Tuberc Respir Dis.
2016 Jul;79(3):179-183. 10.4046/trd.2016.79.3.179.
Acute Respiratory Failure Caused by Hepatopulmonary Fistula in a Patient with Hepatocellular Carcinoma
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. sunmich81@gmail.com
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea.
- 3Division of Hepatology, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea.
- KMID: 2326686
- DOI: http://doi.org/10.4046/trd.2016.79.3.179
Abstract
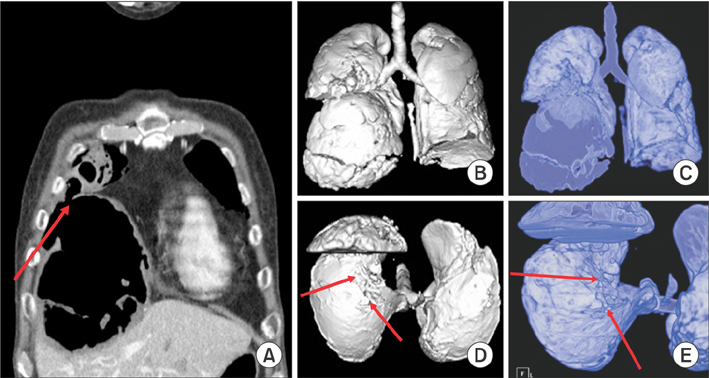
- A 59-year-old man presented with acute dyspnea following sudden productive cough and expectoration of a full cup of "blood-tinged" sputum. He had been diagnosed with hepatitis B virus-related hepatocellular carcinoma and had received transarterial chemoembolization 5 years ago for a 20-cm hepatic mass; he denied any history of hematemesis and the last esophagogastroduodenoscopy from a year ago showed absence of varix. Chest computed tomography (CT) with angiography showed new appearance of right basal lung consolidation but no bleeding focus. Despite the use of systemic antibiotics, the patient developed respiratory failure on day 7 of hospitalization. After intubation, a massive amount of brown sputum with anchovy-paste-like consistency was suctioned via the endotracheal tube. Bronchoscopic toileting was performed and the patient was extubated. In the ward, he continued to expectorate the brown sputum. On day 25 of hospitalization, a repeat CT scan showed simultaneous disappearance of the pneumonic consolidation and the necrotic fluid within the hepatic mass, suggesting the presence of a fistula. He has continued to receive systemic antibiotics, sorafenib, and entecavir, and follow up by respiratory and hepato-oncology specialists.
MeSH Terms
-
Angiography
Anti-Bacterial Agents
Carcinoma, Hepatocellular*
Cough
Dyspnea
Endoscopy, Digestive System
Fistula*
Follow-Up Studies
Hematemesis
Hemorrhage
Hepatitis B
Hospitalization
Humans
Intubation
Lung
Middle Aged
Pneumonia
Respiratory Insufficiency*
Respiratory Tract Fistula
Specialization
Sputum
Suction
Thorax
Tomography, X-Ray Computed
Varicose Veins
Anti-Bacterial Agents
Figure
Reference
-
1. Baudet JS, Medina A, Moreno A, Navazo L, Aviles J, Soriano A. Bronchobiliary fistula secondary to ruptured hepatocellular carcinoma into the bile duct. J Hepatol. 2004; 41:1066–1067.2. Strange C, Allen ML, Freedland PN, Cunningham J, Sahn SA. Biliopleural fistula as a complication of percutaneous biliary drainage: experimental evidence for pleural inflammation. Am Rev Respir Dis. 1988; 137:959–961.3. Yoon DH, Shim JH, Lee WJ, Kim PN, Shin JH, Kim KM. Percutaneous management of a bronchobiliary fistula after radiofrequency ablation in a patient with hepatocellular carcinoma. Korean J Radiol. 2009; 10:411–415.4. Ono F, Hiraga M, Omura N, Sato M, Yamamura A, Obara M, et al. Hemothorax caused by spontaneous rupture of hepatocellular carcinoma: a case report and review of the literature. World J Surg Oncol. 2012; 10:215.5. Lai EC, Lau WY. Spontaneous rupture of hepatocellular carcinoma: a systematic review. Arch Surg. 2006; 141:191–198.6. Kim JS, Yoon SK, Kim JA, Kim CW, Bae SH, Choi JY, et al. Long-term survival in a patient with ruptured hepatocellular carcinoma. Korean J Intern Med. 2009; 24:63–67.7. Islam M, Deka P, Kapur R, Ansari MA. Non-bleeding spontaneous rupture of hepatocellular carcinoma. Niger J Surg. 2013; 19:82–84.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Intracardiac Metastasis of Hepatocellular Carcinoma Presenting with Functional Tricuspid Valve Stenosis Accompanied with Hepatopulmonary Syndrome
- A Case of Transcatheter Arterial Embolization-nduced Hepatobronchial Fistula in a Patient with Hepatocellular Carcinoma
- A Case of Hepatosubphrenic Fistula Treated by Histoacryl(R) Injection by ERCP
- A Case of Duodenobiliary Fistula Caused by a Metal Stent in a Patient with Hepatocellular Carcinoma
- A Case of Respiratory Failure Caused by Gastropleural Fistula: A Case Report