J Korean Diabetes Assoc.
2006 Nov;30(6):450-458.
Randomized, Open Label, Multicenter Clinical Trial about the Effect of Cilazapril on Vascular Endothelial Function in Patients with Type 2 Diabetes Combined with Hypertension
- Affiliations
-
- 1Department of Endocrinology and Metabolism, Kyung Hee University, Korea.
- 2Department of Endocrinology and Metabolism, Korea University, Korea.
- 3Department of Endocrinology and Metabolism, Young Nam University, Korea.
- 4Department of Endocrinology and Metabolism, Kyung Pook National University, Korea.
- 5Department of Endocrinology and Metabolism, Keimyung University, Korea.
- 6Department of Endocrinology and Metabolism, Sung Kyun Kwan University, Korea.
- 7Department of Endocrinology and Metabolism, Choong Nam National University, Korea.
- 8Department of Endocrinology and Metabolism, Won Kwang University, Korea.
- 9Department of Endocrinology and Metabolism, Yonsei University, Korea.
Abstract
-
BACKGROUND: The angiotensin converting enzyme inhibitor (ACEi) improves the vascular endothelial cell function and has a better clinical outcome by decreasing the LDL cholesterol oxidation, hypercoagulability, oxidative stress and improving the level of endothelial nitric oxide synthesis in patients with type 2 diabetes and hypertension. However, the correlations between the ACEi and the serum markers for the vascular endothelial function in previous studies were not consistent.
SUBJECTS AND METHODS
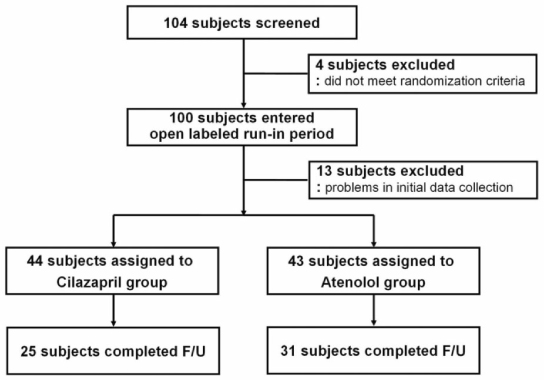
Between July 2003 and April 2005, 104 type 2 diabetes patients with hypertension, who had been admitted to 9 major university hospitals in Korea, were examined. The subjects were randomly allocated to the cilazapril (2.5~5 mg/day) and atenolol (50~100 mg/day) treatment group and given a combination of hydrochlorothiazide and amlodipine. The lipid profile and the markers for endothelial function, such as vWF, VCAM, E-selectin, tPA, fibrinogen, adiponectin, hsCRP, nitrotyrosine were evaluated and the differences in the variables were compared with those obtained 6 months later.
RESULTS
A total 56 subjects completed the 6-months follow up period. Regarding the baseline characteristics, there were no significant differences in the variables observed in the two groups except for HbA1c (P = 0.037), vWF (P = 0.048), and hsCRP (P = 0.038). After 6 months, both groups showed a significant and identical decrease in the systolic and diastolic blood pressure compared with the baseline (P < 0.002). However, there were no significant differences in the endothelial markers between each group. On the other hand, there was some deterioration in the triglyceride (P = 0.009) and HbA1c (P = 0.017) levels in the atenolol treatment groups.
CONCLUSIONS
There were no significant differences in the endothelial function markers observed between the cilazapril and atenolol groups. However, cilazapril had an identical effect on the blood pressure reduction compared with atenolol but had fewer adverse effects on the glucose and lipid metabolism.
