J Korean Ophthalmol Soc.
2007 Nov;48(11):1479-1486.
Changes in Anterior Chamber Depth and Refraction after Accommodative Intraocular Lens Implantation
- Affiliations
-
- 1Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. tychung@smc.samsung.co.kr
Abstract
-
PURPOSE: To evaluate the change in anterior chamber depth and refraction after AT-45 implantation
METHODS
Twenty-two eyes from 22 patients were enrolled in this prospective study. After phacoemulsification, AT-45 (11 eyes) and SA60AT (11 eyes) were implanted. Clinical data included anterior chamber depth and refractive error at 1 week, 1 month, 2 months and 6 months postoperatively. The correlation between anterior chamber depth change and spherical equivalent change was also evaluated.
RESULTS
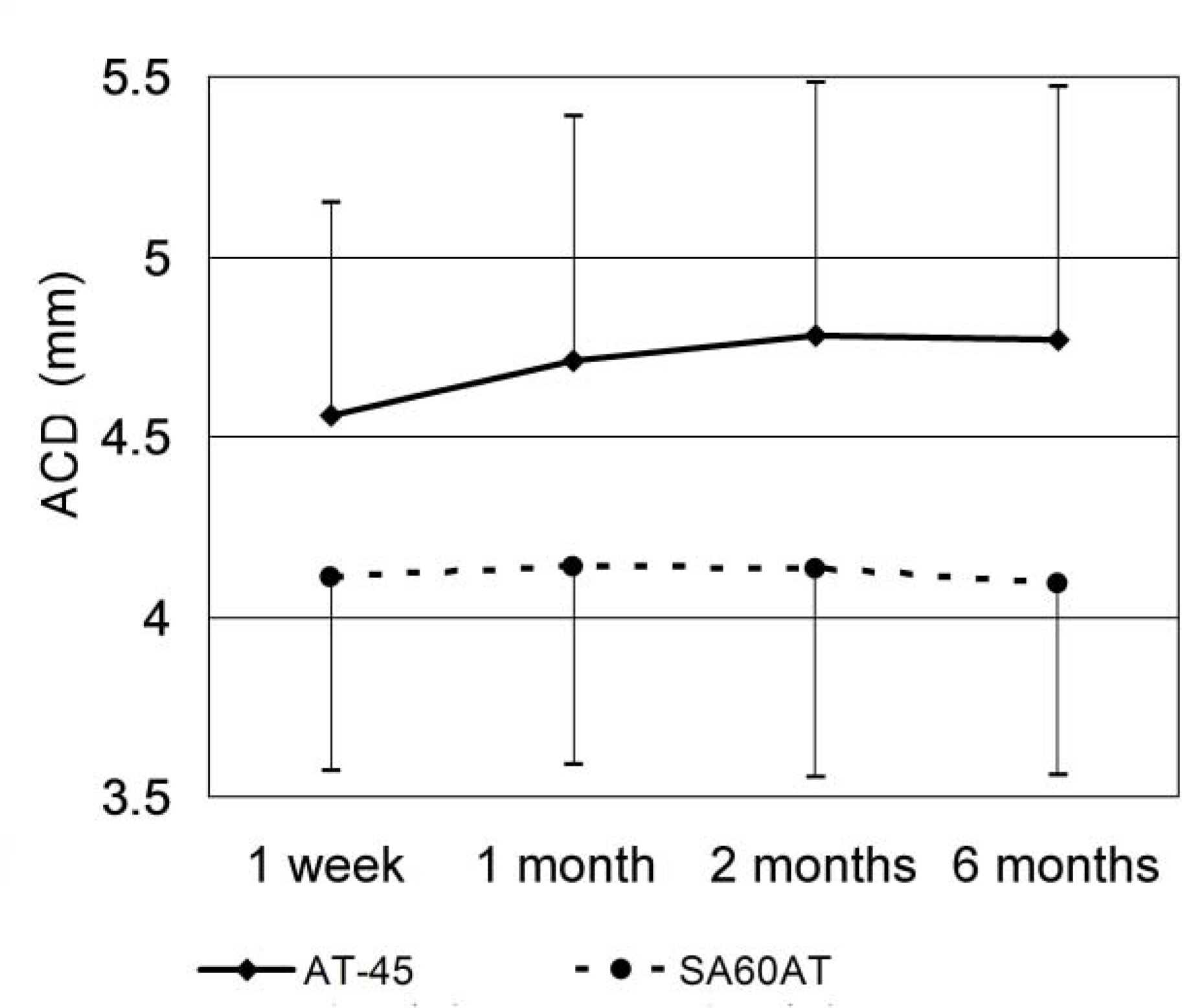
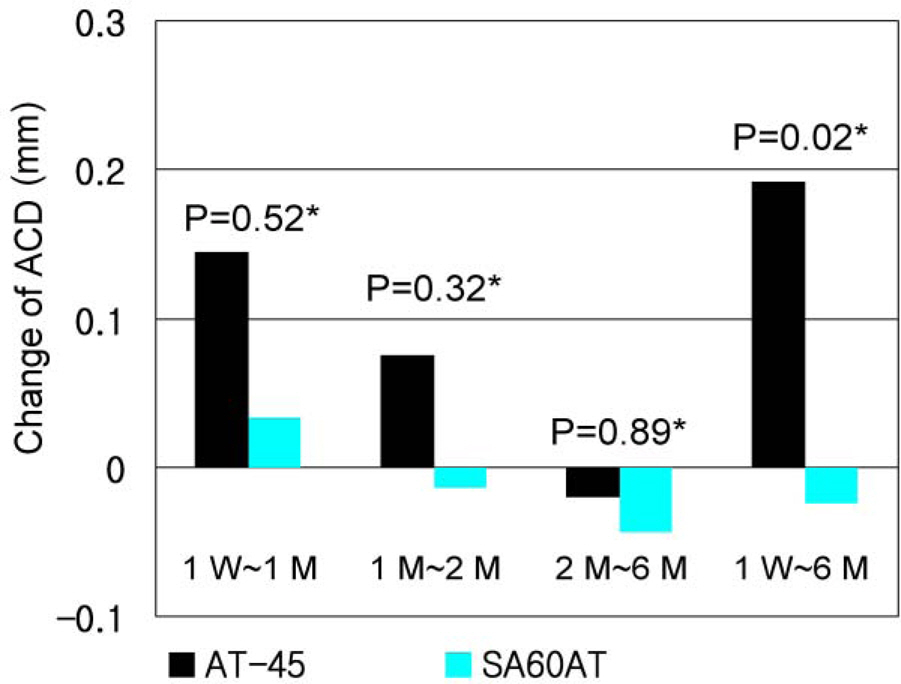
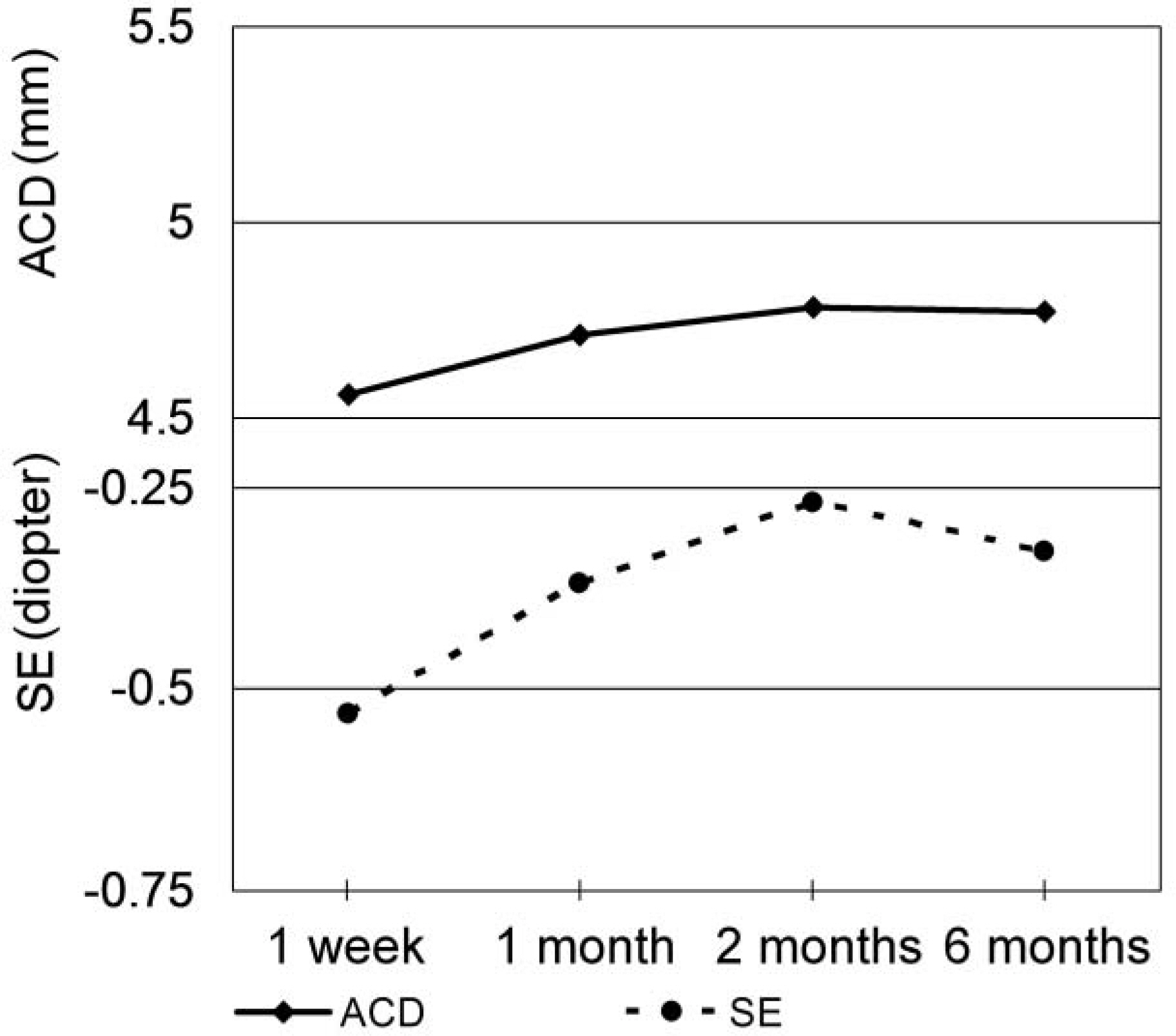
In the AT-45 implanted group, the mean anterior chamber depth was 4.56+/-0.59 mm at 1 week postoperative, 4.70+/-0.69 mm at 1 month postoperative, 4.78+/-0.71 mm at 2 months postoperative and 