Korean Circ J.
2016 Jul;46(4):443-455. 10.4070/kcj.2016.46.4.443.
Revisit of Functional Tricuspid Regurgitation; Current Trends in the Diagnosis and Management
- Affiliations
-
- 1Department of Cardiac, Thoracic and Vascular Sciences, University of Padua, School of Medicine, Padua, Italy. lpbadano@gmail.com
- KMID: 2344418
- DOI: http://doi.org/10.4070/kcj.2016.46.4.443
Abstract
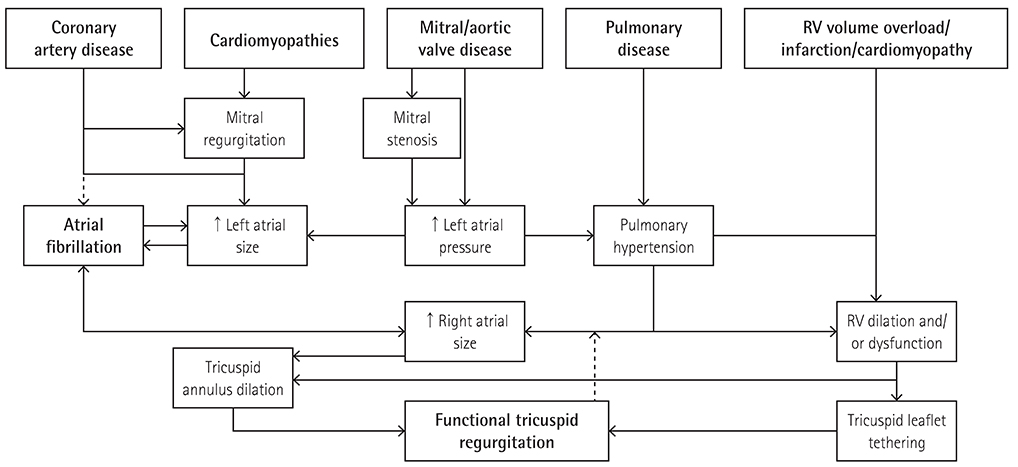
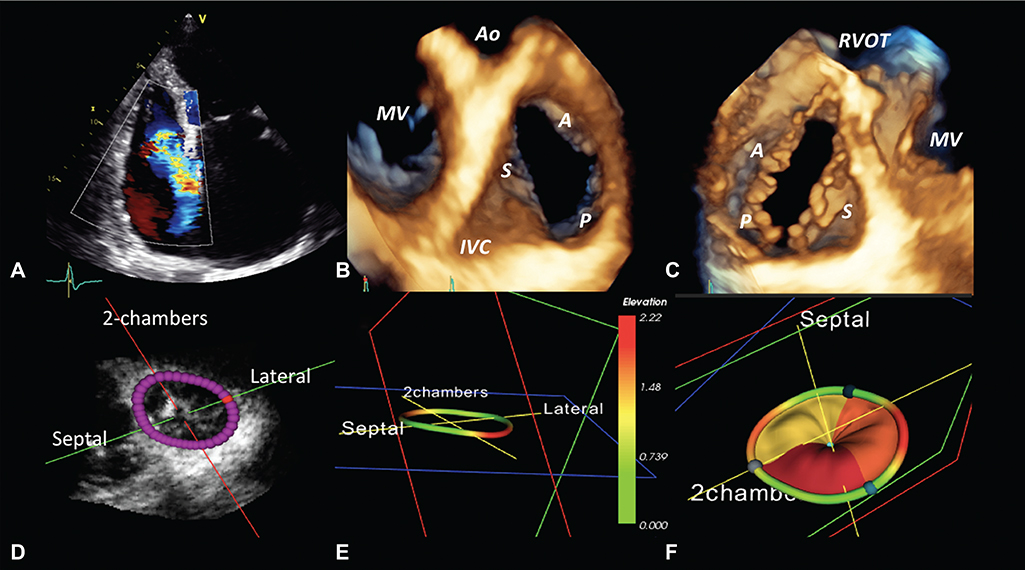
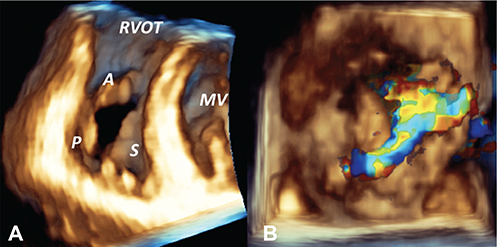
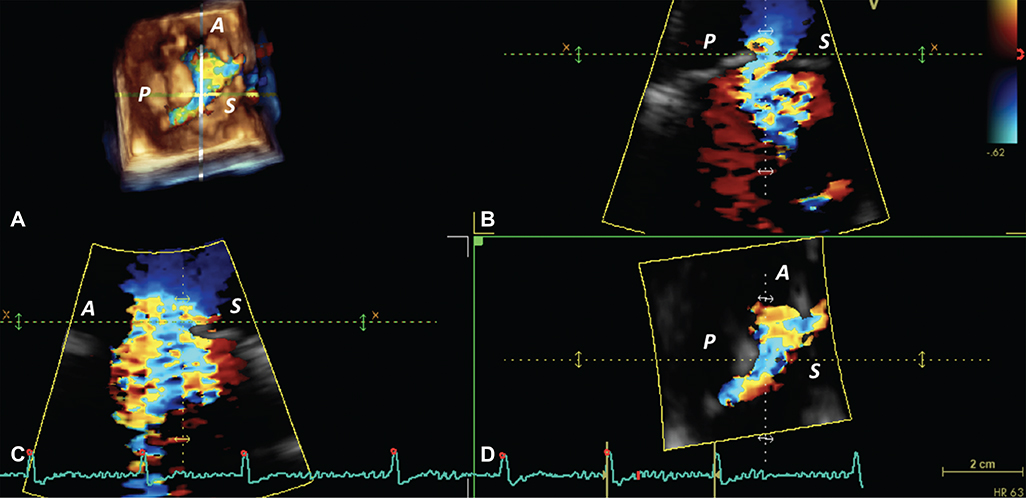
- Current knowledge of functional tricuspid regurgitation (FTR) as a progressive entity, worsening the prognosis of patients irrespective of its aetiology, has led to renewed interest in the pathophysiology and assessment of FTR. For the proper management of FTR, not only its severity, but also the mechanisms, the mode of leaflet coaptation, the degree of tricuspid annulus enlargement and leaflet tenting, and the haemodynamic consequences for right atrial and right ventricular morphology and function have to be taken into account. A better assessment of the anatomy and function of tricuspid apparatus and tricuspid regurgitation severity should help with the appropriate selection of patients who will benefit from either surgical tricuspid valve repair/replacement or a percutaneous procedure, especially among patients who are to undergo or have undergone primary left-sided valvular surgery. In this article, we review the anatomy, pathophysiology and the use of imaging techniques to assess patients with FTR, as well as the various treatment options for FTR, including emerging transcatheter procedures. The limitations affecting the current approach to FTR patients and the unmet clinical needs for their management have also been discussed.
Keyword
Figure
Cited by 2 articles
-
Current Unmet Needs and Clues to the Solution in the Management of Tricuspid Regurgitation
Byung Joo Sun, Jae-Hyeong Park
Korean Circ J. 2022;52(6):414-428. doi: 10.4070/kcj.2022.0117.Be Prepared: New Era of Heart-Team Approach for the Treatment of Tricuspid Regurgitation
Cheong Lim, Joon Chul Jung
Korean Circ J. 2023;53(11):787-789. doi: 10.4070/kcj.2023.0225.
