J Korean Ophthalmol Soc.
2012 Mar;53(3):372-384.
Analysis of Inpatients with Bacterial Keratitis Over a 12-Year Period: Pathogenic Organisms and Antibiotic Resistance
- Affiliations
-
- 1Department of Ophthalmology, Yeungnam University College of Medicine, Daegu, Korea. sbummlee@med.yu.ac.kr
Abstract
- PURPOSE
To investigate the distribution of bacterial keratitis isolates and the shifting trends of in vitro antibiotic susceptibility of the isolates for inpatients with bacterial keratitis.
METHODS
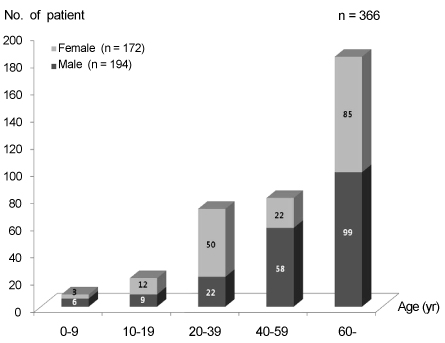
Three hundred ninety-two bacterial isolates with 366 positive culture cases from consecutive corneal scrapes of 988 clinically diagnosed bacterial keratitis inpatients hospitalized at Yeungnam University Hospital between January 1998 and December 2009 were retrospectively reviewed. The bacteriological profiles and in vitro resistance were evaluated in the first and second six-year periods.
RESULTS
The percentage of positive cultures was 37.0% (366/988). The commonly isolated Gram-positive and Gram-negative organisms were S. epidermidis (98; 25.0%) and P. aeruginosa (41; 10.5%), respectively. The ratio of Gram-positive to Gram-negative isolates was 1.24:1. The Gram-positive isolates significantly decreased compared to the Gram-negative isolates in the last six-year period (45.3% versus 54.7%, respectively) relative to those in the first six-year period (66.1% versus 33.9%, respectively). S. epidermidis and S. aureus decreased, and E. cloacae, S. marcescens, and S. maltophilia increased in the last six-year period. The resistance of fluoroquinolone to the Gram-positive isolates, though not statistically significant, tended to increase to 34.1% from 21.5% (p=0.061), and the methicillin-resistant S. aureus tended to increase to 54.2% from 30.0% (p=0.055).
CONCLUSIONS
S. epidermidis and P. aeruginosa were the most common bacterial keratitis isolates in Gram-positive and Gram-negative isolates. The Gram-positive isolates tended to decrease, though the Gram-negative organisms tended to increase in the last six-year period compared to the first six-year period. Empirical antibiotic selection should be based on local susceptibility patterns and distribution of bacterial isolates.
MeSH Terms
Figure
Reference
-
1. Kim YS, Chung WS, Lee SB. The causative organisms and therapy of corneal ulcers. J Korean Ophthalmol Soc. 1994. 35:1171–1177.2. Park JH, Lee SB. Analysis on inpatients with infectious keratitis: causative organisms, clinical aspects and risk factors. J Korean Ophthalmol Soc. 2009. 50:1152–1166.3. Levey SB, Katz HR, Abrams DA, et al. The role of cultures in the management of ulcerative keratitis. Cornea. 1997. 16:383–386.4. Schaefer F, Bruttin O, Zografos L, Guex-Crosier Y. Bacterial keratitis: a prospective clinical and microbiological study. Br J Ophthalmol. 2001. 85:842–847.5. Armstrong RA. The microbiology of the eye. Ophthalmic Physiol Opt. 2000. 20:429–441.6. Leck AK, Thomas PA, Hagan M, et al. Aetiology of suppurative corneal ulcers in Ghana and south India, and epidemiology of fungal keratitis. Br J Ophthalmol. 2002. 86:1211–1215.7. Hahn YH, Lee SJ, Hahn TW, et al. Antibiotic susceptibilities of ocular isolates from patients with bacterial keratitis: a multi-center study. J Korean Ophthalmol Soc. 1999. 