Korean J Radiol.
2015 Dec;16(6):1326-1331. 10.3348/kjr.2015.16.6.1326.
Ultrasound-Guided Percutaneous Removal of Wooden Foreign Bodies in the Extremities with Hydro-Dissection Technique
- Affiliations
-
- 1Department of Radiology, Sungkyunkwan University School of Medicine, Kangbuk Samsung Hospital, Seoul 03181, Korea.
- 2Department of Radiology, Dongsan Medical Center, Keimyung University School of Medicine, Daegu 41931, Korea. parkhiji@kangwon.ac.kr
- 3Department of Orthopaedic Surgery, Dongsan Medical Center, Keimyung University School of Medicine, Daegu 41931, Korea.
- 4Department of Radiology, Inje University College of Medicine, Busan Paik Hospital, Busan 47392, Korea.
- KMID: 2344288
- DOI: http://doi.org/10.3348/kjr.2015.16.6.1326
Abstract
OBJECTIVE
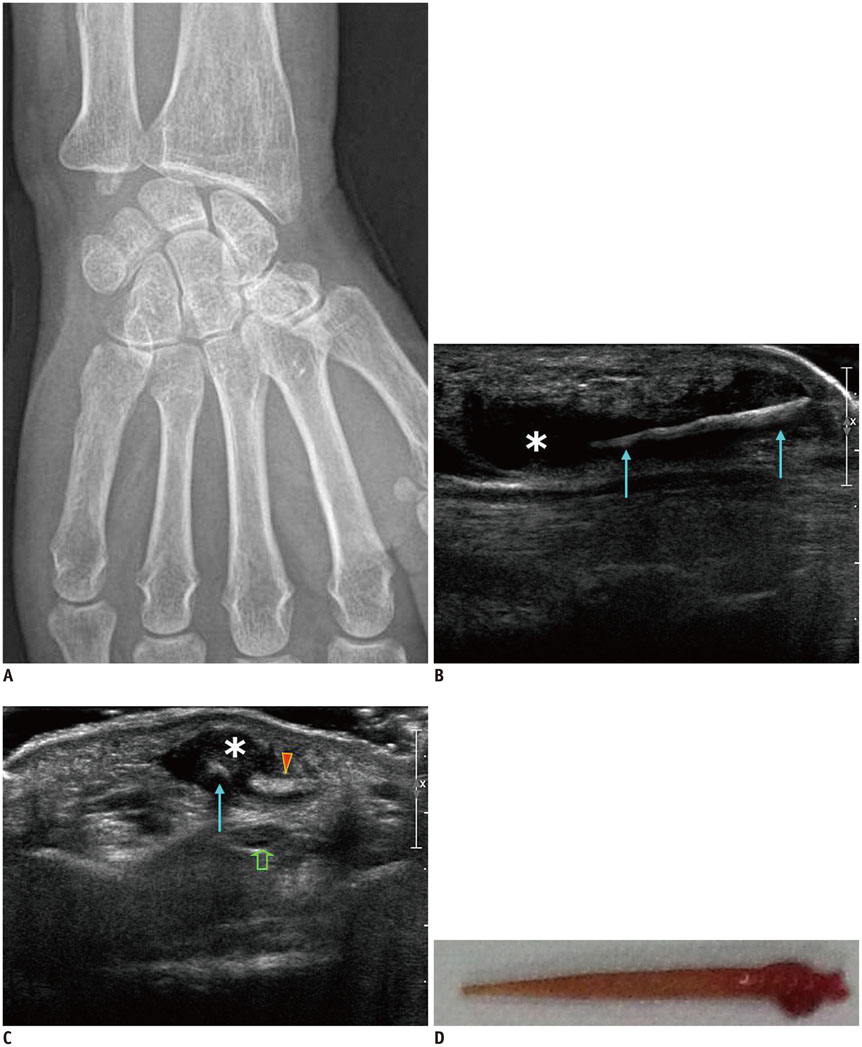
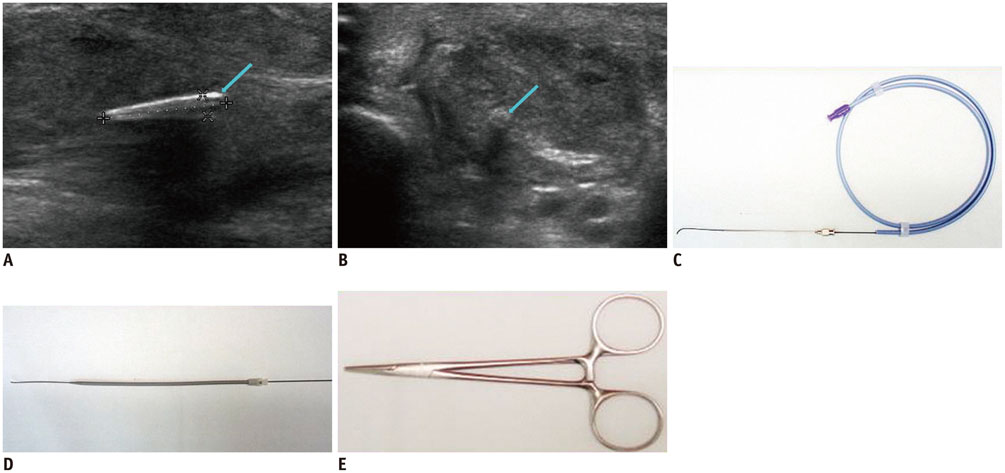
We described the technique of ultrasound (US)-guided percutaneous removal of the foreign bodies (FB) with hydro-dissection in the radiologic department and presented video files of several cases.
