J Korean Neurosurg Soc.
2014 Sep;56(3):248-253. 10.3340/jkns.2014.56.3.248.
Emerging Surgical Strategies of Intractable Frontal Lobe Epilepsy with Cortical Dysplasia in Terms of Extent of Resection
- Affiliations
-
- 1Department of Neurosurgery, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea. drson@dsmc.or.kr
- 2Department of Pathology, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea.
- KMID: 2339965
- DOI: http://doi.org/10.3340/jkns.2014.56.3.248
Abstract
OBJECTIVE
Cortical dysplasia (CD) is one of the common causes of epilepsy surgery. However, surgical outcome still remains poor, especially with frontal lobe epilepsy (FLE), despite the advancement of neuroimaging techniques and expansion of surgical indications. The aim of this study was to focus on surgical strategies in terms of extent of resection to improve surgical outcome in the cases of FLE with CD.
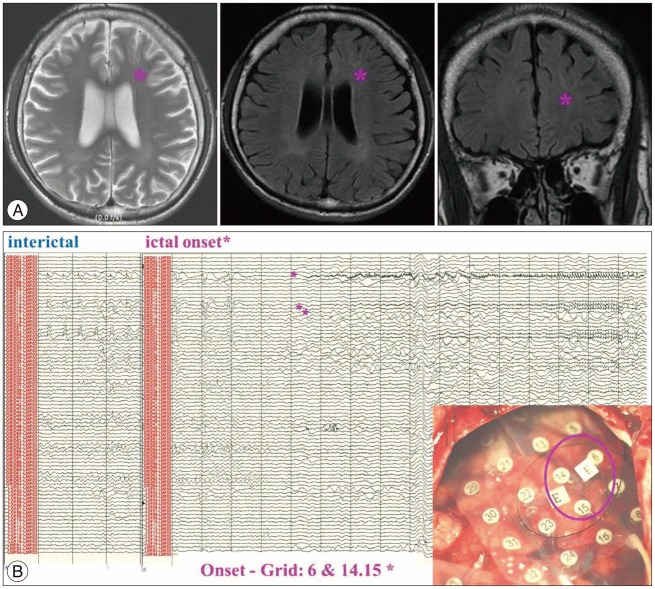
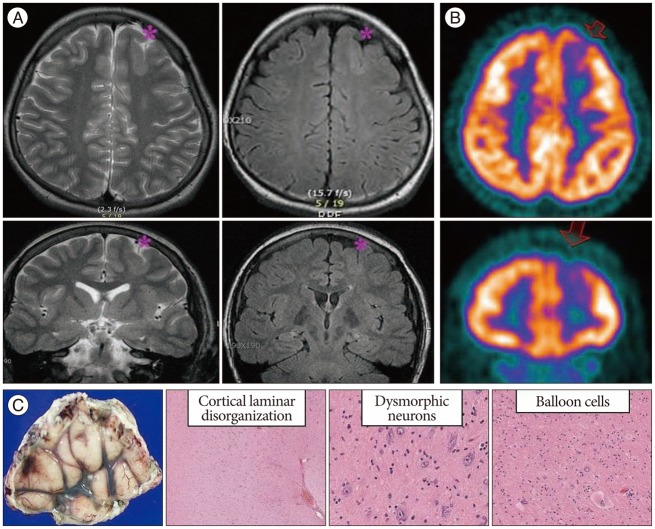
METHODS
A total of 11 patients of FLE were selected among 67 patients who were proven pathologically as CD, out of a total of 726 epilepsy surgery series since 1992. This study categorized surgical groups into three according to the extent of resection : 1) focal corticectomy, 2) regional corticectomy, and 3) partial functional lobectomy, based on the preoperative evaluation, in particular, ictal scalp EEG onset and/or intracranial recordings, and the lesions in high-resolution MRI. Surgical outcome was assessed following Engel's classification system.
RESULTS
Focal corticectomy was performed in 5 patients and regional corticectomy in another set of 5 patients. Only 1 patient underwent partial functional lobectomy. Types I and II CD were detected with the same frequency (45.45% each) and postoperative outcome was fully satisfactory (91%).
CONCLUSION
The strategy of epilepsy surgery is to focus on the different characteristics of each individual, considering the extent of real resection, which is based on the focal ictal onset consistent with neuroimaging, especially in the practical point of view of neurosurgery.
MeSH Terms
Figure
Reference
-
1. Awad IA, Rosenfeld J, Ahl J, Hahn JF, Lüders H. Intractable epilepsy and structural lesions of the brain : mapping, resection strategies, and seizure outcome. Epilepsia. 1991; 32:179–186. PMID: 1900789.
