Yonsei Med J.
2015 Nov;56(6):1632-1637. 10.3349/ymj.2015.56.6.1632.
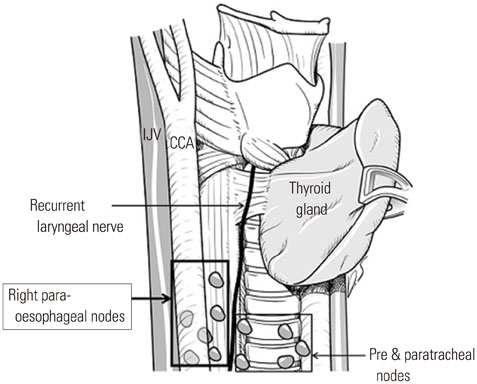
The Clinical Significance of the Right Para-Oesophageal Lymph Nodes in Papillary Thyroid Cancer
- Affiliations
-
- 1Thyroid Cancer Center, Department of Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. surghsc@yuhs.ac
- 2Department of Surgery, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- 3Department of Surgery, Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- KMID: 2345893
- DOI: http://doi.org/10.3349/ymj.2015.56.6.1632
Abstract
- PURPOSE
Although guidelines indicate that routine dissection of the central lymph nodes in patients with thyroid carcinoma should include the right para-oesophageal lymph nodes (RPELNs), located between the right recurrent laryngeal nerve and the cervical oesophagus and posterior to the former, RPELN dissection is often omitted due to high risk of injuries to the recurrent laryngeal nerve and the right inferior parathyroid gland.
MATERIALS AND METHODS
We retrospectively identified all patients diagnosed with papillary thyroid carcinoma who underwent total thyroidectomy with central lymph node dissection, including the RPELNs, between January 1, 2009 and December 31, 2013 at the Thyroid Cancer Center of Yonsei University College of Medicine, Seoul, Korea.
RESULTS
Of 5556 patients, 148 were positive for RPELN metastasis; of the latter, 91 had primary tumours greater than 1 cm (p<0.001). Extrathyroidal extension by the primary tumour (81.8%; p<0.001), bilaterality, and multifocality were more common in patients with than without RPELN metastasis; however, there were no significant differences in age and sex between groups. A total of 95.9% of patients with RPELN metastasis had central node (except right para-oesophageal lymph node) metastasis, and the incidence of lateral neck node metastasis was significantly higher in patients with than without RPELN metastasis (63.5% vs. 14.3%, p<0.001). Forty-one patients underwent mediastinal dissection, with 11 patients confirmed as having mediastinal lymph node metastasis with RPELN metastasis on pathological examination.
CONCLUSION
RPELN metastasis is significantly associated with lateral neck and mediastinal lymph node metastasis.
Keyword
MeSH Terms
-
Adult
Aged
Carcinoma/pathology/*surgery
Carcinoma, Papillary/pathology/*surgery
Esophageal Neoplasms/*secondary/surgery
Female
Humans
Incidence
*Lymph Node Excision
Lymph Nodes/pathology/*surgery
Lymphatic Metastasis/pathology
Male
Middle Aged
Recurrent Laryngeal Nerve/pathology
Republic of Korea/epidemiology
Retrospective Studies
Thyroid Neoplasms/pathology/*surgery
*Thyroidectomy
Treatment Outcome
Young Adult
Figure
Reference
-
1. Davidson HC, Park BJ, Johnson JT. Papillary thyroid cancer: controversies in the management of neck metastasis. Laryngoscope. 2008; 118:2161–2165.2. Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Seo HG, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2009. Cancer Res Treat. 2012; 44:11–24.3. Ahmadi N, Grewal A, Davidson BJ. Patterns of cervical lymph node metastases in primary and recurrent papillary thyroid cancer. J Oncol. 2011; 2011:735678.4. Machens A, Hinze R, Thomusch O, Dralle H. Pattern of nodal metastasis for primary and reoperative thyroid cancer. World J Surg. 2002; 26:22–28.5. Leboulleux S, Rubino C, Baudin E, Caillou B, Hartl DM, Bidart JM, et al. Prognostic factors for persistent or recurrent disease of papillary thyroid carcinoma with neck lymph node metastases and/or tumor extension beyond the thyroid capsule at initial diagnosis. J Clin Endocrinol Metab. 2005; 90:5723–5729.
Article6. Pereira JA, Jimeno J, Miquel J, Iglesias M, Munné A, Sancho JJ, et al. Nodal yield, morbidity, and recurrence after central neck dissection for papillary thyroid carcinoma. Surgery. 2005; 138:1095–1100.
Article7. White ML, Gauger PG, Doherty GM. Central lymph node dissection in differentiated thyroid cancer. World J Surg. 2007; 31:895–904.
Article8. Roh JL, Park JY, Park CI. Total thyroidectomy plus neck dissection in differentiated papillary thyroid carcinoma patients: pattern of nodal metastasis, morbidity, recurrence, and postoperative levels of serum parathyroid hormone. Ann Surg. 2007; 245:604–610.
Article9. Zhang L, Wei WJ, Ji QH, Zhu YX, Wang ZY, Wang Y, et al. Risk factors for neck nodal metastasis in papillary thyroid microcarcinoma: a study of 1066 patients. J Clin Endocrinol Metab. 2012; 97:1250–1257.
