Infect Chemother.
2016 Jun;48(2):99-107. 10.3947/ic.2016.48.2.99.
Outbreaks of Middle East Respiratory Syndrome in Two Hospitals Initiated by a Single Patient in Daejeon, South Korea
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Division of Infectious Diseases, Department of Internal Medicine, Chungnam National University School of Medicine, Daejeon, Korea. alice@cnuh.co.kr
- 3Division of infectious disease, Department of internal medicine, Hallym Sacred Heart Hospital, Anayang, Korea.
- 4Department of Neurology, Dae-Chung Hospital, Daejeon, Korea.
- 5Department of Microbiology and Immunology, Department of Biomedical Science, Seoul National University College of Medicine and Bundang Hospital, Seoul, Korea.
- 6Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, Chungbuk National University, Cheongju, Korea.
- 7Division of Infectious Diseases, Department of Internal Medicine, Eulji University hospital, Daejeon, Korea.
- 8Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, Hallym University, Seoul, Korea.
- KMID: 2327977
- DOI: http://doi.org/10.3947/ic.2016.48.2.99
Abstract
- BACKGROUND
A Middle East Respiratory Syndrome coronavirus (MERS-CoV) outbreak in South Korea in 2015 started by a single imported case and was amplified by intra- and inter-hospital transmission. We describe two hospital outbreaks of MERS-CoV infection in Daejeon caused by a single patient who was infected by the first Korean case of MERS.
MATERIALS AND METHODS
Demographic and clinical information involving MERS cases in the Daejeon cluster were retrospectively collected and potential contacts and exposures were assessed. The incubation periods and serial intervals were estimated. Viral RNAs were extracted from respiratory tract samples obtained from the index case, four secondary cases and one tertiary case from each hospital. The partial S2 domain of the MERS-CoV spike was sequenced.
RESULTS
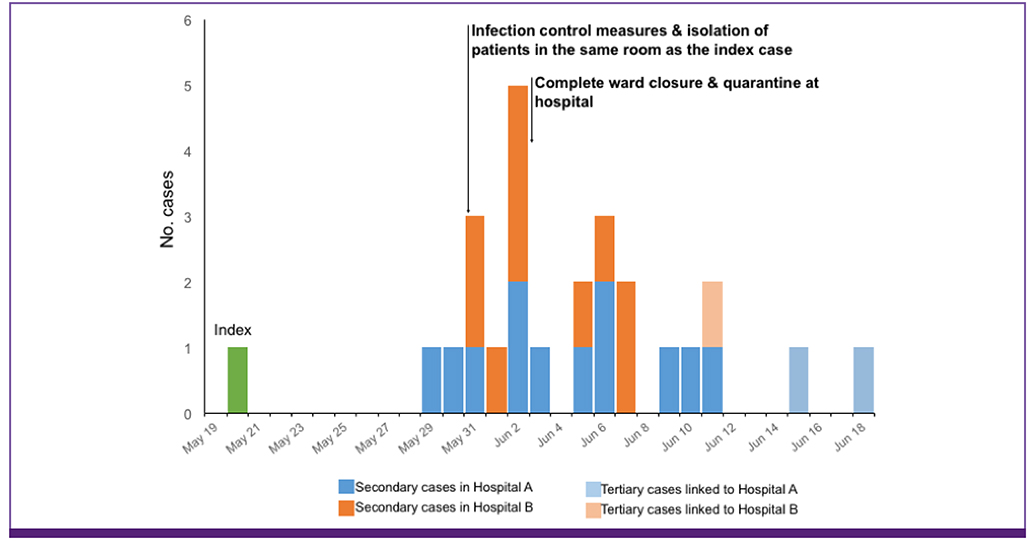
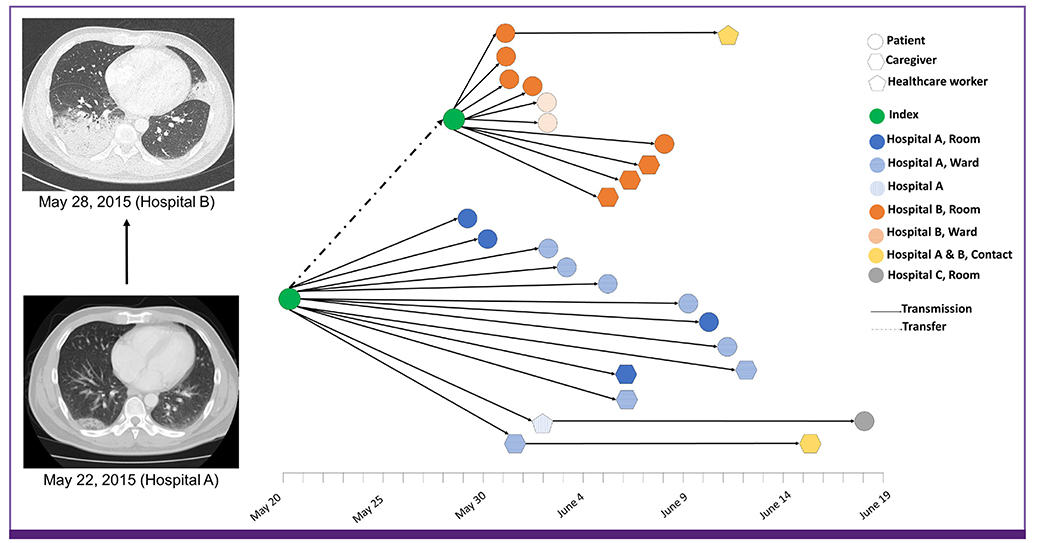