4.76+/-0.69 mm at 6 months postoperative. The mean spherical equivalent was -0.53+/-0.48D, -0.37+/-0.42D, -0.27+/-0.47D, and -0.33+/-0.44D respectively. When analyzed using the Mann-Whitney U test, p-values of anterior chamber depth differences between the 2 groups were P=0.52 at 1 week to 1 month, P=0.32 at 1 month to 2 months, P=0.89 at 2 months to 6 months, and P=0.02 at 1 week to 6 months, showing a deeper anterior chamber in the AT-45 implanted group. P-values (Mann-Whitney U test) of spherical equivalent differences between the 2 groups were P=0.33, P=0.56, P=0.94, and P=0.19, respectively, showing more hyperopic change in the AT-45 implanted group. The correlation between anterior chamber depth change and spherical equivalent change in the AT-45 implanted group at 1 week to 6 months was not statistically significant (Spearman correlation analysis, P=0.223).
CONCLUSIONS
Anterior chamber depth deepening and associated hyperopic refractive change were observed after AT-45 implantation, especially at 1 month after the surgery.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Im YW, Lee KH, Park SC. The differences of the near visual acuity between multifocal IOL and monofocal IOL. J Korean Ophthalmol Soc. 1994; 35:1027–32.2. Hayashi K, Hayashi H, Nakao F, Hayashi F. Aging changes in apparent accommodation in eyes with a monofocal intraocular lens. Am J Ophthalmol. 2003; 135:432–6.
Article3. Kuchle M, Langenbucher A, Gusek-Schneider GC, et al. First results of implantation of a new, potentially accommodative posterior chamber intraocular lens. Klin Monatsbl Augenheilkd. 2001; 218:603–8.4. Kuchle M, Seitz B, Langenbucher A, et al. Comparison of 6-month results of implantation of the 1CU accommodative intraocular lens with conventional intraocular lenses. Ophthalmology. 2004; 111:318–24.
Article5. Hara T, Hara T, Yasuda A, Yamada Y. Accommodative intraocular lens with spring action-part 1: design and placement in an excised animal eye. Ophthalmic Surg. 1990; 21:128–33.6. Hara T, Hara T, Yasuda A, et al. Accommodative intraocular lens with spring action-part 2: fixation in the living rabbit. Ophthalmic Surg. 1992; 23:632–5.