MATERIALS AND METHODS
Four patients referred to the radiology department for US evaluation and US-guided percutaneous removal of the FBs in the upper and lower extremities between November, 2006 and November, 2013 were included in this study. The procedures started with US evaluation for the exact location and shape of the FB. A 5 mm-sized skin incision was made at the site of the nearest point from the FB where no passing arteries or tendons were present. We adopted a hydrodissection technique to separate the FB from adjacent tissue using a 2% lidocaine solution. Injected anesthetics detached the FBs from surrounding tissue and thereby facilitated removal. After the tip of the mosquito forceps reached the FB, the wooden FBs were removed.
RESULTS
The mean time required for the entire procedure was approximately 20 minutes. There were no significant complications during the US-guided removal or long-term complications after the procedure. All 4 FBs were successfully removed from the soft tissue under US guidance.
CONCLUSION
Ultrasound-guided percutaneous removal of the FBs with hydro-dissection in the radiology department is a less invasive and safe method over surgical removal in the operating room. Additionally, the use of a guide wire and serial dilator may help minimize soft tissue injury and facilitate the introduction of forceps.
Keyword
MeSH Terms
Figure
Reference
-
1. Budhram GR, Schmunk JC. Bedside ultrasound AIDS identification and removal of cutaneous foreign bodies: a case series. J Emerg Med. 2014; 47:e43–e48.2. Callegari L, Leonardi A, Bini A, Sabato C, Nicotera P, Spano' E, et al. Ultrasound-guided removal of foreign bodies: personal experience. Eur Radiol. 2009; 19:1273–1279.3. Anderson MA, Newmeyer WL 3rd, Kilgore ES Jr. Diagnosis and treatment of retained foreign bodies in the hand. Am J Surg. 1982; 144:63–67.4. Lee SM, Cho CH. Ultrasound-guided percutaneous removal of foreign body using hydrodissection and serial dilators. J Korean Orthop Assoc. 2012; 47:150–155.5. Nwawka OK, Kabutey NK, Locke CM, Castro-Aragon I, Kim D. Ultrasound-guided needle localization to aid foreign body removal in pediatric patients. J Foot Ankle Surg. 2014; 53:67–70.6. Mulvaney SW. Ultrasound-guided percutaneous neuroplasty of the lateral femoral cutaneous nerve for the treatment of meralgia paresthetica: a case report and description of a new ultrasound-guided technique. Curr Sports Med Rep. 2011; 10:99–104.7. Peterson JJ, Bancroft LW, Kransdorf MJ. Wooden foreign bodies: imaging appearance. AJR Am J Roentgenol. 2002; 178:557–562.8. Choudhari KA, Muthu T, Tan MH. Progressive ulnar neuropathy caused by delayed migration of a foreign body. Br J Neurosurg. 2001; 15:263–265.9. Jacobson JA, Powell A, Craig JG, Bouffard JA, van Holsbeeck MT. Wooden foreign bodies in soft tissue: detection at US. Radiology. 1998; 206:45–48.10. Bray PW, Mahoney JL, Campbell JP. Sensitivity and specificity of ultrasound in the diagnosis of foreign bodies in the hand. J Hand Surg Am. 1995; 20:661–666.11. Boyse TD, Fessell DP, Jacobson JA, Lin J, van Holsbeeck MT, Hayes CW. US of soft-tissue foreign bodies and associated complications with surgical correlation. Radiographics. 2001; 21:1251–1256.12. Malone DG, Clark TB, Wei N. Ultrasound-guided percutaneous injection, hydrodissection, and fenestration for carpal tunnel syndrome: description of a new technique. J Appl Res. 2010; 10:116–123.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound-Guided Percutaneous Removal of Foreign Body Using Hydrodissection and Serial Dilators
- Removal of Esophageal Foreign Body: Fluoroscopic Guided Double Balloon Technique
- Two Cases of Non-Surgical Removal of Intravascular Foreign Bodies
- Diagnosis and Management of Wooden Foreign Bodies in the Orbit: A Case Report
- Two Cases of Intraorbital Wooden Foreign Bodies