Article2. Barkovich AJ, Kuzniecky RI. Neuroimaging of focal malformations of cortical development. J Clin Neurophysiol. 1996; 13:481–494. PMID: 8978620.
Article3. Bautista RE, Cobbs MA, Spencer DD, Spencer SS. Prediction of surgical outcome by interictal epileptiform abnormalities during intracranial EEG monitoring in patients with extrahippocampal seizures. Epilepsia. 1999; 40:880–890. PMID: 10403211.
Article4. Becker AJ, Blümcke I, Urbach H, Hans V, Majores M. Molecular neuropathology of epilepsy-associated glioneuronal malformations. J Neuropathol Exp Neurol. 2006; 65:99–108. PMID: 16462201.
Article5. Blümcke I, Thom M, Aronica E, Armstrong DD, Vinters HV, Palmini A, et al. The clinicopathologic spectrum of focal cortical dysplasias : a consensus classification proposed by an ad hoc Task Force of the ILAE Diagnostic Methods Commission. Epilepsia. 2011; 52:158–174. PMID: 21219302.
Article6. Bronen RA, Vives KP, Kim JH, Fulbright RK, Spencer SS, Spencer DD. Focal cortical dysplasia of Taylor, balloon cell subtype : MR differentiation from low-grade tumors. AJNR Am J Neuroradiol. 1997; 18:1141–1151. PMID: 9194442.7. Chassoux F, Devaux B, Landré E, Turak B, Nataf F, Varlet P, et al. Stereoelectroencephalography in focal cortical dysplasia : a 3D approach to delineating the dysplastic cortex. Brain. 2000; 123(Pt 8):1733–1751. PMID: 10908202.
Article8. Cohen-Gadol AA, Ozduman K, Bronen RA, Kim JH, Spencer DD. Long-term outcome after epilepsy surgery for focal cortical dysplasia. J Neurosurg. 2004; 101:55–65. PMID: 15255252.
Article9. Davies KG, Weeks RD. Cortical resections for intractable epilepsy of extratemporal origin : experience with seventeen cases over eleven years. Br J Neurosurg. 1993; 7:343–353. PMID: 8216904.
Article10. Dubeau F, Palmini A, Fish D, Avoli M, Gambardella A, Spreafico R, et al. The significance of electrocorticographic findings in focal cortical dysplasia : a review of their clinical, electrophysiological and neurochemical characteristics. Electroencephalogr Clin Neurophysiol Suppl. 1998; 48:77–96. PMID: 9949777.11. Engel J Jr, Van Ness PC, Rasmussen TB, Ojemann LM. Outcome with respect to epileptic seizures. In : Engel J, editor. Surgical treatment of the Epilepsies. ed 2. New York: Raven Press;1993. p. 609–621.12. Englot DJ, Wang DD, Rolston JD, Shih TT, Chang EF. Rates and predictors of long-term seizure freedom after frontal lobe epilepsy surgery : a systematic review and meta-analysis. J Neurosurg. 2012; 116:1042–1048. PMID: 22304450.
Article13. Eriksson S, Malmgren K, Rydenhag B, Jönsson L, Uvebrant P, Nordborg C. Surgical treatment of epilepsy--clinical, radiological and histopathological findings in 139 children and adults. Acta Neurol Scand. 1999; 99:8–15. PMID: 9925233.
Article14. Gambardella A, Palmini A, Andermann F, Dubeau F, Da Costa JC, Quesney LF, et al. Usefulness of focal rhythmic discharges on scalp EEG of patients with focal cortical dysplasia and intractable epilepsy. Electroencephalogr Clin Neurophysiol. 1996; 98:243–249. PMID: 8641147.
Article15. Giulioni M, Rubboli G, Marucci G, Martinoni M, Volpi L, Michelucci R, et al. Seizure outcome of epilepsy surgery in focal epilepsies associated with temporomesial glioneuronal tumors : lesionectomy compared with tailored resection. J Neurosurg. 2009; 111:1275–1282. PMID: 19408976.
Article16. Gump WC, Skjei KL, Karkare SN. Seizure control after subtotal lesional resection. Neurosurg Focus. 2013; 34:E1. PMID: 23724833.
Article17. Hader WJ, Mackay M, Otsubo H, Chitoku S, Weiss S, Becker L, et al. Cortical dysplastic lesions in children with intractable epilepsy : role of complete resection. J Neurosurg. 2004; 100(2 Suppl Pediatrics):110–117. PMID: 14758938.
