J Dent Anesth Pain Med.
2016 Jun;16(2):117-122. 10.17245/jdapm.2016.16.2.117.
Comparative study of analgesia with bupivacaine 0.25% versus 0.5% for third molar removal under general anesthesia
- Affiliations
-
- 1Oral Surgery, Hcf dental center, Sydney, Australia. dan.dhanrajani@gmail.com
- 2VMO, Concord Repatriation General Hospital, Sydney, Australia.
- KMID: 2328854
- DOI: http://doi.org/10.17245/jdapm.2016.16.2.117
Abstract
- BACKGROUND
The aim of this study was to compare the effectiveness and duration of action of two concentrations of bupivacaine with adrenaline for postoperative pain in patients undergoing surgical removal of four third molars under general anesthesia.
METHODS
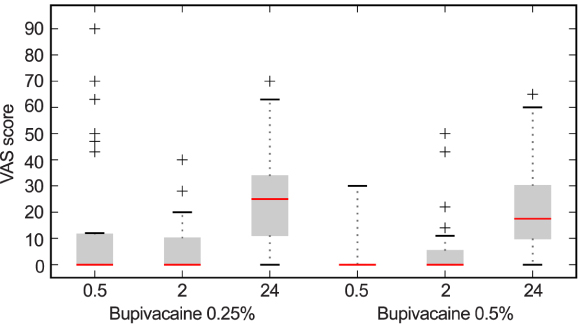
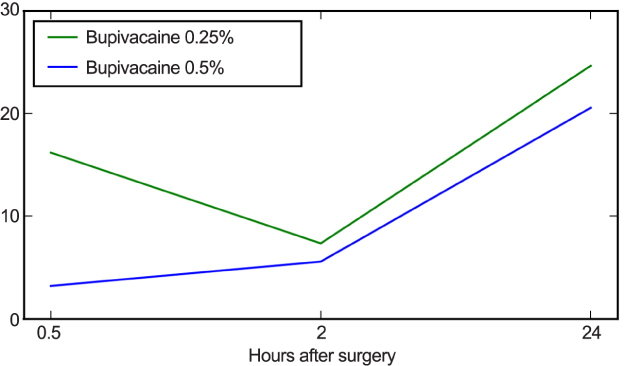
Sixty patients undergoing surgical removal of four wisdom teeth received bupivacaine 0.5% (n = 30) or 0.25% (n = 30). The severity of pain in the immediate recovery period and at 2 and 24 h after surgery was recorded using the visual analogue scale. Differences were assessed by box and whisper plot and the Student's t-test.
RESULTS
The analgesic effects of the 0.25% and 0.5% doses were significantly different (P = 0.022) at 30 min after surgery but not after 2 and 24 h. The difference of mean of 0.25% and 0.5% was much higher after 0.5 h but less after 2 and 24 h.
CONCLUSIONS
Bupivacaine 0.5% was statistically better for pain control during the immediate postoperative period, but there was no significant difference in pain control between the two dose strengths at 2 and 24 h after surgery.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
An in vivo study comparing efficacy of 0.25% and 0.5% bupivacaine in infraorbital nerve block for postoperative analgesia
Aditi Saha, Sonal Shah, Pushkar Waknis, Sharvika Aher, Prathamesh Bhujbal, Vibha Vaswani
J Dent Anesth Pain Med. 2019;19(4):209-215. doi: 10.17245/jdapm.2019.19.4.209.
Reference
-
1. Sancho-Puchades M, Vilchez-perez M, Valmaseda-Castellon E, Paredes-Garcia J, Berini-Aytes L, Gay-Escoda C. Bupivacaine 0.5% versus 4% for the removal of lower third molars. A crossover randomized controlled trial. Med Oral Patol Oral Cir Bucal. 2012; 17:e462–e468.
Article2. Sisk AL. Long-acting local anaesthetics in dentistry. Anaesth Prog. 1992; 39:53–60.
Article3. Valpato MC, Ranali J, Groppo FC. Anaesthetic efficacy of bupivacaine solutions in inferior alveolar nerve block. Anaesth Prog. 2005; 52:132–135.
Article4. Moore PA. Bupivacaine: A long-standing local anaesthetic for dentistry. Oral Surg Oral Med Oral Pathol. 1984; 58:369–374.
Article5. Bouloux GF, Punnia-Moorthy A. Bupivacaine versus lidocaine for third molar surgery: adouble-blind, randomized, crossover study. J Oral Maxillofac Surg. 1999; 57:510–514.
Article6. Branco FP, Ranali J, Ambrosano GM, Volpato MC. A double-blind comparison of 0.5% bupivacaine with 1:200,000 epinepherine and 0.5% levobupivacaine with 1:200,000 epinepherine for the inferior alveolar nerve block. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:442–447.
Article7. Gregorio LV, Giglio FP, Sakai VT, Modena KC, Colombini BL, Calvo AM, et al. Comparison of the clinical anaesthtic efficacy of 4% articaine and 0.5% bupivacaine (both with 1:200,000 epinepherine) for lower third molar removal. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:19–28.
Article8. Nayyar MS, Yates C. Bupivacaine as pre-emptive analgesia in third molar surgery: randomized controlled trial. Br J Oral Maxillofac Surg. 2006; 44:501–503.
Article9. Shyamala M, Ramesh C, Yuvraj V, Suresh V, Sathya-Narayanan R, Balaji TS, et al. A comparative study between bupivacaine with adrenaline and carbonated bupivacaine with adrenaline for surgical removal of impacted mandibular third molar. J Maxillofac Oral Surg. 2016; 15:99–105.
Article10. Maeda N, Shimomura I, Kishida K, Nishizawa H, Matsuda M, Nagaretani H, et al. Diet-induced insulin resistance in mice lacking adiponectin/ACRP30. Nat Med. 2002; 8:731–737.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the effects of articaine and bupivacaine in impacted mandibular third molar tooth surgery: a randomized, controlled trial
- The Effect of Intraarticular Morphine and Clonidine on Postoperative Analgesia after Knee Surgery
- The Comparative Investigation of the Spread of Epidural Anesthesia
- Effectiveness of spinal anesthesia after epidural labor analgesia versus spinal anesthesia only for intrapartum cesarean section
- The Effects of Clonidine in Pediatric Caudal Anesthesia