J Korean Surg Soc.
2013 Jul;85(1):15-19.
Clinical implications of preoperative thyrotropin serum concentrations in patients who underwent thyroidectomy for nonfunctioning nodule(s)
- Affiliations
-
- 1Department of Surgery, Chungbuk National University Hospital, Cheongju, Korea. webjwpark@chungbuk.ac.kr
Abstract
- PURPOSE
Thyroid stimulating hormone (TSH) measurement is the most sensitive screening test for thyroid dysfunction. TSH is a well-known thyroid growth factor but its pathogenic role in thyroid oncogenesis remains to be clarified. The purpose of the present study was to evaluate the relationship between clinicopathologic characteristics of nonfunctioning thyroid nodules and preoperative TSH serum concentrations.
METHODS
Serum TSH concentrations can be affected by many factors. After exclusion of these confounding factors, a total of 126 patients who underwent thyroidectomy from Januray 2009 to December 2010 were included in this study. Average age was 45.4 +/- 10.6 years and male:female ratio was 1:2.9. There were 11 patients with benign nodules, 34 patients with papillary thyroid microcarcinoma (PTMC) of less than 5 mm in maximal diameter, 66 patients with PTMCs of more than 5 mm but not more than 10 mm in maximal diameter, and 15 patients with papillary thyroid carcinoma (PTC) of more than 10 mm in maximal diameter.
RESULTS
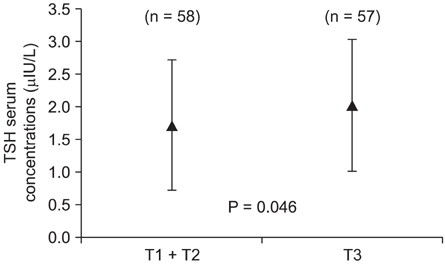
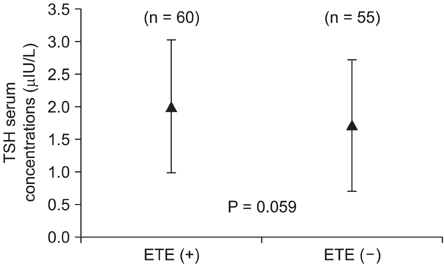
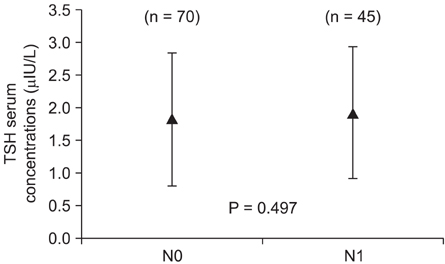
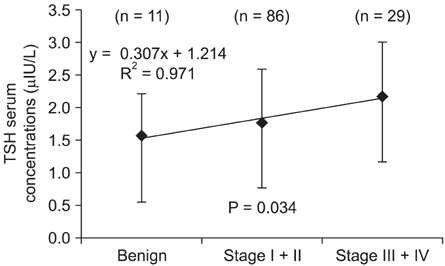
TNM stages of PTCs correlated with higher preoperative TSH serum concentrations. There were trends of higher preoperative TSH serum concentrations in patients who had extrathyroidal extension (P = 0.059) and advanced N stages (P = 0.120) but did not reach statistical significance. Patients' age, sex, and tumor volume did not seem to affect preoperative TSH serum concentrations significantly.
CONCLUSION
In patients who have PTCs without clinical, immunological, or ultrasonographic evidence of thyroiditis, higher preoperative TSH serum concentrations within the normal range might suggest advanced TNM stages.