Reference
-
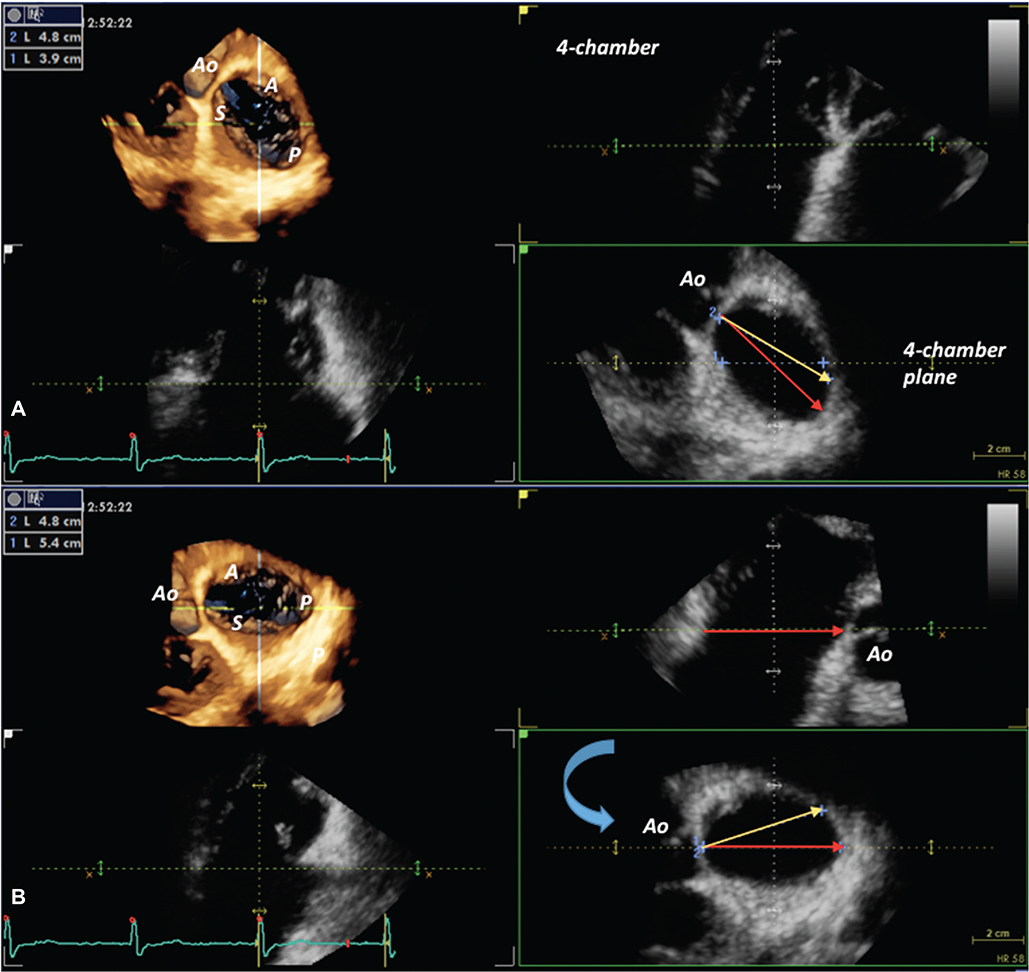
1. Braunwald NS, Ross J Jr, Morrow AG. Conservative management of tricuspid regurgitation in patients undergoing mitral valve replacement. Circulation. 1967; 35:4 Suppl. I63–I69.2. Sade RM, Castaneda AR. The dispensable right ventricle. Surgery. 1975; 77:624–631.3. Kim JB, Yoo DG, Kim GS, et al. Mild-to-moderate functional tricuspid regurgitation in patients undergoing valve replacement for rheumatic mitral disease: the influence of tricuspid valve repair on clinical and echocardiographic outcomes. Heart. 2012; 98:24–30.4. Nath J, Foster E, Heidenreich PA. Impact of tricuspid regurgitation on long-term survival. J Am Coll Cardiol. 2004; 43:405–409.5. Shiran A, Sagie A. Tricuspid regurgitation in mitral valve disease incidence, prognostic implications, mechanism, and management. J Am Coll Cardiol. 2009; 53:401–408.6. Jeong DS, Park PW, Mwambu TP, et al. Tricuspid reoperation after left-sided rheumatic valve operations. Ann Thorac Surg. 2013; 95:2007–2013.7. Kim YI, Kwon DA, Kim HK, et al. Determinants of surgical outcome in patients with isolated tricuspid regurgitation. Circulation. 2009; 120:1672–1678.8. Zhu TY, Wang JG, Meng X. Does concomitant tricuspid annuloplasty increase perioperative mortality and morbidity when correcting left-sided valve disease? Interact Cardiovasc Thorac Surg. 2015; 20:114–118.9. Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC). European Association for Cardio-Thoracic Surgery (EACTS). Vahanian A, et al. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J. 2012; 33:2451–2496.10. Sutton JP 3rd, Ho SY, Vogel M, Anderson RH. Is the morphologically right atrioventricular valve tricuspid? J Heart Valve Dis. 1995; 4:571–575.11. Victor S, Nayak VM. The tricuspid valve is bicuspid. J Heart Valve Dis. 1994; 3:27–36.12. Basso C, Muraru D, Badano LP, Thiene G. Anatomy and pathology of right-sided atrioventricular and semilunar valves. In : Rajamannan N, editor. Cardiac Valvular Medicine. London: Springer-Verlag;2013. p. 211–221.13. Miglioranza MH, Mihăilă S, Muraru D, Cucchini U, Iliceto S, Badano LP. Dynamic changes in tricuspid annular diameter measurement in relation to the echocardiographic view and timing during the cardiac cycle. J Am Soc Echocardiogr. 2015; 28:226–235.14. Fukuda S, Saracino G, Matsumara Y, et al. Three-dimensional geometry of the tricuspid annulus in healthy subjects and in patients with functional tricuspid regurgitation: a real-time, 3-dimensional echocardiographic study. Circulation. 2006; 114:1 Suppl. I492–I498.15. Ton-Nu TT, Levine RA, Handschumacher MD, et al. Geometric determinants of functional tricuspid regurgitation: insights from 3-dimensional echocardiography. Circulation. 