Ann Surg Treat Res.
2016 Jul;91(1):8-16. 10.4174/astr.2016.91.1.8.
Characteristics of patients operated for primary hyperparathyroidism at university hospitals in Türkiye: differences among Türkiye's geographical regions
- Affiliations
-
- 1Department of Surgery, Uludag University Faculty of Medicine, Bursa, Türkiye. tkirdak@uludag.edu.tr
- 2Department of Surgery, Kocaeli University Faculty of Medicine, Kocaeli, Türkiye.
- 3Department of Biostatistics, Uludag University Faculty of Medicine, Bursa, Türkiye.
- KMID: 2327411
- DOI: http://doi.org/10.4174/astr.2016.91.1.8
Abstract
- PURPOSE
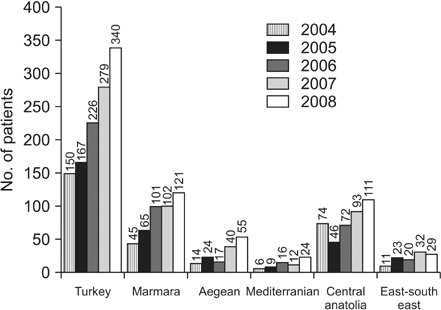
The aim of this study was to define the clinical and laboratory characteristics of patients operated on for primary hyperpatathyroidism (PHPT) at university hospitals in Türkiye, and to investigate the differences in the clinical presentations of the disease between different geographical regions.
METHODS
Patients operated on for PHPT in the university hospitals of Türkiye were included in the study. The demographic, clinical, and laboratory findings and the operational data of the patients were investigated according to the whole country and to different geographical regions. Comparisons were performed according to whole country and regions.
RESULTS
A total of 1,162 cases were included in the study from different regions and 20 university hospitals. The mean age of patients was 52.4 ± 0.38 (mean ± standard error) in the general population of Türkiye. The rates of hypertension, urolithiasis, bone disease and 25-hydroxyvitamin D insufficiency were 35%, 18.6%, 67.6%, and 63%, respectively. The median parathormone (PTH), serum total calcium (Ca+2) and phosphorus value were 220 pg/mL (range, 70-2,500 pg/mL), 11.2 mg/dL (range, 9.5-11.2 mg/dL), and 2.4 mg/dL (range, 1-4.7 mg/dL), respectively. The median size of the adenomas resected was 16 mm (range, 4-70 mm). Significant differences were observed in the clinical and laboratory findings of the patients operated on due to PHPT between different geographical regions of Türkiye (P < 0.05).
CONCLUSION
The clinical and laboratory characteristics of the patients with PHPT in different geographical regions of Türkiye differ. Furthermore, the general findings of the cases in Türkiye give us a hint that the severity of the disease here is somewhere between Eastern and Western countries.
MeSH Terms
Figure
Reference
-
1. Bilezikian JP, Meng X, Shi Y, Silverberg SJ. Primary hyperparathyroidism in women: a tale of two cities--New York and Beijing. Int J Fertil Womens Med. 2000; 45:158–165.2. Yeh MW, Ituarte PH, Zhou HC, Nishimoto S, Liu IL, Harari A, et al. Incidence and prevalence of primary hyperparathyroidism in a racially mixed population. J Clin Endocrinol Metab. 2013; 98:1122–1129.3. Kirdak T, Duh QY, Kebebew E, Clark OH. Do patients undergoing parathyroidectomy for primary hyperparathyroidism in San Francisco, CA, and Bursa, Turkey, differ? Am J Surg. 2009; 198:188–192.4. De Lucia F, Minisola S, Romagnoli E, Pepe J, Cipriani C, Scillitani A, et al. Effect of gender and geographic location on the expression of primary hyperparathyroidism. J Endocrinol Invest. 2013; 36:123–126.5. Nordenstrom E, Sitges-Serra A, Sancho JJ, Thier M, Almquist M. Vitamin d status in patients operated for primary hyperparathyroidism: comparison of patients from southern and northern europe. Int J Endocrinol. 2013; 2013:164939.6. Griebeler ML, Kearns AE, Ryu E, Hathcock MA, Melton LJ 3rd, Wermers RA. Secular trends in the incidence of primary hyperparathyroidism over five decades (1965-2010). Bone. 2015; 73:1–7.7. Rao DS, Honasoge M, Divine GW, Phillips ER, Lee MW, Ansari MR, et al. Effect of vitamin D nutrition on parathyroid adenoma weight: pathogenetic and clinical implications. J Clin Endocrinol Metab. 2000; 85:1054–1058.8. Karakas E, Schneider R, Rothmund M, Bartsch DK, Schlosser K. Initial surgery for benign primary hyperparathyroidism: an analysis of 1,300 patients in a teaching hospital. World J Surg. 2014; 38:2011–2018.9. Tassone F, Gianotti L, Baffoni C, Visconti G, Pellegrino M, Cassibba S, et al. Vitamin D status in primary hyperparathyroidism: a Southern European perspective. Clin Endocrinol (Oxf). 2013; 79:784–790.10. Moosgaard B, Vestergaard P, Heickendorff L, Melsen F, Christiansen P, Mosekilde L. Vitamin D status, seasonal variations, parathyroid adenoma weight and bone mineral density in primary hyperparathyroidism. Clin Endocrinol (Oxf). 