MeSH Terms
Figure
Reference
-
1. Matsuo K, Friedman E, Gejman PV, Fagin JA. The thyrotropin receptor (TSH-R) is not an oncogene for thyroid tumors: structural studies of the TSH-R and the alpha-subunit of Gs in human thyroid neoplasms. J Clin Endocrinol Metab. 1993. 76:1446–1451.2. Derwahl M, Broecker M, Kraiem Z. Clinical review 101: thyrotropin may not be the dominant growth factor in benign and malignant thyroid tumors. J Clin Endocrinol Metab. 1999. 84:829–834.3. Mazzaferri EL. Thyroid cancer and Graves' disease: the controversy ten years later. Endocr Pract. 2000. 6:221–225.4. Shi Y, Zou M, Farid NR. Expression of thyrotrophin receptor gene in thyroid carcinoma is associated with a good prognosis. Clin Endocrinol (Oxf). 1993. 39:269–274.5. Papini E, Petrucci L, Guglielmi R, Panunzi C, Rinaldi R, Bacci V, et al. Long-term changes in nodular goiter: a 5-year prospective randomized trial of levothyroxine suppressive therapy for benign cold thyroid nodules. J Clin Endocrinol Metab. 1998. 83:780–783.6. Zelmanovitz F, Genro S, Gross JL. Suppressive therapy with levothyroxine for solitary thyroid nodules: a double-blind controlled clinical study and cumulative meta-analyses. J Clin Endocrinol Metab. 1998. 83:3881–3885.7. Vermiglio F, Lo Presti VP, Violi MA, Moleti M, Castagna MG, Finocchiaro MD, et al. Changes in both size and cytological features of thyroid nodule after levothyroxine treatment. Clin Endocrinol (Oxf). 2003. 59:347–353.8. Singh B, Shaha AR, Trivedi H, Carew JF, Poluri A, Shah JP. Coexistent Hashimoto's thyroiditis with papillary thyroid carcinoma: impact on presentation, management, and outcome. Surgery. 1999. 126:1070–1076.9. Jonklaas J, Sarlis NJ, Litofsky D, Ain KB, Bigos ST, Brierley JD, et al. Outcomes of patients with differentiated thyroid carcinoma following initial therapy. Thyroid. 2006. 16:1229–1242.10. Polyzos SA, Kita M, Efstathiadou Z, Poulakos P, Slavakis A, Sofianou D, et al. Serum thyrotropin concentration as a biochemical predictor of thyroid malignancy in patients presenting with thyroid nodules. J Cancer Res Clin Oncol. 2008. 134:953–960.11. Fiore E, Rago T, Provenzale MA, Scutari M, Ugolini C, Basolo F, et al. Lower levels of TSH are associated with a lower risk of papillary thyroid cancer in patients with thyroid nodular disease: thyroid autonomy may play a protective role. Endocr Relat Cancer. 2009. 16:1251–1260.12. Boelaert K, Horacek J, Holder RL, Watkinson JC, Sheppard MC, Franklyn JA. Serum thyrotropin concentration as a novel predictor of malignancy in thyroid nodules investigated by fine-needle aspiration. J Clin Endocrinol Metab. 2006. 91:4295–4301.13. Haymart MR, Greenblatt DY, Elson DF, Chen H. The role of intraoperative frozen section if suspicious for papillary thyroid cancer. Thyroid. 2008. 18:419–423.14. Gerschpacher M, Gobl C, Anderwald C, Gessl A, Krebs M. Thyrotropin serum concentrations in patients with papillary thyroid microcancers. Thyroid. 2010. 20:389–392.15. Jang YY, Kim CY, Hwang TY, Kim KD, Lee CH. Reference interval of serum thyroid hormones in healthy Korean adults. J Prev Med Public Health. 2008. 41:128–134.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes of Thyroid Function in Patients Undergoing Partial Thyroidectomy for Benign Thyroid Tumors
- Papillary Thyroid Carcinoma Hidden behind the Hot Nodule
- Papillary Thyroid Carcinoma Presented as a Hot Nodule with Hyperthyroidism
- Clinical Study of Post Thyroidectomy Hypocalcemia
- Graves' Disease: Can It Be Cured?