J Korean Ophthalmol Soc.
2016 Aug;57(8):1193-1198. 10.3341/jkos.2016.57.8.1193.
Comparison of Results and Complications between 0.64 mm and 0.94 mm Silicone Tube Intubation in Adults
- Affiliations
-
- 1Department of Ophthalmology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea. jhahn77@hanmail.net
- 2Department of Ophthalmology, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea.
- KMID: 2349062
- DOI: http://doi.org/10.3341/jkos.2016.57.8.1193
Abstract
- PURPOSE
To compare surgical success rates and complications of silicone tube intubation using 0.64-mm- and 0.94-mm-diameter tubes in adult patients with nasolacrimal duct stenosis.
METHODS
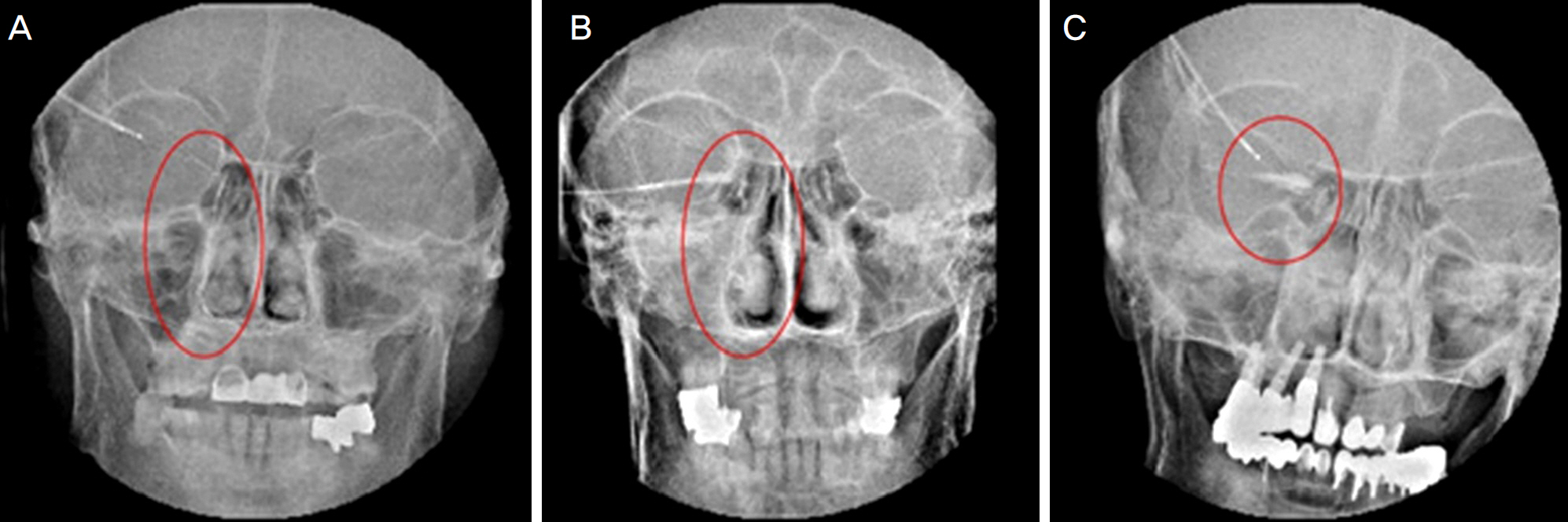
In 62 eyes of 36 patients diagnosed with nasolacrimal duct stenosis who had undergone silicone tube intubation, we surveyed sex, age, symptom duration, time of tube removal, mean follow-up period, and surgical success rate between two groups divided by silicone tube diameter, 0.64 mm and 0.94 mm. By preoperative syringing test and dacryocystography, we examined the surgical results and complications of the two groups.
RESULTS
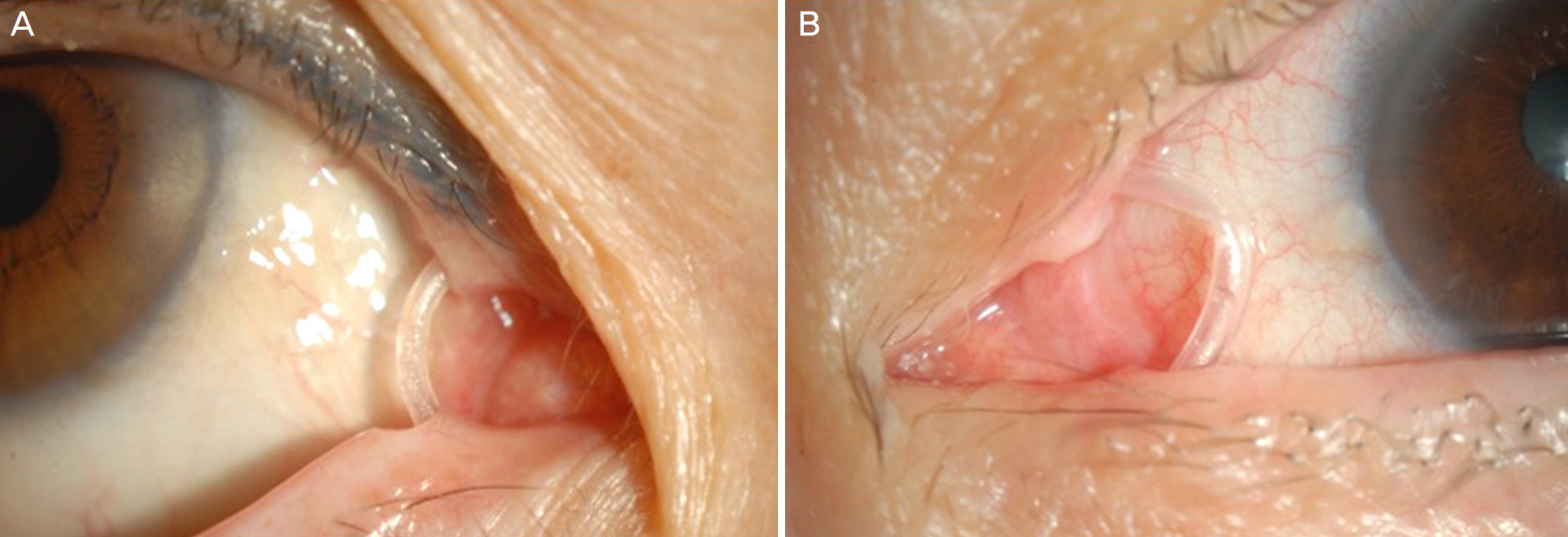
The silicone tube diameter was 0.64 mm in 43 eyes (69.4%) and 0.94 mm in 19 eyes (30.2%). The surgical success rates in the two groups were 84.1% (36 eyes) and 78.9% (15 eyes), respectively, but the difference was not significant statistically. The surgical success rate was higher in partial stenosis than in complete stenosis but was not different according to silicone tube diameter according to preoperative syringing test and dacryocystography. Silicone tube disconnection and bending were only observed in 0.94-mm-diameter silicone tubes.