40:2401–2410.8. Jones DB. Decision-making in the management of microbial keratitis. Ophthalmology. 1981. 88:814–820.9. Baum JL. Initial therapy of suspected microbial corneal ulcers. I. Broad antibiotic therapy based on prevalence of organisms. Surv Ophthalmol. 1979. 24:97–105.10. Humphreys H, Mulvihill E. Ciprofloxacin-resistant Staphylococcus aureus. Lancet. 1985. 2:383.11. George RC, Ball LC, Norbury PB. Susceptibility to ciprofloxacin of nosocomial gram-negative bacteria and staphylococci isolated in the UK. J Antimicrob Chemother. 1990. 26:145–156.12. Raviglione MC, Boyle JF, Mariuz P, et al. Ciprofloxacin-resistant methicillin-resistant Staphylococcus aureus in an acute-care hospital. Antimicrob Agents Chemother. 1990. 34:2050–2054.13. Alexandrakis G, Alfonso EC, Miller D. Shifting trends in bacterial keratitis in south Florida and emerging resistance to fluoroquinolones. Ophthalmology. 2000. 107:1497–1502.14. Kunimoto DY, Sharma S, Garg P, Rao GN. In vitro susceptibility of bacterial keratitis pathogens to ciprofloxacin. Emerging resistance. Ophthalmology. 1999. 106:80–85.15. Garg P, Sharma S, Rao GN. Ciprofloxacin-resistant Pseudomonas keratitis. Ophthalmology. 1999. 106:1319–1323.16. Srinivasan M, Gonzales CA, George C, et al. Epidemiology and aetiological diagnosis of corneal ulceration in Madurai, south India. Br J Ophthalmol. 1997. 81:965–971.17. Yeh DL, Stinnett SS, Afshari NA. Analysis of bacterial cultures in infectious keratitis, 1997 to 2004. Am J Ophthalmol. 2006. 142:1066–1068.18. Zhang C, Liang Y, Deng S, et al. Distribution of bacterial keratitis and emerging resistance to antibiotics in China from 2001 to 2004. Clin Ophthalmol. 2008. 2:575–579.19. Toshida H, Kogure N, Inoue N, Murakami A. Trends in microbial keratitis in Japan. Eye Contact Lens. 2007. 33:70–73.20. Liesegang TJ, Forster RK. Spectrum of microbial keratitis in South Florida. Am J Ophthalmol. 1980. 90:38–47.21. Ahn M, Jung YT, Han HJ. A clinical study on infectious corneal ulcer. J Korean Ophthalmol Soc. 1996. 37:1538–1543.22. Kim WJ, Kweon EY, Lee DW, et al. Prognostic factor and antibiotic susceptibility in bacterial keratitis: results of an eight-year period. J Korean Ophthalmol Soc. 2009. 50:1495–1504.23. Lee WC, Lee SY. National health screening program of Korea. J Korean Med Assoc. 2010. 53:363–370.24. Kirkendall WM, Hammond JJ. Hypertension in the elderly. Arch Intern Med. 1980. 140:1155–1161.25. Biemer JJ. Antimicrobial susceptibility testing by the Kirby-Bauer disc diffusion method. Ann Clin Lab Sci. 1973. 3:135–140.26. Jorgensen JH, Hindler JF. New consensus guidelines from the Clinical and Laboratory Standards Institute for antimicrobial susceptibility testing of infrequently isolated or fastidious bacteria. Clin Infect Dis. 2007. 44:280–286.27. Shin SY, Koo SH, Kwon KC, et al. Evaluation of the Vitek 2 korean antimicrobial susceptibility testing cards AST N056 and AST N055. Korean J Clin Microbiol. 2008. 11:23–28.28. Sun X, Deng S, Li R, et al. Distribution and shifting trends of bacterial keratitis in north China (1989-98). Br J Ophthalmol. 2004. 88:165–166.29. Bourcier T, Thomas F, Borderie V, et al. Bacterial keratitis: predisposing factors, clinical and microbiological review of 300 cases. Br J Ophthalmol. 2003. 