J Korean Soc Radiol.
2010 Dec;63(6):519-524.
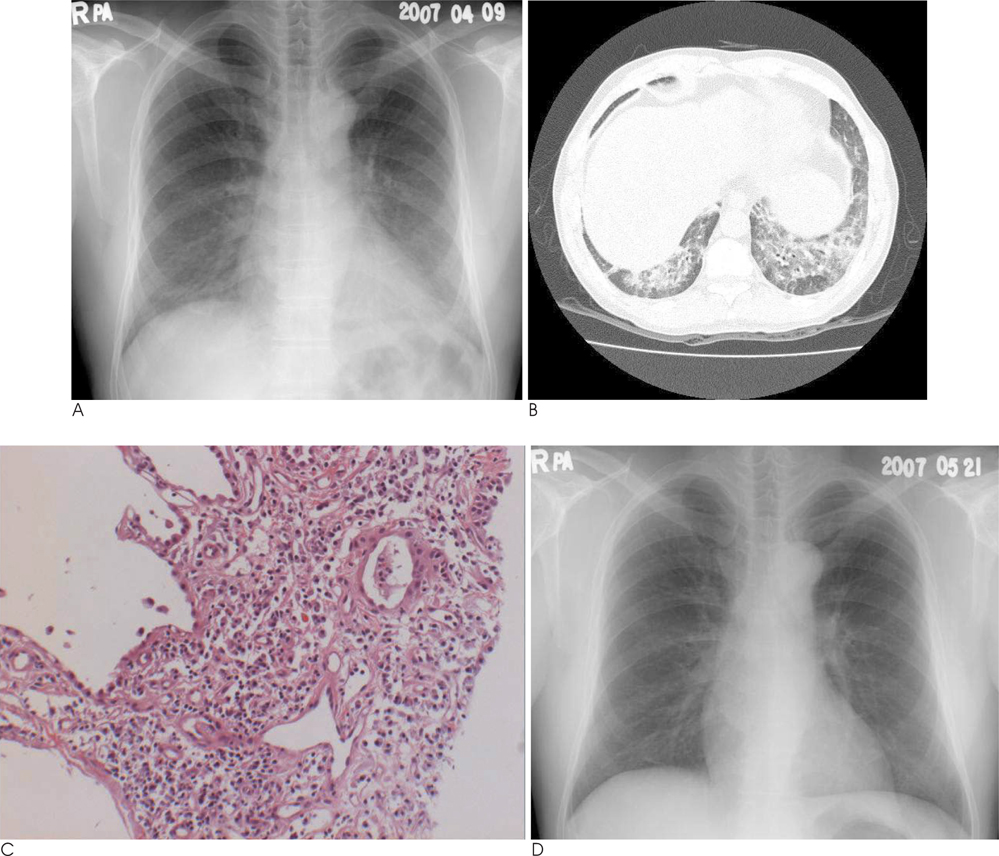
Mixed Herbal Medicine Induced Diffuse Infiltrative Lung Disease: The HRCT and Histopathologic Findings
- Affiliations
-
- 1Department of Radiology, Sanggye Paik Hospital, Inje University, Korea.
- 2Department of Health Promotion Medicine, Mokdong Hospital, Ewha Womans University, Korea. kjshpc@ewha.ac.kr
- 3Department of Pathology, Sanggye Paik Hospital, Inje University, Korea.
Abstract
- PURPOSE
The purpose of this study was to evaluate the high-resolution CT (HRCT) and pathologic findings of mixed herbal medicine-induced diffuse interstitial lung disease.
MATERIALS AND METHODS
Eight patients (6 women and 2 men, age range: 31 to 81 years, mean age: 51.4 years) who presented with cough or dyspnea after taking mixed herbal medicine were included in this study. All the patients underwent plain chest radiography and HRCT. We obtained pathologic specimens from 7 patients via fluoroscopy guided large bore cutting needle biopsy and transbronchial lung biopsy. All the patients were treated with steroid therapy.
RESULTS
The most common HRCT finding was bilateral diffuse ground glass opacity (n=7), followed by peribronchial consolidation (n=5) and inter- or intralobular septal thickening (n=2). For the disease distribution, the lower lung zone was dominantly involved. The pathologic results of 7 patients were nonspecific interstitial pneumonia (n=3), bronchiolitis obliterans organizing pneumonia (n=2), hypersensitivity pneumonitis (n=1) and eosinophilic pneumonia (n=1). Irrespective of the pathologic results, all 8 patients improved clinically and radiologically after steroid treatment.