2005; 63:506–513.11. Mishra SK, Agarwal G, Kar DK, Gupta SK, Mithal A, Rastad J. Unique clinical characteristics of primary hyperparathyroidism in India. Br J Surg. 2001; 88:708–714.12. Zhao L, Liu JM, He XY, Zhao HY, Sun LH, Tao B, et al. The changing clinical patterns of primary hyperparathyroidism in Chinese patients: data from 2000 to 2010 in a single clinical center. J Clin Endocrinol Metab. 2013; 98:721–728.13. Lo CY, Chan WF, Kung AW, Lam KY, Tam SC, Lam KS. Surgical treatment for primary hyperparathyroidism in Hong Kong: changes in clinical pattern over 3 decades. Arch Surg. 2004; 139:77–82.14. Heath H 3rd, Hodgson SF, Kennedy MA. Primary hyperparathyroidism. Incidence, morbidity, and potential economic impact in a community. N Engl J Med. 1980; 302:189–193.15. Wermers RA, Khosla S, Atkinson EJ, Hodgson SF, O'Fallon WM, Melton LJ 3rd. The rise and fall of primary hyperparathyroidism: a population-based study in Rochester, Minnesota, 1965-1992. Ann Intern Med. 1997; 126:433–440.16. Rao DS, Agarwal G, Talpos GB, Phillips ER, Bandeira F, Mishra SK, et al. Role of vitamin D and calcium nutrition in disease expression and parathyroid tumor growth in primary hyperparathyroidism: a global perspective. J Bone Miner Res. 2002; 17:Suppl 2. N75–N80.17. Oltmann SC, Rajaei MH, Sippel RS, Chen H, Schneider DF. Primary hyperparathyroidism across the ages: presentation and outcomes. J Surg Res. 2014; 190:185–190.18. Harinarayan CV, Gupta N, Kochupillai N. Vitamin D status in primary hyperparathyroidism in India. Clin Endocrinol (Oxf). 1995; 43:351–358.19. Mollerup CL, Bollerslev J, Blichert-Toft M. Primary hyperparathyroidism: incidence and clinical and biochemical characteristics. a demographic study. Eur J Surg. 1994; 160:485–489.20. Vestergaard P. Primary hyperparathyroidism and nephrolithiasis. Ann Endocrinol (Paris). 2015; 76:116–119.21. Berger AD, Wu W, Eisner BH, Cooperberg MR, Duh QY, Stoller ML. Patients with primary hyperparathyroidism--why do some form stones? J Urol. 2009; 181:2141–2145.22. Rejnmark L, Vestergaard P, Mosekilde L. Nephrolithiasis and renal calcifications in primary hyperparathyroidism. J Clin Endocrinol Metab. 2011; 96:2377–2385.23. Chen HH, Chen YW, Wu CJ. Primary hyperparathyroidism in Taiwan: clinical features and prevalence in a single-center experience. Endocrine. 2010; 37:373–378.24. Silverberg SJ. Vitamin D deficiency and primary hyperparathyroidism. J Bone Miner Res. 2007; 22:Suppl 2. V100–V104.25. Ozbey N, Erbil Y, Ademoglu E, Ozarmagan S, Barbaros U, Bozbora A. Correlations between vitamin D status and biochemical/ clinical and pathological parameters in primary hyperparathyroidism. World J Surg. 2006; 30:321–326.26. Boudou P, Ibrahim F, Cormier C, Sarfati E, Souberbielle JC. A very high incidence of low 25 hydroxy-vitamin D serum concentration in a French population of patients with primary hyperparathyroidism. J Endocrinol Invest. 2006; 29:511–515.27. Jabiev AA, Lew JI, Garb JL, Sanchez YM, Solorzano CC. Primary hyperparathyroidism in the underinsured: a study of 493 patients. Surgery. 2012; 151:471–476.28. Han G, Wang O, Nie M, Zhu Y, Meng X, Hu Y, et al. Clinical phenotypes of Chinese primary hyperparathyroidism patients are associated with the calcium-sensing receptor gene R990G polymorphism. Eur J Endocrinol. 2013; 169:629–638.29. Kandil E, Tsai HL, Somervell H, Dackiw AP, Tufano RP, Tufaro AP, et al. African Americans present with more severe primary hyperparathyroidism than non-African Americans. Surgery. 2008; 144:1023–1026.30. Kim HG, Kim WY, Woo SU, Lee JB, Lee YM. Minimally invasive parathyroidectomy with or without intraoperative parathyroid hormone for primary hyperparathyroidism. Ann Surg Treat Res. 2015; 89:111–116.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple brown tumors in a patient with primary hyperparathyroidism
- Primary hyperparathyroidism erosion of the sternal ends of the clavicles, a new sign of hyperparathyroidism: a case report
- A Case of Primary Hyperparathyroidism Associated with Hypercalcemic Crisis and Systemic Calcinosis
- Primary Hyperparathyroidism in a Child with Urolithiasis: 1 Case
- A Case of Type 2 Diabetes Mellitus Improved after Surgical Treatment of Primary Hyperparathyroidism