MeSH Terms
-
Adiponectin
Amlodipine
Atenolol
Biomarkers
Blood Pressure
Cholesterol, LDL
Cilazapril*
Diabetes Mellitus, Type 2
E-Selectin
Endothelial Cells
Endothelium, Vascular
Fibrinogen
Follow-Up Studies
Glucose
Hand
Hospitals, University
Humans
Hydrochlorothiazide
Hypertension*
Korea
Lipid Metabolism
Nitric Oxide
Oxidative Stress
Peptidyl-Dipeptidase A
Thrombophilia
Triglycerides
Adiponectin
Amlodipine
Atenolol
Cholesterol, LDL
Cilazapril
E-Selectin
Fibrinogen
Glucose
Hydrochlorothiazide
Nitric Oxide
Peptidyl-Dipeptidase A
Figure
Reference
-
1. Stamler J, Vaccaro O, Neaton JD, Wentworth D. Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care. 1993. 16:434–444.2. de Vegt F, Dekker JM, Ruhe HG, Stehouwer CD, Nijpels G, Bouter LM, Heine RJ. Hyperglycaemia is associated with all-cause and cardiovascular mortality in the Hoorn population: the Hoorn Study. Diabetologia. 1999. 42:926–931.3. Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998. 339:229–234.4. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001. 285:2486–2497.5. de Jager J, Dekker JM, Kooy A, Kostense PJ, Nijpels G, Heine RJ, Bouter LM, Stehouwer CD. Endothelial dysfunction and low-grade inflammation explain much of the excess cardiovascular mortality in individuals with type 2 diabetes: the Hoorn Study. Arterioscler Thromb Vasc Biol. 2006. 26:1086–1093.6. Chaudhuri A. Vascular reactivity in diabetes mellitus. Curr Diab Rep. 2002. 2:305–310.7. Ferri C, Desideri G, Baldoncini R, Bellini C, De Angelis C, Mazzocchi C, Santucci A. Early activation of vascular endothelium in nonobese, nondiabetic essential hypertensive patients with multiple metabolic abnormalities. Diabetes. 1998. 47:660–667.8. Saydah SH, Loria CM, Eberhardt MS, Brancati FL. Subclinical states of glucose intolerance and risk of death in the U.S. Diabetes Care. 2001. 24:447–453.9. Stehouwer CD, Gall MA, Twisk JW, Knudsen E, Emeis JJ, Parving HH. Increased urinary albumin excretion, endothelial dysfunction, and chronic low-grade inflammation in type 2 diabetes: progressive, interrelated, and independently associated with risk of death. Diabetes. 2002. 51:1157–1165.10. Kinlay S, Libby P, Ganz P. Endothelial function and coronary artery disease. Curr Opin Lipidol. 2001. 12:383–389.11. De Caterina R. Endothelial dysfunctions: common denominators in vascular disease. Curr Opin Clin Nutr Metab Care. 2000. 3:453–467.12. Schachinger V, Zeiher AM. Prognostic implications of endothelial dysfunction: does it mean anything? Coron Artery Dis. 2001. 12:435–443.13. Schmidt AM, Hori O, Chen JX, Li JF, Crandall J, Zhang J, Cao R, Yan SD, Brett J, Stern D. Advanced glycation endproducts interacting with their endothelial receptor induce expression of vascular cell adhesion molecule-1 (VCAM-1) in cultured human endothelial cells and in mice. A potential mechanism for the accelerated vasculopathy of diabetes. J Clin Invest. 1995. 96:1395–1403.14. Conlan MG, Folsom AR, Finch A, Davis CE, Sorlie P, Wu KK. Correlation of plasma protein C levels with cardiovascular risk factors in middle-aged adults: the Atherosclerosis Risk in Communities (ARIC) Study. Thromb Haemost. 1993. 70:762–767.15. Park L, Raman KG, Lee KJ, Lu Y, Ferran LJ Jr, Chow WS, Stern D, Schmidt AM. Suppression of accelerated diabetic atherosclerosis by the soluble receptor for advanced glycation endproducts. Nat Med. 1998. 4:1025–1031.16. Irani K. Oxidant signaling in vascular cell growth, death, and survival: a review of the roles of reactive oxygen species in smooth muscle and endothelial cell mitogenic and apoptotic signaling. Circ Res. 2000. 