J Korean Neurosurg Soc.
2014 Sep;56(3):211-217. 10.3340/jkns.2014.56.3.211.
Early Vertebroplasty versus Delayed Vertebroplasty for Acute Osteoporotic Compression Fracture : Are the Results of the Two Surgical Strategies the Same?
- Affiliations
-
- 1Department of Neurosurgery, Gachon University Gil Medical Center, Incheon, Korea. samddal@gilhospital.com
- KMID: 2339959
- DOI: http://doi.org/10.3340/jkns.2014.56.3.211
Abstract
OBJECTIVE
In Korea, early vertebroplasty (EVP) or delayed vertebroplasty (DVP, which is performed at least 2 weeks after diagnosis) were performed for the treatment of acute osteoporotic compression fracture (OCF) of the spine. The present study compared the outcomes of two surgical strategies for the treatment of single-level acute OCF in the thoracolumbar junction (T12-L2).
METHODS
From 2004 to 2010, 23 patients were allocated to the EVP group (EVPG) and 27 patients to the DVP group (DVPG). Overall mean age was 68.3+/-7.9 and minimum follow-up period was 1.0 year. Retrospective study of clinical and radiological results was conducted.
RESULTS
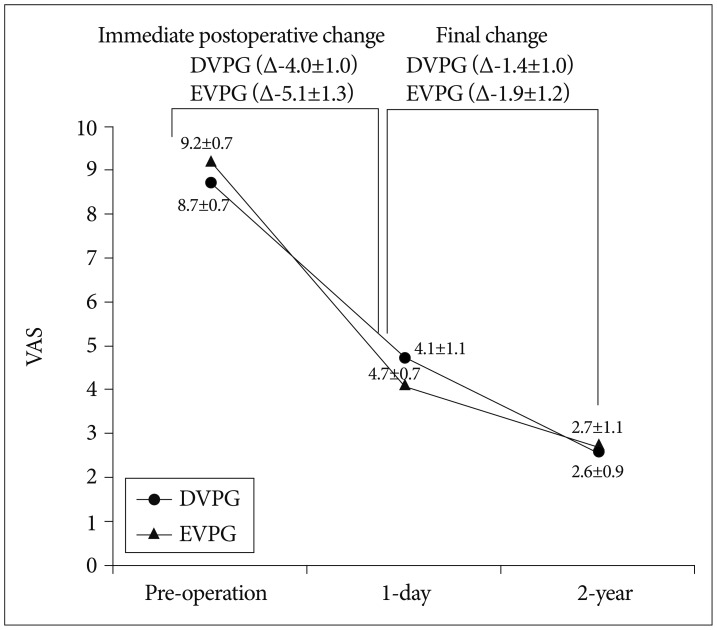
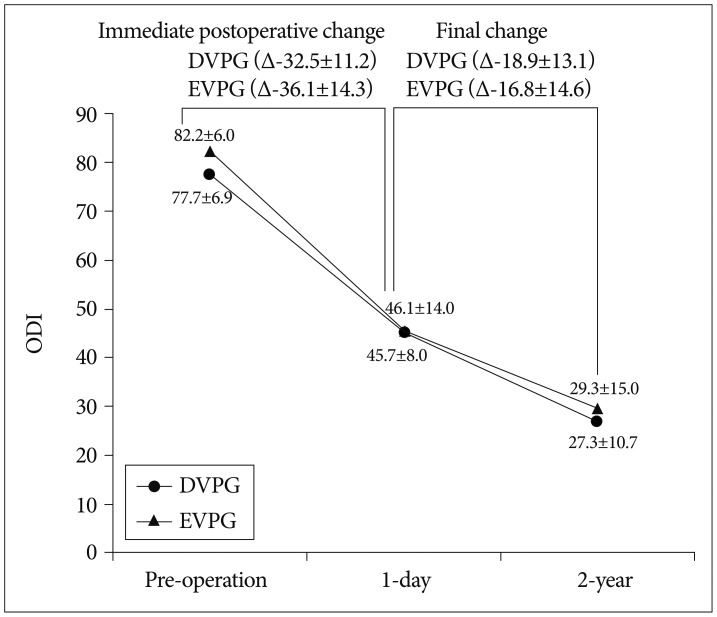
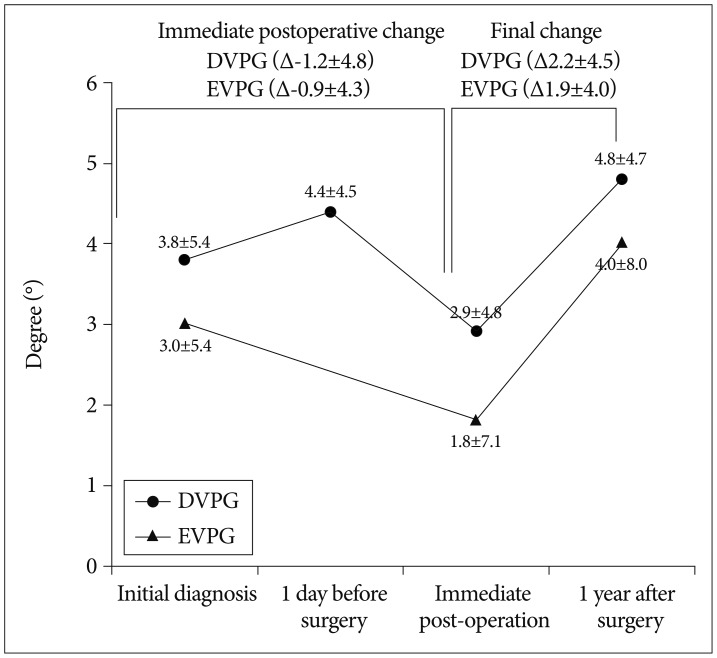
No significant differences in baseline characteristics were observed between the two groups. As expected, mean duration from onset to vertebroplasty and mean duration of hospital stay were significantly longer in the DVPG (17.1+/-2.1 and 17.5+/-4.2) than in the EVPG (3.8+/-3.3 and 10.8+/-5.1, p=0.001). Final clinical outcome including visual analogue scale (VAS), Oswestry Disability Index, and Odom's criteria did not differ between the two groups. However, immediate improvement of the VAS after vertebroplasty was greater in the EVPG (5.1+/-1.3) than in the DVPG (4.0+/-1.0, p=0.002). The proportion of cement leakage was lower in the EVPG (30.4%) than in the DVPG (59.3%, p=0.039). In addition, semiquantitative grade of cement interdigitation was significantly more favorable in the EVPG than in the DVPG (p=0.003). Final vertebral body collapse and segmental kyphosis did not differ significantly between the two groups.