In Daejeon, a MERS patient (the index case) was hospitalized at Hospital A in the first week of illness and was transferred to Hospital B because of pneumonia progression in the second week of illness, where he received a bronchoscopic examination and nebulizer therapy. A total of 23 secondary cases (10 in Hospital A and 13 in Hospital B) were detected among patients and caregivers who stayed on the same ward with the index case. There were no secondary cases among healthcare workers. Among close hospital contacts, the secondary attack rate was 15.8% (12/76) in Hospital A and 14.3% (10/70) in Hospital B. However, considering the exposure duration, the incidence rate was higher in Hospital B (7.7/100 exposure-days) than Hospital A (3.4/100 exposure-days). In Hospital B, the median incubation period was shorter (4.6 days vs. 10.8 days), the median time to pneumonia development was faster (3 days vs. 6 days) and mortality was higher (70% vs. 30.8%) than in Hospital A. MERS-CoV isolates from 11 cases formed a single monophyletic clade, with the closest similarity to strains from Riyadh.
CONCLUSION
Exposure to the MERS case in the late stage (2nd week) of diseases appeared to increase the risk of transmission and was associated with shorter incubation periods and rapid disease progression among those infected. Early detection and isolation of cases is critical in preventing the spread of MERS in the hospital and decreasing the disease severity among those infected.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The Korean Middle East Respiratory Syndrome Coronavirus Outbreak and Our Responsibility to the Global Scientific Community
Myoung-don Oh
Infect Chemother. 2016;48(2):145-146. doi: 10.3947/ic.2016.48.2.145.
Reference
-
1. Oboho IK, Tomczyk SM, Al-Asmari AM, Banjar AA, Al-Mugti H, Aloraini MS, Alkhaldi KZ, Almohammadi EL, Alraddadi BM, Gerber SI, Swerdlow DL, Watson JT, Madani TA. 2014 MERS-Cov outbreak in Jeddah-a link to health care facilities. N Engl J Med. 2015; 372:846–854.
Article2. Assiri A, McGeer A, Perl TM, Price CS, Al Rabeeah AA, Cummings DA, Alabdullatif ZN, Assad M, Almulhim A, Makhdoom H, Madani H, Alhakeem R, Al-Tawfiq JA, Cotten M, Watson SJ, Kellam P, Zumla AI, Memish ZA. KSA MERS-CoV Investigation Team. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med. 2013; 369:407–416.
Article3. Park YS, Lee C, Kim KM, Kim SW, Lee KJ, Ahn J, Ki M. The first case of the 2015 Korean Middle East Respiratory Syndrome outbreak. Epidemiol Health. 2015; 37:e2015049.
