Yonsei Med J.
2015 Nov;56(6):1627-1631. 10.3349/ymj.2015.56.6.1627.
Paralytic Ileus and Prophylactic Gastrointestinal Motility Medication after Spinal Operation
- Affiliations
-
- 1Department of Neurosurgery, Guro Teun Teun Hospital, Seoul, Korea.
- 2Department of Neurosurgery, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Neurosurgery, Inha University College of Medicine, Incheon, Korea. nsyoon@gmail.com
- 4Department of Radiology, Inha University College of Medicine, Incheon, Korea.
- KMID: 2345892
- DOI: http://doi.org/10.3349/ymj.2015.56.6.1627
Abstract
- PURPOSE
To investigate the prevalence of paralytic ileus after spinal operation in the supine or prone operative position and to determine the efficacy of prophylactic gastrointestinal motility medications in preventing symptomatic paralytic ileus after a spinal operation.
MATERIALS AND METHODS
All patients received spinal surgery in the supine or prone operative position. The study period was divided into two phases: first, to analyze the prevalence of radiographic and symptomatic paralytic ileus after a spinal operation, and second, to determine the therapeutic effects of prophylactic gastrointestinal motility medications (postoperative intravenous injection of scopolamine butylbromide and metoclopramide hydrochloride) on symptomatic paralytic ileus after a spinal operation.
RESULTS
Basic demographic data were not different. In the first phase of this study, 27 patients (32.9%) with radiographic paralytic ileus and 11 patients (13.4%) with symptomatic paralytic ileus were observed. Radiographic paralytic ileus was more often noted in patients who underwent an operation in the prone position (p=0.044); whereas the occurrence of symptomatic paralytic ileus was not different between the supine and prone positioned patients (p=0.385). In the second phase, prophylactic medications were shown to be ineffective in preventing symptomatic paralytic ileus after spinal surgery [symptomatic paralytic ileus was observed in 11.1% (4/36) with prophylactic medication and 16.7% (5/30) with a placebo, p=0.513].
CONCLUSION
Spinal surgery in the prone position was shown to increase the likelihood of radiographic paralytic ileus occurrence, but not symptomatic paralytic ileus. Unfortunately, the prophylactic medications to prevent symptomatic paralytic ileus after spine surgery were shown to be ineffective.
Keyword
MeSH Terms
-
Adjuvants, Anesthesia/*administration & dosage/pharmacology
Adult
Aged
Antiemetics/*administration & dosage/pharmacology
Female
Gastrointestinal Motility/*drug effects/physiology
Humans
Injections, Intravenous
Intestinal Pseudo-Obstruction/drug therapy/epidemiology/*prevention & control
Lumbar Vertebrae/radiography/*surgery
Male
Metoclopramide/*administration & dosage/pharmacology
Middle Aged
Postoperative Complications/epidemiology
Prevalence
Prone Position
Prospective Studies
Republic of Korea
Scopolamine Hydrobromide/*administration & dosage/*pharmacology
Spinal Fusion/*adverse effects
Supine Position
Treatment Outcome
Adjuvants, Anesthesia
Antiemetics
Metoclopramide
Scopolamine Hydrobromide
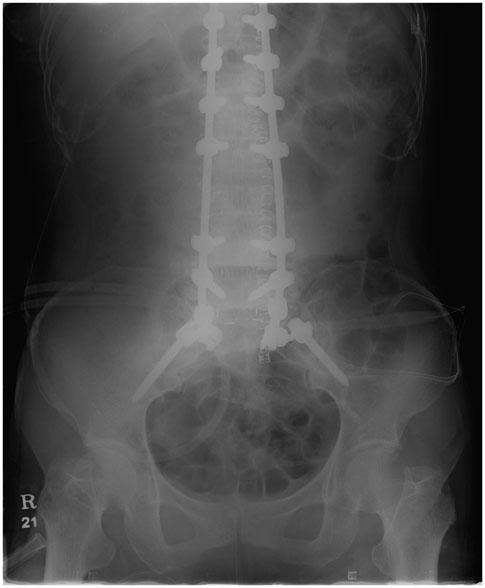
Figure
Cited by 1 articles
-
Incidence and Risk Factors of Gastrointestinal and Hepatobiliary Complications after Spinal Fusion Surgery: a Retrospective Cohort Study
Ji Hoon Bahk, Young-Hoon Kim, Hyung-Youl Park, Hyung-Ki Min, Sang-Il Kim, Kee-Yong Ha
J Korean Med Sci. 2020;35(40):e345. doi: 10.3346/jkms.2020.35.e345.
Reference
-
1. Ratliff JK, Lebude B, Albert T, Anene-Maidoh T, Anderson G, Dagostino P, et al. Complications in spinal surgery: comparative survey of spine surgeons and patients who underwent spinal surgery. J Neurosurg Spine. 2009; 10:578–584.
