J Korean Diabetes Assoc.
2006 Jan;30(1):73-81.
Glycemic Control and Health Behaviors through Diabetes Mellitus Education in a Clinic
- Affiliations
-
- 1Chang's Clinic.
- 2Department of Preventive Medicine, College of Medicine, Dongguk University.
Abstract
-
BACKGROUND: This study was carried out to examine the changes in the health behaviors and glycemic control before and after administering a Diabetes Mellitus (DM) education program in a clinic.
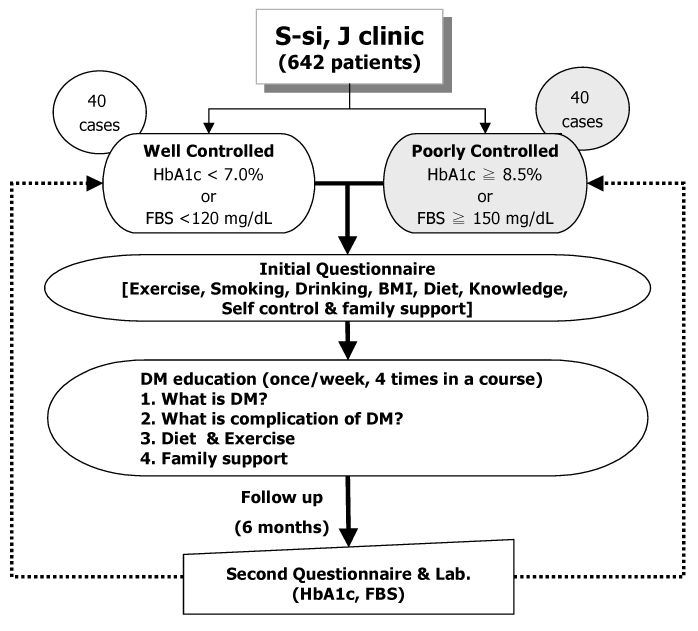
METHODS
The author conducted a questionnaire and analyzed the blood chemistry with the fasting plasma blood sugar (FBS) and hemoglobin A1c (HbA1c) level of 80 patients in a clinic for 6 months from February to July 2004. The study group was divided into a poorly controlled (PC) group and well-controlled (WC) group according to the FBS or HbA1c level. The author then educated the subjects about general knowledges for DM over a 6-month period. The changes in the results before and after the DM education were measured as the changes in the health behaviors along with the changes in the FBS, and HbA1c levels.
RESULTS
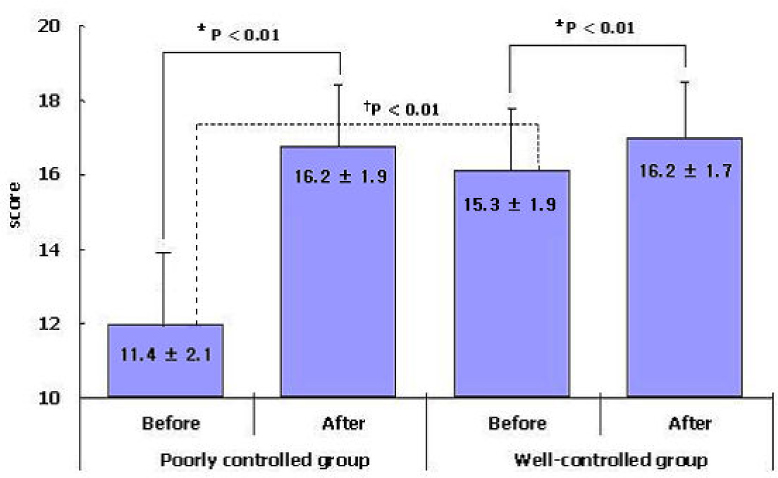
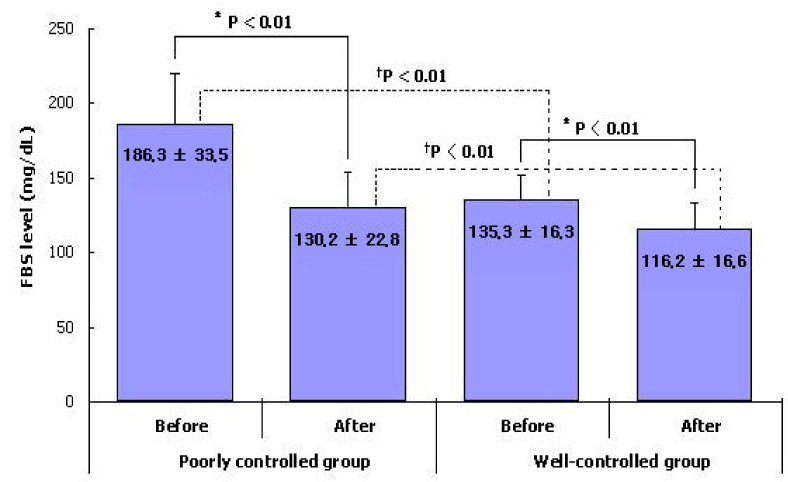
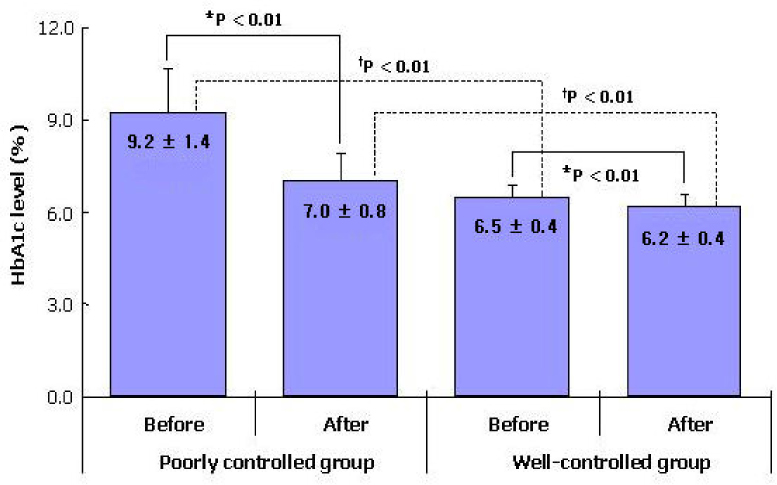
The study subjects contained 20 males and 20 females in each groups, and the major age group was the fifth decade (22 cases, 27.5%). The mean values for the total health behavior scores after the DM education program in the PC and WC group were 16.2 +/- 1.9, and 16.2 +/- 1.7 respectively, and were significantly higher than that before the education program (11.4 +/- 2.1, 15.3 +/- 1.9, P < 0.05). The mean FBS levels after the DM education program in the PC and WC groups were 130.2 +/- 22.8 mg/dL, and 116.2 +/- 16.6 mg/dL respectively, and was significantly lower than that before the education program (186.3 +/- 33.5 mg/dL, 135.3 +/- 16.3 mg/dL, P < 0.05). The mean HbA1c levels after the DM education program in the PC and WC groups were 7.0 +/- 0.8%, and 6.2 +/- 0.4% respectively, which were significantly lower than that before the education program (9.2 +/- 1.4%, 6.5 +/- 0.4%, P < 0.05).
CONCLUSION
This study suggests that a DM education program in a clinic is effective in improving the health behaviors and laboratory findings in DM patients.
Keyword
MeSH Terms
Figure
Reference
-
4. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993. 329:977–986.5. Nicolucci A, Cavaliere D, Scorpiglione N, Carinci F, Capani F, Tognoni G, Benedetti MM. SID-AMD Italian Study Group for the Implementation of the St. Vincent Declaration. A comprehensive assessment of the avoidability of long-term complications of diabetes. A case-control study. Diabetes Care. 1996. 19:927–933.6. UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with diabetes (UKPDS 34). Lancet. 