Article7. McLeod SD, Portney V, Ting A. A dual optic accommodating foldable intraocular lens. Br J Ophthalmol. 2003; 87:1083–5.
Article8. Cumming JS, Slade SG, Chayet A. Clinical evaluation of the model AT-45 silicone accommodating intraocular lens. Ophthalmology. 2001; 108:2005–10.9. Coleman PJ. On the hydraulic suspension theory of accommodation. Trans Am Ophthalmol Soc. 1986; 84:846–68.10. Strenk SA, Semmlow JL, Strenk LM, et al. Age-related changes in human ciliary muscle and lens: a magnetic resonance imaging study. Invest Ophthalmol Vis Sci. 1999; 40:1162–9.11. Cumming JS, Ritter JA. The measurement of vitreous cavity length and its comparison pre- and postoperatively. Eur J Implant Refract Surg. 1994; 6:261–72.
Article12. Kim JH, Park JS, Chung TY, Chung ES. Clinical evaluation of AT-45 implantation. J Korean Ophthalmol Soc. 2007; 48:368–75.13. Nejima R, Miyai T, Kataoka Y, et al. Prospective intrapatient comparison of 6.0-millimeter optic single-piece and 3-piece hydrophobic acrylic foldable intraocular lenses. Ophthalmology. 2006; 113:585–90.
Article14. Cazal J, Lavin-Dapena C, Marin J, Verges C. Accommodative intraocular lens tilting. Am J Ophthalmol. 2005; 140:341–4.
Article15. Cumming JS, Colvard DM, Dell SJ, et al. Clinical evaluation of the Crystalens AT-45 accommodating intraocular lens: results of the U.S. Food and Drug Administration clinical trial. J Cataract Refract Surg. 2006; 32:812–25.16. Alio JL, Tavolato M, De la Hoz F, et al. Near vision restoration with refractive lens exchange and pseudoaccommodating and multifocal refractive and diffractive intraocular lenses: comparative clinical study. J Cataract Refract Surg. 2004; 30:2494–503.17. Marchini G, Pedrotti E, Sartori P, Tosi R. Ultrasound biomicroscopic changes during accommodation in eyes with accommodating intraocular lenses: pilot study and hypothesis for the mechanism of accommodation. J Cataract Refract Surg. 2004; 30:2476–82.18. Lee DY, Ahn CS. Statistical study of the ocular dimensions on refractive error. J Korean Ophthalmol Soc. 1994; 35:1137–46.19. Kim CS, Kim MY, Kim HS, Lee YC. Change of corneal astigmatism with aging in Koreans with normal visual acuity. J Korean Ophthalmol Soc. 2002; 43:1956–62.20. Foster PJ, Baasanhu J, Alsbirk PH, et al. Central corneal thickness and intraocular pressure in a Mongolian population. Ophthalmology. 1998; 105:969–73.
Article21. La Rosa FA, Gross RL, Orengo-Nania S. Central corneal thickness of Caucasians and African Americans in glaucomatous and nonglaucomatous populations. Arch Ophthalmol. 2001; 119:23–7.22. Yo C, Ariyasu RG. Racial differences in central corneal thickness and refraction among refractive surgery candidates. J Refract Surg. 2005; 21:194–7.
Article23. Clemmesen V, Olurin O. Lens thickness in western Nigeria. A comparative ultrasonic study in Negros and Danes. Acta Ophthalmol. 1985; 63:274–6.24. Wojciechowski R, Congdon N, Anninger W, Teo Broman A. Age, gender, biometry, refractive error, and the anterior chamber angle among Alaskan Eskimos. Ophthalmology. 2003; 110:365–75.
Article25. Stachs O, Schneider H, Stave J, Guthoff R. Potentially accommodating intraocular lenses-an in vitro and in vivo study using three-dimensional high-frequency ultrasound. J Refract Surg. 2005; 21:37–45.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diurnal Variation in the Depth of the Anterior Chamber and Correlation between the Depth of the Anterior Chamber and Intraocular Pressure
- Predictability of Postoperative Refractive Error after Secondary Lens Implantation
- Clinical Results on Intraocular Lens Implantation
- Intraocular Pressure Changes in the Uneventful Extra-capsular Cataract Extraction and Extra-capsular Cataract Extraction with Vitreous Loss followed by Anterior Chamber Lens Implantation
- Transecleral Suture Fixation for a Posterior Chamber Intraocular Lens Implantation