J Korean Neurosurg Soc.
2014 Sep;56(3):188-193. 10.3340/jkns.2014.56.3.188.
Preliminary Study of Neurocognitive Dysfunction in Adult Moyamoya Disease and Improvement after Superficial Temporal Artery-Middle Cerebral Artery Bypass
- Affiliations
-
- 1Department of Neurosurgery, Eulji University Hospital, College of Medicine, Eulji University, Daejeon, Korea. neurocsy@eulji.ac.kr
- KMID: 2339955
- DOI: http://doi.org/10.3340/jkns.2014.56.3.188
Abstract
OBJECTIVE
Moyamoya disease (MMD) is a chronic cerebrovascular occlusive disease of unknown etiology. In addition, the neurocognitive impairment of adults with MMD is infrequently reported and, to date, has not been well described. We attempted to determine both the neurocognitive profile of adult moyamoya disease and whether a superficial temporal artery-middle cerebral artery (STA-MCA) anastomosis can improve the neurocognitive impairment in exhibiting hemodynamic disturbance without stroke.
METHODS
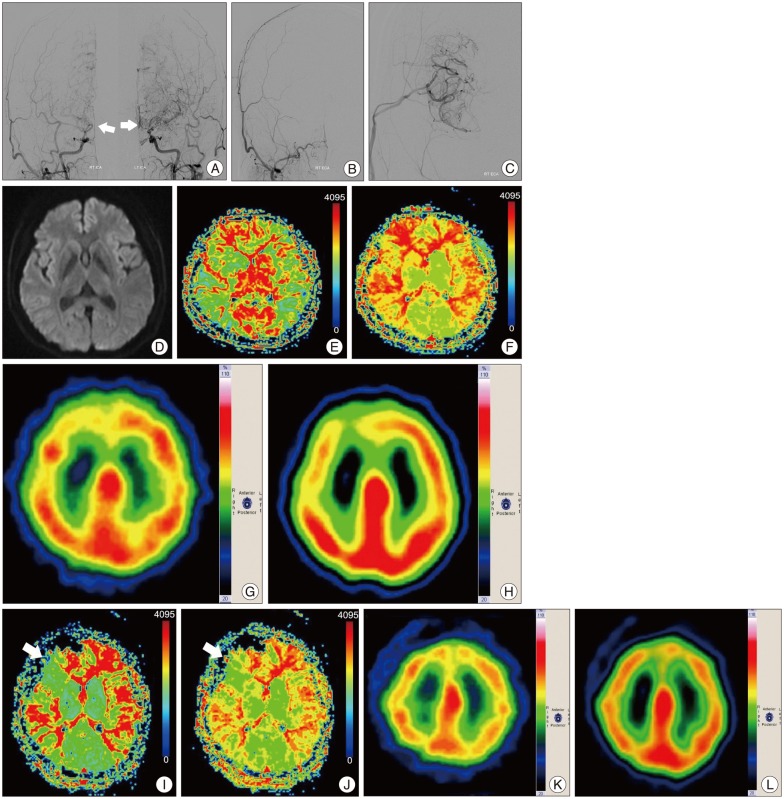
From September 2010 through November 2012, 12 patients with angiographically diagnosed MMD underwent STA-MCA anastomosis for hemodynamic impairment. Patients with hypoperfusion and impaired cerebrovascular reserve (CVR) capacity but without evidence of ischemic stroke underwent a cognitive function test, the Seoul Neuropsychological Screening Battery (SNSB). Five patients agreed to undergo a follow-up SNSB test. Data from preoperative and postoperative neurocognitive function tests were compared and analyzed.