87:834–838.30. Sun HJ, Lee JY, Kim SY, Jung MS. Clinical features of infectious keratits in west coast area of Chungcheongnam-do, Korea. J Korean Ophthalmol Soc. 2010. 51:658–663.31. Tuft SJ, Matheson M. In vitro antibiotic resistance in bacterial keratitis in London. Br J Ophthalmol. 2000. 84:687–691.32. Fong CF, Hu FR, Tseng CH, et al. Antibiotic susceptibility of bacterial isolates from bacterial keratitis cases in a university hospital in Taiwan. Am J Ophthalmol. 2007. 144:682–689.33. Potron A, Poirel L, Bernabeu S, et al. Nosocomial spread of ESBL-positive Enterobacter cloacae co-expressing plasmid-mediated quinolone resistance Qnr determinants in one hospital in France. J Antimicrob Chemother. 2009. 64:653–654.34. Ahn GS, Hahn YH, Lee HB. Serratia marcescens keratitis. J Korean Ophthalmol Soc. 2002. 43:658–664.35. Cheng KH, Leung SL, Hoekman HW, et al. Incidence of contact-lens-associated microbial keratitis and its related morbidity. Lancet. 1999. 354:181–185.36. You IC, Lee SH, Park YG, Yoon KC. Clinical aspect and prognosis of Stenotrophomonas (Xanthomonas) Maltophilia keratitis. J Korean Ophthalmol Soc. 2007. 48:889–897.37. Jensen HG, Felix C. In Vitro Antibiotic Testing Group. In vitro antibiotic susceptibilities of ocular isolates in North and South America. Cornea. 1998. 17:79–87.38. Bower KS, Kowalski RP, Gordon YJ. Fluoroquinolones in the treatment of bacterial keratitis. Am J Ophthalmol. 1996. 121:712–715.39. Kim DH, Stark WJ, O'Brien TP, Dick JD. Aqueous penetration and biological activity of moxifloxacin 0.5% ophthalmic solution and gatifloxacin 0.3% solution in cataract surgery patients. Ophthalmology. 2005. 112:1992–1996.40. Lai WW, Chu KO, Chan KP, et al. Differential aqueous and vitreous concentrations of moxifloxacin and ofloxacin after topical administration one hour before vitrectomy. Am J Ophthalmol. 2007. 144:315–318.41. Mather R, Karenchak LM, Romanowski EG, Kowalski RP. Fourth generation fluoroquinolones: new weapons in the arsenal of ophthalmic antibiotics. Am J Ophthalmol. 2002. 133:463–466.42. Smitha S, Lalitha P, Prajna VN, Srinivasan M. Susceptibility trends of pseudomonas species from corneal ulcers. Indian J Med Microbiol. 2005. 23:168–171.43. Keseru JS, Gál Z, Barabás G, et al. Investigation of beta-Lactamases in clinical isolates of Staphylococcus aureus for further explanation of borderline methicillin resistance. Chemotherapy. 2005. 51:300–304.44. Fontana R, Aldegheri M, Ligozzi M, et al. Overproduction of a low-affinity penicillin-binding protein and high-level ampicillin resistance in Enterococcus faecium. Antimicrob Agents Chemother. 1994. 38:1980–1983.45. Ly CN, Pham JN, Badenoch PR, et al. Bacteria commonly isolated from keratitis specimens retain antibiotic susceptibility to fluoroquinolones and gentamicin plus cephalothin. Clin Experiment Ophthalmol. 2006. 34:44–50.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical and Microbiological Analysis of Gram-Positive Bacterial Keratitis, a 15-Year Review
- The Resistance to Ciprofloxacin in Bacterial Ocular Disease
- Antibiotics Susceptibility in Bacterial Keratitis and Proper Initial Treatment
- The Cultured Organisms and In Vitro Antibiotic Sensitivity of Ocular Bacterial Infection
- Gram-Negative Bacterial Keratitis: A 15-Year Review of Clinical Aspects