Article10. Robbins KT, Clayman G, Levine PA, Medina J, Sessions R, Shaha A, et al. Neck dissection classification update: revisions proposed by the American Head and Neck Society and the American Academy of Otolaryngology-Head and Neck Surgery. Arch Otolaryngol Head Neck Surg. 2002; 128:751–758.11. American Thyroid Association Surgery Working Group. American Association of Endocrine Surgeons. American Academy of Otolaryngology-Head and Neck Surgery. American Head and Neck Society. Carty SE, Cooper DS, et al. Consensus statement on the terminology and classification of central neck dissection for thyroid cancer. Thyroid. 2009; 19:1153–1158.
Article12. Wang TS, Evans DB, Fareau GG, Carroll T, Yen TW. Effect of prophylactic central compartment neck dissection on serum thyroglobulin and recommendations for adjuvant radioactive iodine in patients with differentiated thyroid cancer. Ann Surg Oncol. 2012; 19:4217–4222.
Article13. Grodski S, Cornford L, Sywak M, Sidhu S, Delbridge L. Routine level VI lymph node dissection for papillary thyroid cancer: surgical technique. ANZ J Surg. 2007; 77:203–208.14. Yamashita H, Noguchi S, Murakami N, Kawamoto H, Watanabe S. Extracapsular invasion of lymph node metastasis is an indicator of distant metastasis and poor prognosis in patients with thyroid papillary carcinoma. Cancer. 1997; 80:2268–2272.
Article15. Sugitani I, Kasai N, Fujimoto Y, Yanagisawa A. A novel classification system for patients with PTC: addition of the new variables of large (3 cm or greater) nodal metastases and reclassification during the follow-up period. Surgery. 2004; 135:139–148.
Article16. Lundgren CI, Hall P, Dickman PW, Zedenius J. Clinically significant prognostic factors for differentiated thyroid carcinoma: a population-based, nested case-control study. Cancer. 2006; 106:524–531.17. Gemsenjäger E, Perren A, Seifert B, Schüler G, Schweizer I, Heitz PU. Lymph node surgery in papillary thyroid carcinoma. J Am Coll Surg. 2003; 197:182–190.18. Kim YS, Park WC. Clinical predictors of right upper paraesophageal lymph node metastasis from papillary thyroid carcinoma. World J Surg Oncol. 2012; 10:164.19. Bae SY, Yang JH, Choi MY, Choe JH, Kim JH, Kim JS. Right paraesophageal lymph node dissection in papillary thyroid carcinoma. Ann Surg Oncol. 2012; 19:996–1000.
Article20. Machens A, Hinze R, Lautenschläger C, Thomusch O, Dralle H. Thyroid carcinoma invading the cervicovisceral axis: routes of invasion and clinical implications. Surgery. 2001; 129:23–28.
Article21. Honings J, Stephen AE, Marres HA, Gaissert HA. The management of thyroid carcinoma invading the larynx or trachea. Laryngoscope. 2010; 120:682–689.
Article22. Choi JY, Choi YS, Park YH, Kim JH. Experience and analysis of level VII cervical lymph node metastases in patients with papillary thyroid carcinoma. J Korean Surg Soc. 2011; 80:307–312.23. Machens A, Dralle H. Prediction of mediastinal lymph node metastasis in papillary thyroid cancer. Ann Surg Oncol. 2009; 16:171–176.
Article24. Johner CH, Ranniger K. Mediastinal lymphography. Surg Gynecol Obstet. 1968; 127:1313–1316.25. Rosenbaum MA, McHenry CR. Central neck dissection for papillary thyroid cancer. Arch Otolaryngol Head Neck Surg. 2009; 135:1092–1097.
Article26. Teixeira G, Teixeira T, Gubert F, Chikota H, Tufano R. The incidence of central neck micrometastatic disease in patients with papillary thyroid cancer staged preoperatively and intraoperatively as N0. Surgery. 2011; 150:1161–1167.
Article27. Gonçalves Filho J, Kowalski LP. Surgical complications after thyroid surgery performed in a cancer hospital. Otolaryngol Head Neck Surg. 2005; 132:490–494.
Article28. Rosato L, Avenia N, Bernante P, De Palma M, Gulino G, Nasi PG, et al. Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg. 2004; 28:271–276.
Article29. Lefevre JH, Tresallet C, Leenhardt L, Jublanc C, Chigot JP, Menegaux F. Reoperative surgery for thyroid disease. Langenbecks Arch Surg. 2007; 392:685–691.
Article30. Pezzullo L, Delrio P, Losito NS, Caracò C, Mozzillo N. Post-operative complications after completion thyroidectomy for differentiated thyroid cancer. Eur J Surg Oncol. 1997; 23:215–218.
Article31. Kim MK, Mandel SH, Baloch Z, Livolsi VA, Langer JE, Didonato L, et al. Morbidity following central compartment reoperation for recurrent or persistent thyroid cancer. Arch Otolaryngol Head Neck Surg. 2004; 130:1214–1216.
Article32. Iyer NG, Kumar A, Nixon IJ, Patel SG, Ganly I, Tuttle RM, et al. Incidence and significance of Delphian node metastasis in papillary thyroid cancer. Ann Surg. 2011; 253:988–991.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cystic Lymph Node Metastasis from Thyroid Papillary Microcarcinoma
- Optimal Neck Dissection Extent for Metastatic Lymph Nodes in Papillary Thyroid Cancer
- Papillary Thyroid Cancer Arising in Lateral Aberrant Thyroid Presenting with Multiple Metastases
- Retropharyngeal Lymph Node Metastasis from Thyroid Papillary Carcinoma with Airway Obstruction
- One Case of a Primary Papillary Thyroid Carcinoma in the Intrathoracic Lymph Node