J Korean Rheum Assoc.
2009 Sep;16(3):248-252.
Renal Artery Thrombosis in a Patient with Systemic Lupus Erythematosus without Antiphospholipid Antibody Syndrome: A Case Study
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, Jeju National University, Jeju, Korea. slera@cheju.ac.kr
- 2Department of Radiology, College of Medicine, Jeju National University, Jeju, Korea.
Abstract
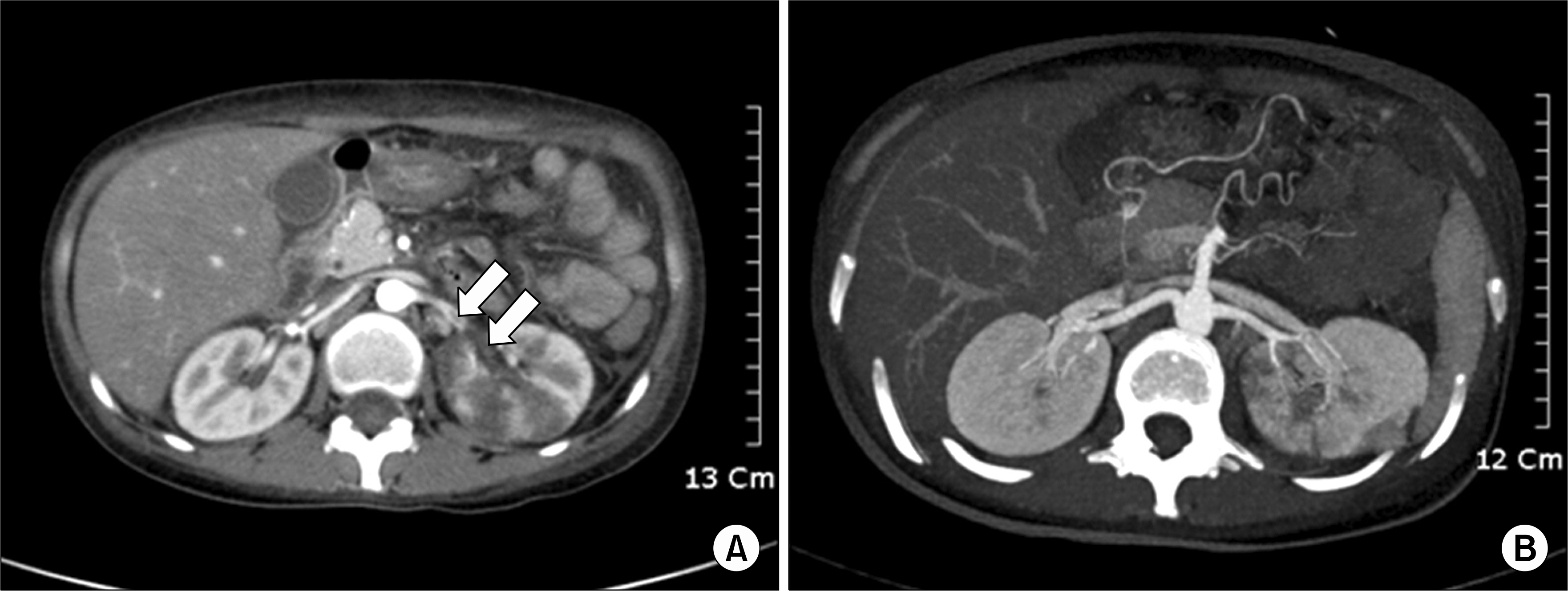
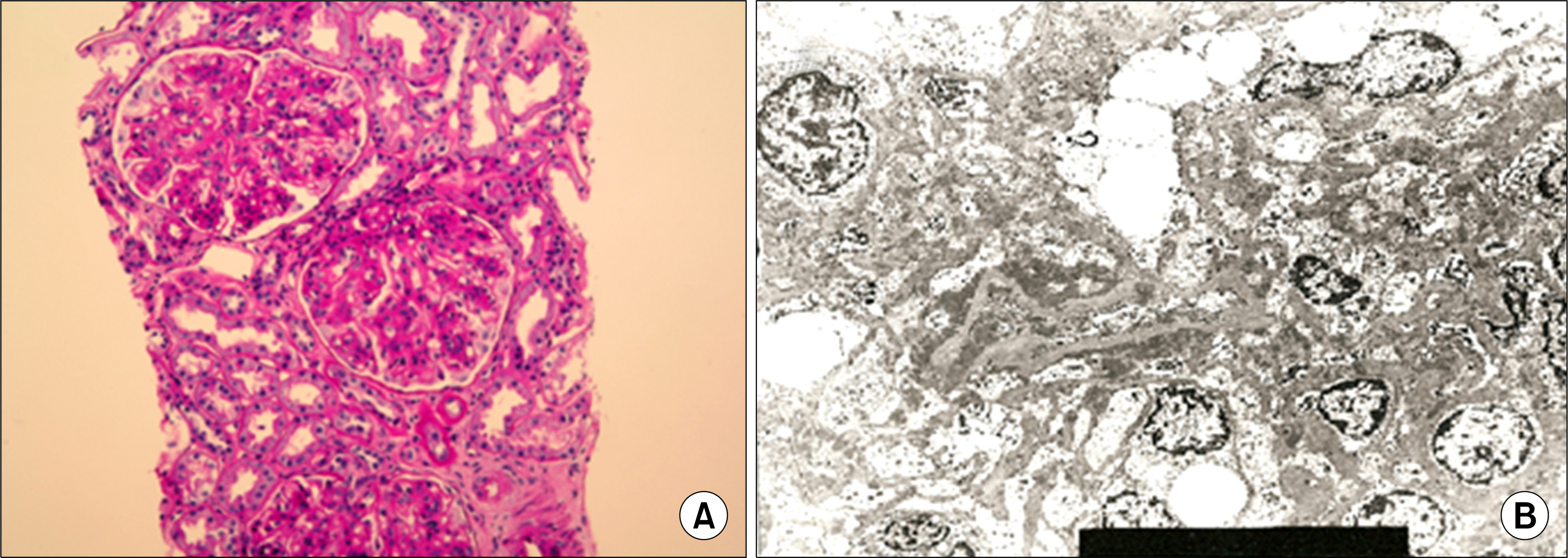
- Systemic lupus erythematosus (SLE) is a multisystemic inflammatory autoimmune disease caused by various autoantibodies and immune complexes. SLE and antiphospholipid antibodies are associated with thrombotic manifestations. However, renal artery thrombosis which causes renal artery occlusion is uncommon even in SLE patients with antiphospholipid antibodies. A 27-year-old woman with SLE suddenly developed left flank pain and generalized edema. From the laboratory workup, the woman was negative for antiphospholipid antibody and nephrotic-range proteinuria was detected. Computed tomography revealed renal artery thromboembolism and multiple renal infarctions with parenchymal perfusion defects in the left kidney. Renal biopsy showed WHO classification III and V lupus nephritis. Left flank pain, generalized edema and proteinuria were resolved and the thromboembolism resolved itself after a high dose of steroid and anticoagulation therapy. In SLE patients, sudden onset of unexplained flank pain is considered as a possible symptom of renal vessel thromboembolism even if the antiphospholipid antibody is negative.
MeSH Terms
-
Adult
Antibodies, Antiphospholipid
Antigen-Antibody Complex
Autoantibodies
Autoimmune Diseases
Biopsy
Edema
Female
Flank Pain
Glycosaminoglycans
Humans
Infarction
Kidney
Lupus Erythematosus, Systemic
Lupus Nephritis
Perfusion
Proteinuria
Renal Artery
Thromboembolism
Thrombosis
Antibodies, Antiphospholipid
Antigen-Antibody Complex
Autoantibodies
Glycosaminoglycans
Figure
Reference
-
References
1. Mok CC, Tang SS, To CH, Petri M. Incidence and risk factors of thromboembolism in systemic lupus erythematosus: a comparison of three ethnic groups. Arthritis Rheum. 2005; 52:2774–82.
Article2. Appel GB, Pirani CL, D'Agati V. Renal vascular complications of systemic lupus erythematosus. J Am Soc Nephrol. 1994; 4:1499–515.