Article2. Cho KJ, Suk SI, Park SR, Kim JH, Kim SS, Choi WK, et al. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine (Phila Pa 1976). 2007; 32:2232–2237.3. Althausen PL, Gupta MC, Benson DR, Jones DA. The use of neostigmine to treat postoperative ileus in orthopedic spinal patients. J Spinal Disord. 2001; 14:541–545.
Article4. Breusch SJ, Lavender CP. Acute pseudo-obstruction of the colon following left-sided total hip replacement: an analysis of five patients. Int J Clin Pract. 1997; 51:327–329.5. elMaraghy AW, Schemitsch EH, Burnstein MJ, Waddell JP. Ogilvie's syndrome after lower extremity arthroplasty. Can J Surg. 1999; 42:133–137.6. Bell DF, Moseley CF, Koreska J. Unit rod segmental spinal instrumentation in the management of patients with progressive neuromuscular spinal deformity. Spine (Phila Pa 1976). 1989; 14:1301–1307.7. Caner H, Bavbek M, Albayrak A, Altinörs TC. Ogilvie's syndrome as a rare complication of lumbar disc surgery. Can J Neurol Sci. 2000; 27:77–78.8. Faciszewski T, Winter RB, Lonstein JE, Denis F, Johnson L. The surgical and medical perioperative complications of anterior spinal fusion surgery in the thoracic and lumbar spine in adults. A review of 1223 procedures. Spine (Phila Pa 1976). 1995; 20:1592–1599.
Article9. Hannon JK, Faircloth WB, Lane DR, Ronderos JF, Snow LL, Weinstein LS, et al. Comparison of insufflation vs. retractional technique for laparoscopic-assisted intervertebral fusion of the lumbar spine. Surg Endosc. 2000; 14:300–304.
Article10. Kang BU, Choi WC, Lee SH, Jeon SH, Park JD, Maeng DH, et al. An analysis of general surgery-related complications in a series of 412 minilaparotomic anterior lumbosacral procedures. J Neurosurg Spine. 2009; 10:60–65.11. Scaduto AA, Gamradt SC, Yu WD, Huang J, Delamarter RB, Wang JC. Perioperative complications of threaded cylindrical lumbar interbody fusion devices: anterior versus posterior approach. J Spinal Disord Tech. 2003; 16:502–507.
Article12. Benacker SA. Managing quality on an orthopedic service: ileus in the lumbar spinal fusion patient. J Healthc Qual. 1993; 15:17–20.
Article13. Clarke HD, Berry DJ, Larson DR. Acute pseudo-obstruction of the colon as a postoperative complication of hip arthroplasty. J Bone Joint Surg Am. 1997; 79:1642–1647.14. Rex DK. Colonoscopy and acute colonic pseudo-obstruction. Gastrointest Endosc Clin N Am. 1997; 7:499–508.15. Ponec RJ, Saunders MD, Kimmey MB. Neostigmine for the treatment of acute colonic pseudo-obstruction. N Engl J Med. 1999; 341:137–141.16. Chan DC, Liu YC, Chen CJ, Yu JC, Chu HC, Chen FC, et al. Preventing prolonged post-operative ileus in gastric cancer patients undergoing gastrectomy and intra-peritoneal chemotherapy. World J Gastroenterol. 2005; 11:4776–4781.
Article17. Stewart D, Waxman K. Management of postoperative ileus. Am J Ther. 2007; 14:561–566.
Article18. Mycek MJ, Harvey RA, Champe PC. Lippincott's Illustrated Reviews: Pharmacology. 2nd ed. Philadelphia: Lippincott, Williams & Wilkins;2000.19. Pappano AJ. Cholinoceptor-blocking drugs. In : Katzung BG, editor. Basic & clinical pharmacology. 8th ed. Philadelphia: Lange Medical Books/McGraw-Hill;2001. p. 107–119.20. Altman DF. Drugs used in gastrointestinal diseases. In : Katzung BG, editor. Basic & clinical pharmacology. 8th ed. Philadelphia: Lange Medical Books/McGraw-Hill;2001. p. 1064–1076.21. Holte K, Kehlet H. Postoperative ileus: progress towards effective management. Drugs. 2002; 62:2603–2615.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Quetiapine Related Acute Paralytic Ileus in a Bipolar I Disorder Patient with Successful Low Dose Amisulpride Substitution: A Case Report
- Neostigmine Treatment of Paralytic Ileus in Critically Ill Patients
- Paralytic Ileus as a Presentation of Antiphospholipid Syndrome in a Patient with Renal Angiomyolipoma: A Case Report
- Risk factors for postoperative ileus
- Factors associated with the Development of Paralytic Ileus in Medical ICU Patients on Mechanical Ventilation