2006; 114:143–149.16. Badano LP, Muraru D, Enriquez-Sarano M. Assessment of functional tricuspid regurgitation. Eur Heart J. 2013; 34:1875–1885.17. Dreyfus GD, Martin RP, Chan KM, Dulguerov F, Alexandrescu C. Functional tricuspid regurgitation: a need to revise our understanding. J Am Coll Cardiol. 2015; 65:2331–2336.18. Rogers JH, Bolling SF. The tricuspid valve: current perspective and evolving management of tricuspid regurgitation. Circulation. 2009; 119:2718–2725.19. Lancellotti P, Moura L, Pierard LA, et al. European Association of Echocardiography recommendations for the assessment of valvular regurgitation. Part 2: mitral and tricuspid regurgitation (native valve diseases). Eur J Echocardiogr. 2010; 11:307–332.20. Singh JP, Evans JC, Levy D, et al. Prevalence and clinical determinants of mitral, tricuspid, and aortic regurgitation (the Framingham Heart Study). Am J Cardiol. 1999; 83:897–902.21. Badano LP, Agricola E, Perez de Isla L, Gianfagna P, Zamorano JL. Evaluation of the tricuspid valve morphology and function by transthoracic real-time three-dimensional echocardiography. Eur J Echocardiogr. 2009; 10:477–484.22. Muraru D, Badano LP. Assessment of tricuspid valve morphology and function. In : Badano LP, Lang RM, Zamorano JL, editors. Textbook of real-time three dimensional echocardiography. London: Springler;2011. p. 173–182.23. Kim HK, Kim YJ, Park JS, et al. Determinants of the severity of functional tricuspid regurgitation. Am J Cardiol. 2006; 98:236–242.24. Tribouilloy CM, Enriquez-Sarano M, Bailey KR, Tajik AJ, Seward JB. Quantification of tricuspid regurgitation by measuring the width of the vena contracta with Doppler color flow imaging: a clinical study. J Am Coll Cardiol. 2000; 36:472–478.25. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 63:e57–e185.26. Song JM, Jang MK, Choi YS, et al. The vena contracta in functional tricuspid regurgitation: a real-time three-dimensional color Doppler echocardiography study. J Am Soc Echocardiogr. 2011; 24:663–670.27. Chen TE, Kwon SH, Enriquez-Sarano M, Wong BF, Mankad SV. Three-dimensional color Doppler echocardiographic quantification of tricuspid regurgitation orifice area: comparison with conventional two-dimensional measures. J Am Soc Echocardiogr. 2013; 26:1143–1152.28. Mascherbauer J, Maurer G. The forgotten valve: lessons to be learned in tricuspid regurgitation. Eur Heart J. 2010; 31:2841–2843.29. Topilsky Y, Tribouilloy C, Michelena HI, Pislaru S, Mahoney DW, Enriquez-Sarano M. Pathophysiology of tricuspid regurgitation: quantitative Doppler echocardiographic assessment of respiratory dependence. Circulation. 