Article3. Frostegard J. SLE, atherosclerosis and cardiovascular disease. J Intern Med. 2005; 257:485–95.
Article4. Tsugawa K, Tanaka H, Kudo M, Nakahata T. Renal artery thrombosis in a pediatric case of systemic lupus erythematosus without antiphospholipid antibodies. Pediatr Nephrol. 2005; 20:1648–50.
Article5. Suwabe H, Moriuchi J, Hoshina Y. Renal and cerebral infarctions in a patient with systemic lupus erythematosus without antiphospholipid antibodies. Ryumachi. 1993; 33:335–40.6. Hall S, Buettner H, Luthra HS. Occlusive retinal vascular disease in systemic lupus erythematosus. J Rheumatol. 1984; 11:846–50.7. Nikpour M, Urowitz MB, Gladman DD. Premature atherosclerosis in systemic lupus erythematosus. Rheum Dis Clin North Am. 2005; 31:329–54.
Article8. Asherson RA, Derksen RH, Harris EN, Bouma BN, Gharavi AE, Kater L, et al. Chorea in systemic lupus erythematosus and "lupus-like" disease: association with antiphospholipid antibodies. Semin Arthritis Rheum. 1987; 16:253–9.
Article9. Hernandez D, Dominquez ML, Diaz F, Fernandez ML, Lorenzo V, Rodriquez A, et al. Renal infarction in a severely hypertensive patient with lupus erythematosus and antiphospholipid antibodies. Nephron. 1996; 72:298–301.
Article10. Laskin CA, Clark CA, Spitzer KA. Antiphospholipid syndrome in systemic lupus erythematosus: is the whole greater than the sum of its parts? Rheum Dis Clin North Am. 2005; 31:255–72.
Article11. Soltesz P, Veres K, Lakos G, Kiss E, Muszbek L, Szeqedi G. Evaluation of clinical and laboratory features of antiphospholipid syndrome: a retrospective study of 637 patients. Lupus. 2003; 12:302–7.12. Raij L, Shultz PJ. Endothelium-derived relaxing factor, nitric oxide: effects on and production by mesangial cells and the glomerulus. J Am Soc Nephrol. 1993; 3:1435–41.
Article13. Ross R. Atherosclerosis–an inflammatory disease. N Engl J Med. 1999; 340:115–26.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Leg Ulcer with SLE and Antiphospholipid Syndrome
- A case of Limited Scleroderma Associated with Antiphospholipid Syndrome
- A Case of Systemic Lupus Erythematosus and Secondary AntiphospholipidSyndrome Presenting as Livedo Reticularis
- A Case of Systemic Lupus Erythematosus and Abdominal Aorta Thrombosis Associated with Protein C and S Deficiency
- Antiphospholipid Syndrome Associated with Adenocarcinoma