CONCLUSION
Our findings suggest that EVP achieves a better immediate surgical effect with more favorable cost-effectiveness.
Keyword
MeSH Terms
Figure
Reference
-
1. Alvarez L, Pérez-Higueras A, Granizo JJ, de Miguel I, Quiñones D, Rossi RE. Predictors of outcomes of percutaneous vertebroplasty for osteoporotic vertebral fractures. Spine (Phila Pa 1976). 2005; 30:87–92. PMID: 15626987.
Article2. Anselmetti GC, Corrao G, Monica PD, Tartaglia V, Manca A, Eminefendic H, et al. Pain relief following percutaneous vertebroplasty : results of a series of 283 consecutive patients treated in a single institution. Cardiovasc Intervent Radiol. 2007; 30:441–447. PMID: 17200900.
Article3. Barr JD, Barr MS, Lemley TJ, McCann RM. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine (Phila Pa 1976). 2000; 25:923–928. PMID: 10767803.
Article4. Erkan S, Ozalp TR, Yercan HS, Okcu G. Does timing matter in performing kyphoplasty? Acute versus chronic compression fractures. Acta Orthop Belg. 2009; 75:396–404. PMID: 19681328.5. Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res. 1993; 8:1137–1148. PMID: 8237484.
Article6. Haynes SR, Lawler PG. An assessment of the consistency of ASA physical status classification allocation. Anaesthesia. 1995; 50:195–199. PMID: 7717481.
Article7. Kaufmann TJ, Jensen ME, Schweickert PA, Marx WF, Kallmes DF. Age of fracture and clinical outcomes of percutaneous vertebroplasty. AJNR Am J Neuroradiol. 2001; 22:1860–1863. PMID: 11733316.8. Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J. 2006; 6:479–487. PMID: 16934715.
Article9. Kim DJ, Kim TW, Park KH, Chi MP, Kim JO. The proper volume and distribution of cement augmentation on percutaneous vertebroplasty. J Korean Neurosurg Soc. 2010; 48:125–128. PMID: 20856660.
Article10. Klazen CA, Lohle PN, de Vries J, Jansen FH, Tielbeek AV, Blonk MC, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II) : an open-label randomised trial. Lancet. 2010; 376:1085–1092. PMID: 20701962.
Article11. Liebschner MA, Rosenberg WS, Keaveny TM. Effects of bone cement volume and distribution on vertebral stiffness after vertebroplasty. Spine (Phila Pa 1976). 2001; 26:1547–1554. PMID: 11462084.
Article12. Lin EP, Ekholm S, Hiwatashi A, Westesson PL. Vertebroplasty : cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol. 2004; 25:175–180. PMID: 14970015.13. McGraw JK, Cardella J, Barr JD, Mathis JM, Sanchez O, Schwartzberg MS, et al. Society of Interventional Radiology quality improvement guidelines for percutaneous vertebroplasty. J Vasc Interv Radiol. 2003; 14(9 Pt 2):S311–S315. PMID: 14514838.
Article14. Mellish RW, Garrahan NJ, Compston JE. Age-related changes in trabecular width and spacing in human iliac crest biopsies. Bone Miner. 1989; 6:331–338. PMID: 2758161.
Article15. Nieuwenhuijse MJ, Muijs SP, van Erkel AR, Dijkstra SP. A clinical comparative study on low versus medium viscosity polymethylmetacrylate bone cement in percutaneous vertebroplasty : viscosity associated with cement leakage. Spine (Phila Pa 1976). 2010; 35:E1037–E1044. PMID: 20802393.16. Norbert B, Mas A. Spinal disorders, Fundamentals of diagnosis and treatment. ed 1. New York: Springer;2008. p. 938.17. Peh WC, Gilula LA. Percutaneous vertebroplasty : indications, contraindications, and technique. Br J Radiol. 2003; 76:69–75. PMID: 12595329.
Article18. Rad AE, Kallmes DF. Correlation between preoperative pain duration and percutaneous vertebroplasty outcome. AJNR Am J Neuroradiol. 2011; 32:1842–1845. PMID: 21852369.
Article19. USFDA. Guidance for Industry and FDA Staff - Clinical Trial Considerations : Vertebral Augmentation Devices to Treat Spinal Insufficiency Fractures. Silverspring: US FDA;2004.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vertebroplasty in the Multiple Osteoporotic Compression Fracture
- Pyogenic Spondylitis after Vertebroplasty: A Report of Two Cases
- Short-term Treatment Comparison of Teriparatide and Percutaneous Vertebroplasty in Patients with Acute Osteoporotic Vertebral Compression Fractures
- The effect of percutaneous vertebroplasty with bone cement in the treatment of osteoporotic thoracolumbar compression fracture
- The Effect of Early Percutaneous Vertebroplasty in Occult Osteoporotic Vertebral Fracture