CONCLUSIONS
In silicone tube intubation for nasolacrimal duct stenosis in adults, silicone tube diameter does not affect operation success. However, silicone tube disconnection and bending were observed only in the 0.94 mm silicone tube.
MeSH Terms
Figure
Cited by 1 articles
-
Combination Surgery of Silicone Tube Intubation and Conjunctival Resection in Patients with Epiphora
Seon Tae Kim, Long Yu Jin, Hee Bae Ahn
Korean J Ophthalmol. 2018;32(6):438-444. doi: 10.3341/kjo.2018.0044.
Reference
-
References
1. Oum JS, Park JW, Choi YK, et al. Result of partial nasolacrimal duct obstruction after silicone tube intubation. J Korean Ophthalmol Soc. 2004; 45:1777–82.2. Keith CG. Intubation of the lacrimal passages. Am J Ophthalmol. 1968; 65:70–4.
Article3. Beigi B, O'Keefe M. Results of Crawford tube intubation in children. Acta Ophthalmol (Copenh). 1993; 71:405–7.
Article4. Ewing AE. Roentgen ray demonstration of the lacrimal abscess cavity. Am J Ophthalmol. 1909; 24:1–4.5. Milder B, Demorest BH. Dacryocystography. I. The normal abdominal apparatus. AMA Arch Ophthalmol. 1954; 51:180–95.6. Jung JJ, Jang SY, Jang JW, In JH. Comparison results of silicone tube intubation according to syringing and dacryocystography. J Korean Ophthalmol Soc. 2014; 55:1584–8.
Article7. Park JJ, Shin DS, Hong SP, Lee KW. Effects of double silicone tube intubation for nasolacrimal duct obstruction in adults. J Korean Ophthalmol Soc. 2005; 46:1951–6.8. Moscato EE, Dolmetsch AM, Silkiss RZ, Seiff SR. Silicone abdominal for the treatment of epiphora in adults with presumed functional nasolacrimal duct obstruction. Ophthal Plast Reconstr Surg. 2012; 28:35–9.9. Kwon YH, Lee YJ. abdominal results of silicone tube intubation in incomplete nasolacrimal duct obstruction (NLDO). J Korean Ophthalmol Soc. 2008; 49:190–4.10. Kim YR, Ahn M. Long term effect of double silicone tube abdominal for acquired nasolacrimal duct obstruction. J Korean Ophthalmol Soc. 2012; 53:1554–8.11. Kashkouli MB, Kempster RC, Galloway GD, Beigi B. Monocanalicular versus bicanalicular silicone intubation for nasolacrimal duct stenosis in adults. Ophthal Plast Reconstr Surg. 2005; 21:142–7.
Article12. Andalib D, Nabie R, Abbasi L. Silicone intubation for nasolacrimal duct stenosis in adults: monocanalicular or bicanalicular intubation. J Craniofac Surg. 2014; 25:1009–11.13. Tucker SM, Linberg JV, Nguyen LL, et al. Measurement of the abdominal to fluid flow within the lacrimal outflow system. Ophthalmology. 1995; 102:1639–45.14. Demirci H, Elner VM. Double silicone tube intubation for the abdominal of partial lacrimal system obstruction. Ophthalmology. 2008; 115:383–5.15. Paik JS, Cho WK, Yang SW. Bicanalicular double silicone stenting in endoscopic dacryocystorhinostomy with lacrimal trephination in distal or common canalicular obstruction. Eur Arch Otorhinolaryngol. 2012; 269:1605–11.
Article16. Hwang SW, Khwarg SI, Kim JH, et al. Bicanalicular double abdominal intubation in external dacryocystorhinostomy and canal-iculoplasty for distal canalicular obstruction. Acta Ophthalmol. 2009; 87:438–42.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tube Position and Culture in the Nasal Cavities of Patients Treated with Silicone Tube Intubation
- Comparison of Dacryocystographic Results Before and After Silicone Intubation in Incomplete Nasolacrimal Duct Obstruction
- Comparison of the Efficacies of 0.94 mm and Double Silicone Tubes for Treatment of Canalicular Obstruction
- The Complications of Silicone Tube Intubation after Lacrimal Surgery
- Silicone Intubation and Dacryocystographic Finding in Incomplete Nasolacrimal Duct Obstruction