2010; 122:1505–1513.30. Miglioranza MH, Mihăilă S, Muraru D, Cucchini U, Iliceto S, Badano LP. Variability of Tricuspid Annulus Diameter Measurement in Healthy Volunteers. JACC Cardiovasc Imaging. 2015; 8:864–866.31. de Agustin JA, Viliani D, Vieira C, et al. Proximal isovelocity surface area by single-beat three-dimensional color Doppler echocardiography applied for tricuspid regurgitation quantification. J Am Soc Echocardiogr. 2013; 26:1063–1072.32. Kim HK, Kim YJ, Park EA, et al. Assessment of hemodynamic effects of surgical correction of severe functional tricuspid regurgitation: cardiac magnetic resonance imaging study. Eur Heart J. 2010; 31:1520–1528.33. Maffessanti F, Gripari P, Pontone G, et al. Three-dimensional dynamic assessment of tricuspid and mitral annuli using cardiovascular magnetic resonance. Eur Heart J Cardiovasc Imaging. 2013; 14:986–995.34. Anwar AM, Soliman OI, Nemes A, van Geuns RJ, Geleijnse ML, Ten Cate FJ. Value of assessment of tricuspid annulus: real-time three-dimensional echocardiography and magnetic resonance imaging. Int J Cardiovasc Imaging. 2007; 23:701–705.35. van Rosendael PJ, Joyce E, Katsanos S, et al. Tricuspid valve remodelling in functional tricuspid regurgitation: multidetector row computed tomography insights. Eur Heart J Cardiovasc Imaging. 2016; 17:96–105.36. Nasis A, Mottram PM, Cameron JD, Seneviratne SK. Current and evolving clinical applications of multidetector cardiac CT in assessment of structural heart disease. Radiology. 2013; 267:11–25.37. Tops LF, Krishnàn SC, Schuijf JD, Schalij MJ, Bax JJ. Noncoronary applications of cardiac multidetector row computed tomography. JACC Cardiovascular imaging. 2008; 1:94–106.38. Porter A, Shapira Y, Wurzel M, et al. Tricuspid regurgitation late after mitral valve replacement: clinical and echocardiographic evaluation. J Heart Valve Dis. 1999; 8:57–62.39. De Bonis M, Lapenna E, Sorrentino F, et al. Evolution of tricuspid regurgitation after mitral valve repair for functional mitral regurgitation in dilated cardiomyopathy. Eur J Cardiothorac Surg. 2008; 33:600–606.40. Di Mauro M, Bezante GP, Di Baldassarre A, et al. Functional tricuspid regurgitation: an underestimated issue. Int J Cardiol. 2013; 168:707–715.41. Vassileva CM, Shabosky J, Boley T, Markwell S, Hazelrigg S. Tricuspid valve surgery: the past 10 years from the Nationwide Inpatient Sample (NIS) database. J Thorac Cardiovasc Surg. 2012; 143:1043–1049.42. Di Mauro M, Bivona A, Iacò AL, et al. Mitral valve surgery for functional mitral regurgitation: prognostic role of tricuspid regurgitation. Eur J Cardiothorac Surg. 2009; 35:635–639. discussion 639-40.43. Ruel M, Kulik A, Rubens FD, et al. Late incidence and determinants of reoperation in patients with prosthetic heart valves. Eur J Cardiothorac Surg. 2004; 25:364–370.44. Tang GH, David TE, Singh SK, Maganti MD, Armstrong S, Borger MA. Tricuspid valve repair with an annuloplasty ring results in improved long-term outcomes. Circulation. 