Article18. Harvey AS, Cross JH, Shinnar S, Mathern GW. ILAE Pediatric Epilepsy Surgery Survey Taskforce. Defining the spectrum of international practice in pediatric epilepsy surgery patients. Epilepsia. 2008; 49:146–155. PMID: 18042232.
Article19. Hashizume K, Kiriyama K, Kunimoto M, Maeda T, Tanaka T, Miyamoto A, et al. Correlation of EEG, neuroimaging and histopathology in an epilepsy patient with diffuse cortical dysplasia. Childs Nerv Syst. 2000; 16:75–79. PMID: 10663810.
Article20. Hauptman JS, Mathern GW. Surgical treatment of epilepsy associated with cortical dysplasia : 2012 update. Epilepsia. 2012; 53(Suppl 4):98–104. PMID: 22946727.
Article21. Hong SC, Kang KS, Seo DW, Hong SB, Lee M, Nam DH, et al. Surgical treatment of intractable epilepsy accompanying cortical dysplasia. J Neurosurg. 2000; 93:766–773. PMID: 11059656.
Article22. Jobst BC, Siegel AM, Thadani VM, Roberts DW, Rhodes HC, Williamson PD. Intractable seizures of frontal lobe origin : clinical characteristics, localizing signs, and results of surgery. Epilepsia. 2000; 41:1139–1152. PMID: 10999553.
Article23. Kabat J, Król P. Focal cortical dysplasia - review. Pol J Radiol. 2012; 77:35–43. PMID: 22844307.24. Kloss S, Pieper T, Pannek H, Holthausen H, Tuxhorn I. Epilepsy surgery in children with focal cortical dysplasia (FCD) : results of long-term seizure outcome. Neuropediatrics. 2002; 33:21–26. PMID: 11930272.
Article25. Kral T, Kuczaty S, Blümcke I, Urbach H, Clusmann H, Wiestler OD, et al. Postsurgical outcome of children and adolescents with medically refractory frontal lobe epilepsies. Childs Nerv Syst. 2001; 17:595–601. PMID: 11685521.
Article26. Kuzniecky RI. Neuroimaging in pediatric epilepsy. Epilepsia. 1996; 37(Suppl 1):S10–S21. PMID: 8647047.
Article27. Lee MH, Son EI. Comparison between initial and recent surgical outcome of 15-year series of surgically remediable epilepsy. J Korean Neurosurg Soc. 2010; 48:230–235. PMID: 21082050.
Article28. Liava A, Francione S, Tassi L, Lo Russo G, Cossu M, Mai R, et al. Individually tailored extratemporal epilepsy surgery in children : anatomo-electro-clinical features and outcome predictors in a population of 53 cases. Epilepsy Behav. 2012; 25:68–80. PMID: 22902651.
Article29. Palmini A, Andermann F, Olivier A, Tampieri D, Robitaille Y. Focal neuronal migration disorders and intractable partial epilepsy : results of surgical treatment. Ann Neurol. 1991; 30:750–757. PMID: 1789692.
Article30. Rosenow F, Lüders HO, Dinner DS, Prayson RA, Mascha E, Wolgamuth BR, et al. Histopathological correlates of epileptogenicity as expressed by electrocorticographic spiking and seizure frequency. Epilepsia. 1998; 39:850–856. PMID: 9701375.
Article31. Seo IY, Son EI, Yi SD, Lee CY, Lee JC, Kim DW, et al. Coexistence of neoplasia and cortical dysplasia associated with intractable epilepsy : a clinical study of seven surgical patients and surgical strategies. J Korean Neurosurg Soc. 1998; 27:516–522.32. Sinclair DB, Wheatley M, Snyder T. Frontal lobe epilepsy in childhood. Pediatr Neurol. 2004; 30:169–176. PMID: 15033198.
Article33. Sisodiya SM. Surgery for malformations of cortical development causing epilepsy. Brain. 2000; 123(Pt 6):1075–1091. PMID: 10825348.
Article34. Téllez-Zenteno JF, Dhar R, Wiebe S. Long-term seizure outcomes following epilepsy surgery : a systematic review and meta-analysis. Brain. 2005; 128:1188–1198. PMID: 15758038.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgery in Patients with Previous Resection of the Epileptogenic Zone Due to Intractable Epilepsy
- Epilepsy Surgery in Children with Intractable Partial Epilepsies
- Surgery of Intractable Epilepsy Associated with Cortical Dysplasia
- Surgical Treatment of Intractable Frontal Lobe Epilepsy
- Surgical Treatment of Intractable Frontal Lobe Epilepsy