Article4. Choi JY. An outbreak of middle east respiratory syndrome coronavirus infection in South Korea, 2015. Yonsei Med J. 2015; 56:1174–1176.
Article5. Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiol Health. 2015; 37:e2015033.
Article6. Korea Centers for Disease Control and Prevention (KCDC). Middle East Respiratory Syndrome coronavirus outbreak in the Republic of Korea, 2015. Osong Public Health Res Perspect. 2015; 6:269–278.
Article7. Ministry of Welfare and Health. MERS statistics. Accessed 25 February 2016. Available at: http://www.mers.go.kr/mers/html/jsp/Menu_C/list_C4.jsp?menuIds=&fid=5767&q_type=&q_value=&cid=65327&pageNum=1.
Article8. Al-Abdallat MM, Payne DC, Alqasrawi S, Rha B, Tohme RA, Abedi GR, Al Nsour M, Iblan I, Jarour N, Farag NH, Haddadin A, Al-Sanouri T, Tamin A, Harcourt JL, Kuhar DT, Swerdlow DL, Erdman DD, Pallansch MA, Haynes LM, Gerber SI. Jordan MERS-CoV Investigation Team. Hospital-associated outbreak of Middle East respiratory syndrome coronavirus: a serologic, epidemiologic, and clinical description. Clin Infect Dis. 2014; 59:1225–1233.
Article9. Ministry of Health and Welfare. Press relseases. Accessed 9 September, 2015. Available at: http://www.mers.go.kr/mers/html/jsp/Menu_C/list_C1.jsp.
Article10. World Health Organizaion (WHO). Laboratory testing for middle east respiratory syndrome coronavirus. Accessed June 25, 2015. Available at: http://www.who.int/csr/disease/coronavirus_infections/WHO_interim_recommendations_lab_detection_MERSCoV_092014.pdf.
Article11. Korean Centers for Disease Control and Prevention (KCDC). Guideline for management of MERS (in Korean). Accessed 3 September, 2015. Available at: http://cdc.go.kr/CDC/info/CdcKrHealth0295.jsp?menuIds=HOME001-MNU1132-MNU1013-MNU1509-MNU1915&fid=5747&q_type=&q_value=&cid=63292&pageNum=.
Article12. Kim JY, Song JY, Yoon YK, Choi SH, Song YG, Kim SR, Son HJ, Jeong SY, Choi JH, Kim KM, Yoon HJ, Choi JY, Kim TH, Choi YH, Kim HB, Yoon JH, Lee J, Eom JS, Lee SO, Oh WS, Choi JH, Yoo JH, Kim WJ, Cheong HJ. Middle East respiratory syndrome infection control and prevention guideline for healthcare facilities. Infect Chemother. 2015; 47:278–302.
Article13. Smits SL, Raj VS, Pas SD, Reusken CB, Mohran K, Farag EA, Al-Romaihi HE, AlHajri MM, Haagmans BL, Koopmans MP. Reliable typing of MERS-CoV variants with a small genome fragment. J Clin Virol. 2015; 64:83–87.
Article14. Cotten M, Watson SJ, Zumla AI, Makhdoom HQ, Palser AL, Ong SH, Al Rabeeah AA, Alhakeem RF, Assiri A, Al-Tawfiq JA, Albarrak A, Barry M, Shibl A, Alrabiah FA, Hajjar S, Balkhy HH, Flemban H, Rambaut A, Kellam P, Memish ZA. Spread, circulation, and evolution of the Middle East respiratory syndrome coronavirus. MBio. 2014; 5:pii:e0062-14.
Article15. Lu R, Wang Y, Wang W, Nie K, Zhao Y, Su J, Deng Y, Zhou W, Li Y, Wang H, Wang W, Ke C, Ma X, Wu G, Tan W. Complete genome sequence of Middle East Respiratory Syndrome coronavirus (MERS-CoV) from the first imported MERS-CoV case in china. Genome Announc. 2015; 3:pii:e00818-15.
Article16. Tamura K, Stecher G, Peterson D, Filipski A, Kumar S. MEGA6: Molecular evolutionary genetics analysis version 6.0. Mol Biol Evol. 2013; 30:2725–2729.