87:179–183.17. Lewis TV, Dart AM, Chin-Dusting JP. Endothelium-dependent relaxation by acetylcholine is impaired in hypertriglyceridemic humans with normal levels of plasma LDL cholesterol. J Am Coll Cardiol. 1999. 33:805–812.18. Shimokawa H. Primary endothelial dysfunction: atherosclerosis. J Mol Cell Cardiol. 1999. 31:23–37.19. Watts GF, O'Brien SF, Silvester W, Millar JA. Impaired endothelium-dependent and independent dilatation of forearm resistance arteries in men with diet-treated non-insulin-dependent diabetes: role of dyslipidaemia. Clin Sci (Lond). 1996. 91:567–573.20. Steinberg HO, Tarshoby M, Monestel R, Hook G, Cronin J, Johnson A, Bayazeed B, Baron AD. Elevated circulating free fatty acid levels impair endothelium-dependent vasodilation. J Clin Invest. 1997. 100:1230–1239.21. Goto K, Fujii K, Onaka U, Abe I, Fujishima M. Renin-angiotensin system blockade improves endothelial dysfunction inhypertension. Hypertension. 2000. 36:575–580.22. Cheetham C, O'Driscoll G, Stanton K, Taylor R, Green D. Losartan, an angiotensin type I receptor antagonist, improves conduit vessel endothelial function in Type II diabetes. Clin Sci (Lond). 2001. 100:13–17.23. d'Uscio LV, Quaschning T, Burnett JC Jr, Luscher TF. Vasopeptidase Inhibition Prevents Endothelial Dysfunction of Resistance Arteries in Salt-Sensitive Hypertension in Comparison With Single ACE Inhibition. Hypertension. 2001. 37:28–33.24. Wassmann S, Hilgers S, Laufs U, Bohm M, Nickenig G. Angiotensin II type 1 receptor antagonism improves hypercholesterolemia-associated endothelial dysfunction. Arterioscler Thromb Vasc Biol. 2002. 22:1208–1212.25. Gasic S, Wagner OF, Fasching P, Ludwig C, Veitl M, Kapiotis S, Jilma B. Fosinopril decreases levels of soluble vascular cell adhesion molecule-1 in borderline hypertensive type II diabetic patients with microalbuminuria. Am J Hypertens. 1999. 12:217–222.26. Gibbs CR, Blann AD, Watson RD, Lip GY. Abnormalities of hemorheological, endothelial, and platelet function in patients with chronic heart failure in sinus rhythm: effects of angiotensin-converting enzyme inhibitor and beta-blocker therapy. Circulation. 2001. 103:1746–1751.27. Brown NJ, Kumar S, Painter CA, Vaughan DE. ACE inhibition versus angiotensin type 1 receptor antagonism: differential effects on PAI-1 over time. Hypertension. 2002. 40:859–865.28. Lithell HO. Effect of antihypertensive drugs on insulin, glucose, and lipid metabolism. Diabetes Care. 1991. 14:203–209.29. Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. N Engl J Med. 1993. 329:1456–1462.30. Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med. 2000. 342:145–153.31. Kasper DL, Harrison TR, Beal MF, Bosl GJ, Crystal RG, Motzer RJ. Harrison's principles of internal medicine. 2005. 16th ed. New York: McGraw-Hill, Medical Pub. Division.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Study Design and Protocol for a Randomized Controlled Trial of Enavogliflozin to Evaluate Cardiorenal Outcomes in Type 2 Diabetes (ENVELOP)
- Self-Monitoring of Blood Pressure and Feed-back Using APP in TReatment of UnconTrolled Hypertension (SMART-BP): A Randomized Clinical Trial
- Effects of Dapagliflozin on Endothelial Function, Renal Injury Markers, and Glycemic Control in Drug-Naïve Patients with Type 2 Diabetes Mellitus
- The Dipeptidyl Peptidase-4 Inhibitor Sitagliptin Improves Vascular Endothelial Function in Type 2 Diabetes
- Blood Pressure Variability and Vascular Dysfunction in Essential Hypertension