhaled corticosteroids for persistent asthma. J Allergy Clin Immunol. 2002; 109:410–418.14. Martin RJ, Szefler SJ, King TS, Kraft M, Boushey HA, Chinchilli VM, et al. The predicting response to inhaled corticosteroid efficacy (PRICE) trial. J Allergy Clin Immunol. 2007; 119:73–80.15. Yilmaz O, Bakirtas A, Ertoy Karagol HI, Topal E, Demirsoy MS. Allergic rhinitis may impact the recovery of pulmonary function tests after moderate/severe asthma exacerbation in children. Allergy. 2014; 69:652–657.16. Jenkins PF, Benfield GF, Smith AP. Predicting recovery from acute severe asthma. Thorax. 1981; 36:835–841.17. Holt PG, Strickland DH. Interactions between innate and adaptive immunity in asthma pathogenesis: new perspectives from studies on acute exacerbations. J Allergy Clin Immunol. 2010; 125:963–972.18. Schwartz HJ, Lowell FC, Melby JC. Steroid resistance in bronchial asthma. Ann Intern Med. 1968; 69:493–499.19. Cohen L, E X, Tarsi J, Ramkumar T, Horiuchi TK, Cochran R, et al. Epithelial cell proliferation contributes to airway remodeling in severe asthma. Am J Respir Crit Care Med. 2007; 176:138–145.20. Greenberg S. Asthma exacerbations: predisposing factors and prediction rules. Curr Opin Allergy Clin Immunol. 2013; 13:225–236.21. Matsumoto K, Inoue H. Viral infections in asthma and COPD. Respir Investig. 2014; 52:92–100.22. Silva RC, Couceiro JN, Câmara FP, Valle S, Santos N. Asthma exacerbation and viral infection in adult patients, Brazil. Braz J Infect Dis. 2015; 19:446–448.23. Chang AB, Clark R, Acworth JP, Petsky HL, Sloots TP. The impact of viral respiratory infection on the severity and recovery from an asthma exacerbation. Pediatr Infect Dis J. 2009; 28:290–294.24. Rueter K, Bizzintino J, Martin AC, Zhang G, Hayden CM, Geelhoed GC, et al. Symptomatic viral infection is associated with impaired response to treatment in children with acute asthma. J Pediatr. 2012; 160:82–87.25. Arden KE, Chang AB, Lambert SB, Nissen MD, Sloots TP, Mackay IM. Newly identified respiratory viruses in children with asthma exacerbation not requiring admission to hospital. J Med Virol. 2010; 82:1458–1461.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Factors Affecting Recovery Time of Pulmonary Function in Hospitalized Patients With Acute Asthma Exacerbations
- Seasonality of asthma exacerbation in children caused by respiratory virus infection and allergen sensitization
- Factors Predicting Recovery From Asthma Exacerbations
- New Tread of Association of Rhinovirus and Asthma
- Effect of influenza vaccine on pulmonary function in stable asthma