Article17. Gouy M, Guindon S, Gascuel O. Seaview version 4: A multi-platform graphical user interface for sequence alignment and phylogenetic tree building. Mol Biol Evol. 2010; 27:221–224.
Article18. Reich NG, Lessler J, Cummings DAT, Brookmeyer R. Estimating incubation period distributions with coarse data. Stat Med. 2009; 28:2769–2784.
Article19. Kim YJ, Cho YJ, Kim DW, Yang JS, Kim H, Park S, Han YW, Yun MR, Lee HS, Kim AR, Heo DR, Kim JA, Kim SJ, Jung HD, Kim N, Yoon SH, Nam JG, Kang HJ, Cheong HM, Lee JS, Chun J, Kim SS. Complete genome sequence of Middle East Respiratory Syndrome coronavirus kor/knih/002_05_2015, isolated in South Korea. Genome Announc. 2015; 3:pii:e00787-15.
Article20. Oh MD, Choe PG, Oh HS, Park WB, Lee SM, Park J, Lee SK, Song JS, Kim NJ. Middle East Respiratory Syndrome coronavirus superspreading event involving 81 persons, Korea 2015. J Korean Med Sci. 2015; 30:1701–1705.
Article21. Poissy J, Goffard A, Parmentier-Decrucq E, Favory R, Kauv M, Kipnis E, Mathieu D, van der Werf S, Guery B. MERS-CoV Biology Group. Kinetics and pattern of viral excretion in biological specimens of two MERS-CoV cases. J Clin Virol. 2014; 61:275–278.
Article22. Shen Z, Ning F, Zhou W, He X, Lin C, Chin DP, Zhu Z, Schuchat A. Superspreading sars events, Beijing, 2003. Emerg Infect Dis. 2004; 10:256–260.
Article23. Seto WH. Airborne transmission and precautions: facts and myths. J Hosp Infect. 2015; 89:225–228.
Article24. Fisman DN, Leung GM, Lipsitch M. Nuanced risk assessment for emerging infectious diseases. Lancet. 2014; 383:189–190.
Article25. Kucharski AJ, Althaus CL. The role of superspreading in Middle East respiratory syndrome coronavirus (MERS-CoV) transmission. Euro Surveill. 2015; 20:14–18.
Article26. Fagbo SF, Skakni L, Chu DK, Garbati MA, Joseph M, Peiris M, Hakawi AM. Molecular epidemiology of hospital outbreak of Middle East respiratory syndrome, Riyadh, Saudi arabia, 2014. Emerg Infect Dis. 2015; 21:1981–1988.27. Drosten C, Muth D, Corman VM, Hussain R, Al Masri M, HajOmar W, Landt O, Assiri A, Eckerle I, Al Shangiti A, Al-Tawfiq JA, Albarrak A, Zumla A, Rambaut A, Memish ZA. An observational, laboratory-based study of outbreaks of Middle East respiratory syndrome coronavirus in Jeddah and Riyadh, kingdom of Saudi arabia, 2014. Clin Infect Dis. 2015; 60:369–377.28. World Health Organization (WHO). Middle East Respiratory Syndrome coronavirus (MERS-CoV): summary of current siation, literature update and risk assessment. WHO/MERS/RA/151 2015. Accessed 25 September 2015. Available at: http://www.who.int/csr/disease/coronavirus_infections/risk-assessment-7july2015/en/.29. World Health Organization (WHO). Disease outbreak news. Middle East Respiratory Syndrome coronavirus (MERS-CoV)-Saudi Arabia. Accessed 18 September 2015. Available at: http://www.who.int/csr/don/17-september-2015-mers-saudi-arabia/en/.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Fatal Case of Middle East Respiratory Syndrome Corona Virus Infection in South Korea: Chest Radiography and CT Findings
- An Unexpected Outbreak of Middle East Respiratory Syndrome Coronavirus Infection in the Republic of Korea, 2015
- Considerations Left behind Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Outbreaks in Republic of Korea
- Middle East respiratory syndrome: what we learned from the 2015 outbreak in the Republic of Korea
- Ethical Perspectives on the Middle East Respiratory Syndrome Coronavirus Epidemic in Korea