2006; 114:1 Suppl. I577–I581.45. Rivera R, Duran E, Ajuria M. Carpentier's flexible ring versus De Vega's annuloplasty. A prospective randomized study. J Thorac Cardiovasc Surg. 1985; 89:196–203.46. McCarthy PM, Bhudia SK, Rajeswaran J, et al. Tricuspid valve repair: durability and risk factors for failure. J Thorac Cardiovasc Surg. 2004; 127:674–685.47. Dreyfus GD, Corbi PJ, Chan KM, Bahrami T. Secondary tricuspid regurgitation or dilatation: which should be the criteria for surgical repair? Ann Thorac Surg. 2005; 79:127–132.48. Benedetto U, Melina G, Angeloni E, et al. Prophylactic tricuspid annuloplasty in patients with dilated tricuspid annulus undergoing mitral valve surgery. J Thorac Cardiovasc Surg. 2012; 143:632–638.49. Navia JL, Brozzi NA, Klein AL, et al. Moderate tricuspid regurgitation with left-sided degenerative heart valve disease: to repair or not to repair? Ann Thorac Surg. 2012; 93:59–67. discussion 68-9.50. Taramasso M, Maisano F, De Bonis M, et al. Prognostic impact and late evolution of untreated moderate (2/4+) functional tricuspid regurgitation in patients undergoing aortic valve replacement. J Card Surg. 2016; 31:9–14.51. Starck CT, Kempfert J, Falk V. Tricuspid valve interventions: surgical techniques and outcomes. EuroIntervention. 2015; 11:Suppl W. W128–W132.52. Taramasso M, Pozzoli A, Guidotti A, et al. Percutaneous tricuspid valve therapies: the new frontier. Eur Heart J. 2016; pii:ehv766. [Epub ahead of print].53. Lauten A, Figulla HR. Tricuspid valve interventions in 2015. EuroIntervention. 2015; 11:Suppl W. W133–W136.54. Arsalan M, Walther T, Smith RL 2nd, Grayburn PA. Tricuspid regurgitation diagnosis and treatment. Eur Heart J. 2015; pii: ehv487. [Epub ahead of print].55. Tornos Mas P, Rodríguez-Palomares JF, Antunes MJ. Secondary tricuspid valve regurgitation: a forgotten entity. Heart. 2015; 101:1840–1848.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
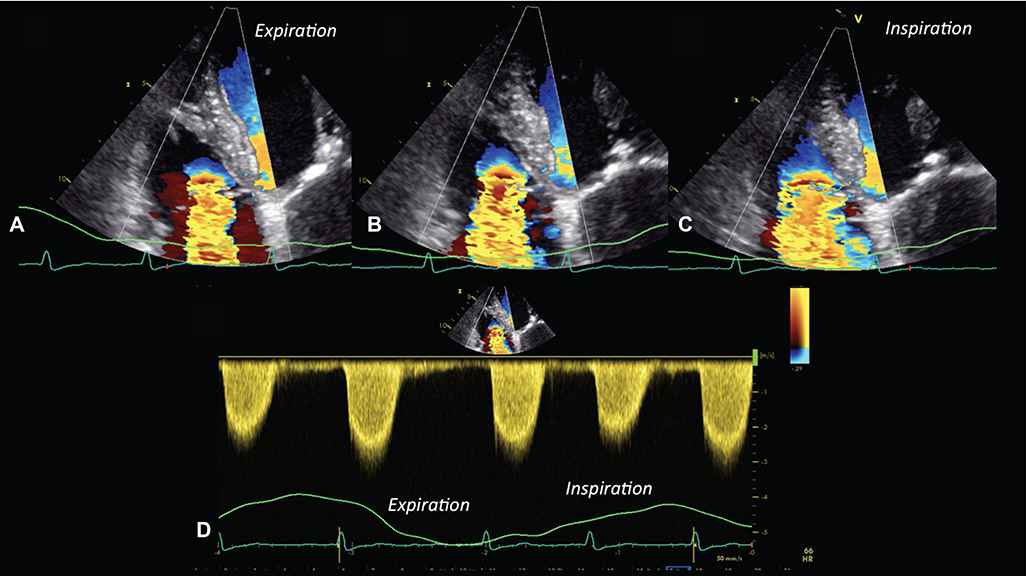
- Share
- Similar articles
-
- Permanent Pacemaker Lead Induced Severe Tricuspid Regurgitation in Patient Undergoing Multiple Valve Surgery
- Clinical Implications of Functional Tricuspid Regurgitation and Optimal Surgical Timing
- Comparison of Cine Magnetic Resonance Imaging with Doppler Echocardiography for the Quantative Evaluation of Tricuspid Regurgitation in Newborn
- Repair of Posttraumatic Tricuspid Regurgitation Using Artificial Chordae and an Annuloplasty Ring
- Tricuspid Regurgitation in Heart Diseases in Infants and Children