RESULTS
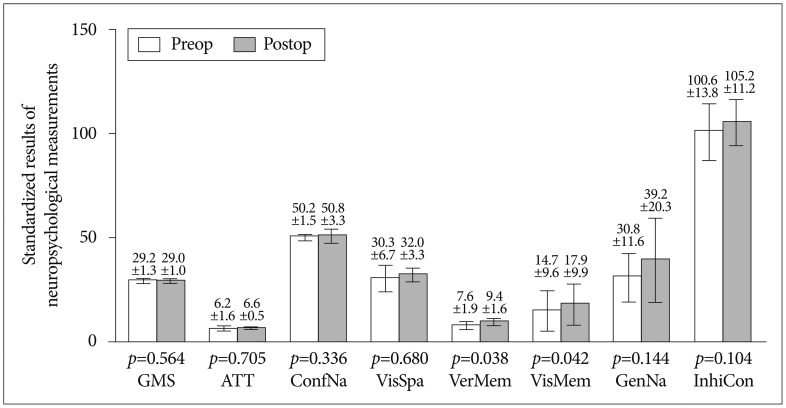
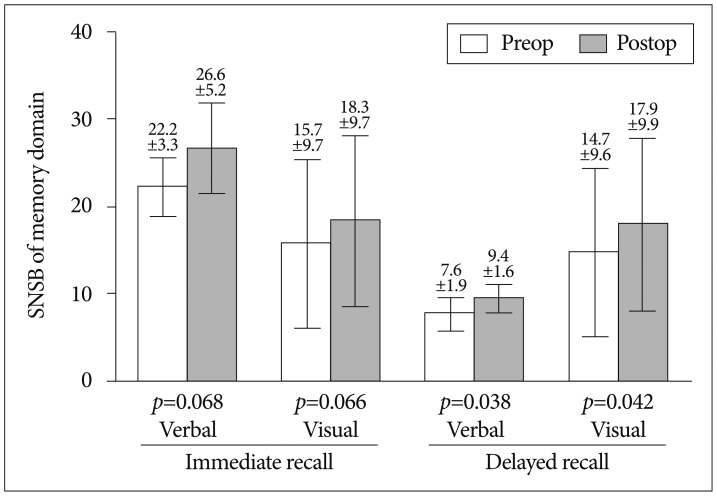
Five of 12 patients were enrolled. The median age was 45 years (range, 24-55 years). A comparison of preoperative to postoperative status of SNSB, memory domain, especially delayed recall showed significant improvement. Although most of the domains showed improvement after surgery, the results were not statistically significant.
CONCLUSION
In our preliminary study, large proportions of adult patients with MMD demonstrate disruption of cognitive function. This suggests the possibility of chronic hypoperfusion as a primary cause of the neurocognitive impairment. When preoperative and postoperative status of cognitive function was compared, memory domain showed remarkable improvement. Although further study is needed, neurocognitive impairment may be an indication for earlier intervention with reperfusion procedures that can improve cognitive function.
MeSH Terms
Figure
Reference
-
1. Calviere L, Catalaa I, Marlats F, Viguier A, Bonneville F, Cognard C, et al. Correlation between cognitive impairment and cerebral hemodynamic disturbances on perfusion magnetic resonance imaging in European adults with moyamoya disease. Clinical article. J Neurosurg. 2010; 113:753–759. PMID: 20469988.
Article2. Chang KH, Yi JG, Han MH, Kim IO. MR imaging findings of moyamoya disease. J Korean Med Sci. 1990; 5:85–90. PMID: 2278666.
Article3. Fujii K, Ikezaki K, Irikura K, Miyasaka Y, Fukui M. The efficacy of bypass surgery for the patients with hemorrhagic moyamoya disease. Clin Neurol Neurosurg. 1997; 99(Suppl 2):S194–S195. PMID: 9409436.
Article4. Fukui M, Kono S, Sueishi K, Ikezaki K. Moyamoya disease. Neuropathology. 2000; 20(Suppl):S61–S64. PMID: 11037190.
Article5. Guzman R, Lee M, Achrol A, Bell-Stephens T, Kelly M, Do HM, et al. Clinical outcome after 450 revascularization procedures for moyamoya disease. Clinical article. J Neurosurg. 2009; 111:927–935. PMID: 19463046.
Article6. Hayashi T, Shirane R, Fujimura M, Tominaga T. Postoperative neurological deterioration in pediatric moyamoya disease : watershed shift and hyperperfusion. J Neurosurg Pediatr. 2010; 6:73–81. PMID: 20593991.