1998. 352:854–865.7. Graber AL, Christman BG, Alogna MT, Davidson JK. Evaluation of diabetes patient-education programs. Diabetes. 1977. 26:61–64.13. Glasgow RE. Outcomes of and for diabetes education research. Diabetes Educ. 1999. 25:74–88.14. The 1999 Scope of Practice for Diabetes Educators and the Standards of Practice for Diabetes Educators. AADE. Cited 2004 Dec 5. Available from URL: http://www.aadenet.org/AboutAADE/99ScopeStandards.html.15. Glasgow RE, Osteen VL. Evaluating diabetes education. Are we measuring the most important outcomes? Diabetes Care. 1992. 15:1423–1432.16. Mensing C, Boucher J, Cypress M, Weinger K, Mulcahy K, Barta P, Hosey G, Kopher W, Lasichak A, Lamb B, Mangan M, Norman J, Tanja J, Yauk L, Wisdom K, Adams C. National standards for diabetes self-management education. Task Force to Review and Revise the National Standards for Diabetes Self-Management Education Programs. Diabetes Care. 2000. 23:682–689.17. Laitinen JH, Ahola IE, Sarkkinen ES, Winberg RL, Harmaakorpi-Iivonen PA, Uusitupa MI. Impact of intensified dietary therapy on energy and nutrient intakes and fatty acid composition of serum lipids in patients with recently diagnosed non-insulin-dependent diabetes mellitus. J Am Diet Assoc. 1993. 93:276–283.19. Goodall TA, Halford WK. Self-management of diabetes mellitus: a critical review. Health Psychol. 1991. 10:1–8.20. World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation on obesity. 1997. Geneva.21. NIH-NHLBI. Clinical Guidelines on the Identification, Evaluation and Treatment of Overweight and Obesity in Adults. The evidence report. 1998. Bethesda:22. International Obesity Task Force. International Association for the Study of Obesity. The Asia-Pacific perspective: redefining obesity and its treatment. WHO Western Pacific Region. 2000.24. ADA. Standards of Medical Care for Patients With Diabetes Mellitus. Diabetes Care. 2002. 25:S33–S49.25. ADA. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2003. 26:5–20.27. Matthews DR, Cull CA, Stratton IM, Holman RR, Turner RC. UK Prospective Diabetes Study (UKPDS) Group. UKPDS 26: Sulphonylurea failure in non-insulin-dependent diabetic patients over six years. Diabet Med. 1998. 15:297–303.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of Diabetes Educators and Effectiveness of Diabetes Education
- Factors Influencing Glycemic Control by gender in Workers with Diabetes Mellitus
- The Effect of a Community-Based Selp-Help Management Program for Patients with Diabetes Mellitus
- Associations between grip strength and glycemic control in type 2 diabetes mellitus: an analysis of data from the 2014-2019 Korea National Health and Nutrition Examination Survey
- Hypoglycemia Care