CONCLUSION
The HRCT findings of mixed herbal medicine-induced diffuse infiltrative lung disease were mainly bilateral diffuse ground glass opacity, peribronchial consolidation and dominant involvement of the lower lung zone. Those pathologic findings were nonspecific and the differential diagnosis could include interstitial pneumonia, bronchiolitis obliterans organizing pneumonia, hypersensitivity pneumonitis and eosinophilic pneumonia.
MeSH Terms
Figure
Reference
-
1. Tsukiyama K, Tasaka Y, Nakajima M, Hino J, Nakahama C, Okimoto N, et al. A case of pneumonitis due to sho-saiko-to. Nihon Kyobu Shikkan Gakkai Zasshi. 1989; 27:1556–1561.2. Takeshita K, Saisho Y, Kitamura K, Kaburagi N, Funabiki T, Inamura T, et al. Pneumonitis induced by ou-gon (scullcap). Intern Med. 2001; 40:764–768.3. Shiota Y, Wilson JG, Matsumoto H, Munemasa M, Okamura M, Hiyama J, et al. Adult respiratory distress syndrome induced by a Chinese medicine, Kamisyoyo-san. Intern Med. 1996; 35:494–496.4. Sakamoto O, Ichikado K, Kohrogi H, Suga M. Clinical and CT characteristics of Chinese medicine-induced acute respiratory distress syndrome. Respirology. 2003; 8:344–350.5. Heki U, Fujimura M, Ogawa H, Matsuda T, Kitagawa M. Pneumonitis caused by saikokeisikankyou-tou, an herbal drug. Intern Med. 1997; 36:214–217.6. Akoun GM, Cadranel JL, Milleron BJ, D'Ortho MP, Mayaud CM. Bronchoalveolar lavage cell data in 19 patients with drug-associated pneumonitis (except amiodarone). Chest. 1991; 99:98–104.7. Akira M, Ishikawa H, Yamamoto S. Drug-induced pneumonitis: thin-section CT findings in 60 patients. Radiology. 2002; 224:852–860.8. Ishizaki T, Sasaki F, Ameshima S, Shiozaki K, Takahashi H, Abe Y, et al. Pneumonitis during interferon and/or herbal drug therapy in patients with chronic active hepatitis. Eur Respir J. 1996; 9:2691–2696.9. Kobashi Y, Nakajima M, Niki Y, Matsushima T. A case of acute eosinophilic pneumonia due to Sho-saiko-to. Nihon Kyobu Shikkan Gakkai Zasshi. 1997; 35:1372–1377.10. Yamawaki I, Katsura H, Taira M, Kadoriku C, Hashimoto I, Chiyotani A, et al. Six patients with pneumonitis related to blended Chinese traditional medicines. Nihon Kyobu Shikkan Gakkai Zasshi. 1996; 34:1331–1336.11. Hata Y, Uehara H. A case where herbal medicine sho-seiryu-to induced interstitial pneumonitis. Nihon Kokyuki Gakkai Zasshi. 2005; 43:23–31.12. Yoshida Y. A non-cardiogenic type of pulmonary edema after administration of Chinese herbal medicine (shosaikoto) - a case report. Nihon Kokyuki Gakkai Zasshi. 2003; 41:300–303.13. Miyazaki E, Ando M, Ih K, Matsumoto T, Kaneda K, Tsuda T. Pulmonary edema associated with the Chinese medicine shosaikoto. Nihon Kokyuki Gakkai Zasshi. 1998; 36:776–780.14. Sato A, Toyoshima M, Kondo A, Ohta K, Sato H, Ohsumi A. Pneumonitis induced by the herbal medicine Sho-saiko-to in Japan. Nihon Kyobu Shikkan Gakkai Zasshi. 1997; 35:391–395.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- DILD (diffuse infiltrative lung disease); Radiologic Diagnostic Approach According to High-Resolution CT Pattern
- Diffuse Infiltrative Lung Disease: Comparison of Diagnostic Accuracies of High-Resolution CT and Radiography
- The Role of HRCT in the Follow-Up Evaluation of Diffuse Interstitial Pulmonary Fibrosis
- Efficacy of Fluoroscopy-Guided Cutting Needle Lung Biopsy in Patients with Diffuse Infiltrative Lung Disease
- Pulmonary Lymphangitic Carcinomatosis: Correlation with High-Resolution CT Findings with Pulmonary Function Test