Article7. Hsu YH, Kuo MF, Hua MS, Yang CC. Selective neuropsychological impairments and related clinical factors in children with moyamoya disease of the transient ischemic attack type. Childs Nerv Syst. 2014; 30:441–447. PMID: 24005800.
Article8. Jefferson AL, Glosser G, Detre JA, Sinson G, Liebeskind DS. Neuropsychological and perfusion MR imaging correlates of revascularization in a case of moyamoya syndrome. AJNR Am J Neuroradiol. 2006; 27:98–100. PMID: 16418365.9. Kang Y, Na DL. Seoul Neuropsychological Screening Battery (SNSB). Seoul: Human Brain Research & Consulting Co.;2003.10. Karzmark P, Zeifert PD, Bell-Stephens TE, Steinberg GK, Dorfman LJ. Neurocognitive impairment in adults with moyamoya disease without stroke. Neurosurgery. 2012; 70:634–638. PMID: 21849919.
Article11. Karzmark P, Zeifert PD, Tan S, Dorfman LJ, Bell-Stephens TE, Steinberg GK. Effect of moyamoya disease on neuropsychological functioning in adults. Neurosurgery. 2008; 62:1048–1051. discussion 1051-1052. PMID: 18580802.
Article12. Kuroda S, Ishikawa T, Houkin K, Nanba R, Hokari M, Iwasaki Y. Incidence and clinical features of disease progression in adult moyamoya disease. Stroke. 2005; 36:2148–2153. PMID: 16179571.
Article13. Kwag HJ, Jeong DW, Lee SH, Kim DH, Kim J. Intracranial hemodynamic changes during adult moyamoya disease progression. J Clin Neurol. 2008; 4:67–74. PMID: 19513306.
Article14. Lee JY, Phi JH, Wang KC, Cho BK, Shin MS, Kim SK. Neurocognitive profiles of children with moyamoya disease before and after surgical intervention. Cerebrovasc Dis. 2011; 31:230–237. PMID: 21178347.
Article15. Mogensen MA, Karzmark P, Zeifert PD, Rosenberg J, Marks M, Steinberg GK, et al. Neuroradiologic correlates of cognitive impairment in adult Moyamoya disease. AJNR Am J Neuroradiol. 2012; 33:721–725. PMID: 22173751.
Article16. Nakagawa Y, Abe H, Sawamura Y, Kamiyama H, Gotoh S, Kashiwaba T. Revascularization surgery for moyamoya disease. Neurol Res. 1988; 10:32–39. PMID: 2899853.
Article17. Peerless SJ. Risk factors of moyamoya disease in Canada and the USA. Clin Neurol Neurosurg. 1997; 99(Suppl 2):S45–S48. PMID: 9409404.
Article18. Scott RM, Smith ER. Moyamoya disease and moyamoya syndrome. N Engl J Med. 2009; 360:1226–1237. PMID: 19297575.
Article19. Smith JL. Understanding and treating moyamoya disease in children. Neurosurg Focus. 2009; 26:E4. PMID: 19335128.
Article20. Weinberg DG, Rahme RJ, Aoun SG, Batjer HH, Bendok BR. Moyamoya disease : functional and neurocognitive outcomes in the pediatric and adult populations. Neurosurg Focus. 2011; 30:E21. PMID: 21631223.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Middle Cerebral Artery AneurysmOriginating Near the Site of Anastomosis after Superficial Temporal Artery-Middle Cerebral Artery Bypass: Case Report
- Long-Term Follow-up Study after Superficial Temporal Artery-Middle Cerebral Artery Anastomosis plus Encephalomyosynangiosis for Moyamoya Disease
- Off-Pump Coronary Artery Bypass Grafting in Moyamoya Disease
- Development of Brain Infarction after Extracranial-Intracranial Bypass Surgery in a Patient with Moyamoya Disease: A case report
- Clinical Analysis of Surgically Treated Moyamoya Diseases