J Korean Soc Spine Surg.
2015 Jun;22(2):60-64. 10.4184/jkss.2015.22.2.60.
Surgical Outcome of Tuberculous Myelitis, Arachnoiditis and Spondylitis after Brain Meningitis: A Case Report
- Affiliations
-
- 1Department of Orthopaedic Surgery, Hanyang University College of Medicine, Seoul, Korea. cnkang65@hanyang.ac.kr
- 2Department of Orthopaedic Surgery, Sung-Ae Hospital, Seoul, Korea.
- KMID: 2322954
- DOI: http://doi.org/10.4184/jkss.2015.22.2.60
Abstract
- STUDY DESIGN: A case report.
OBJECTIVES
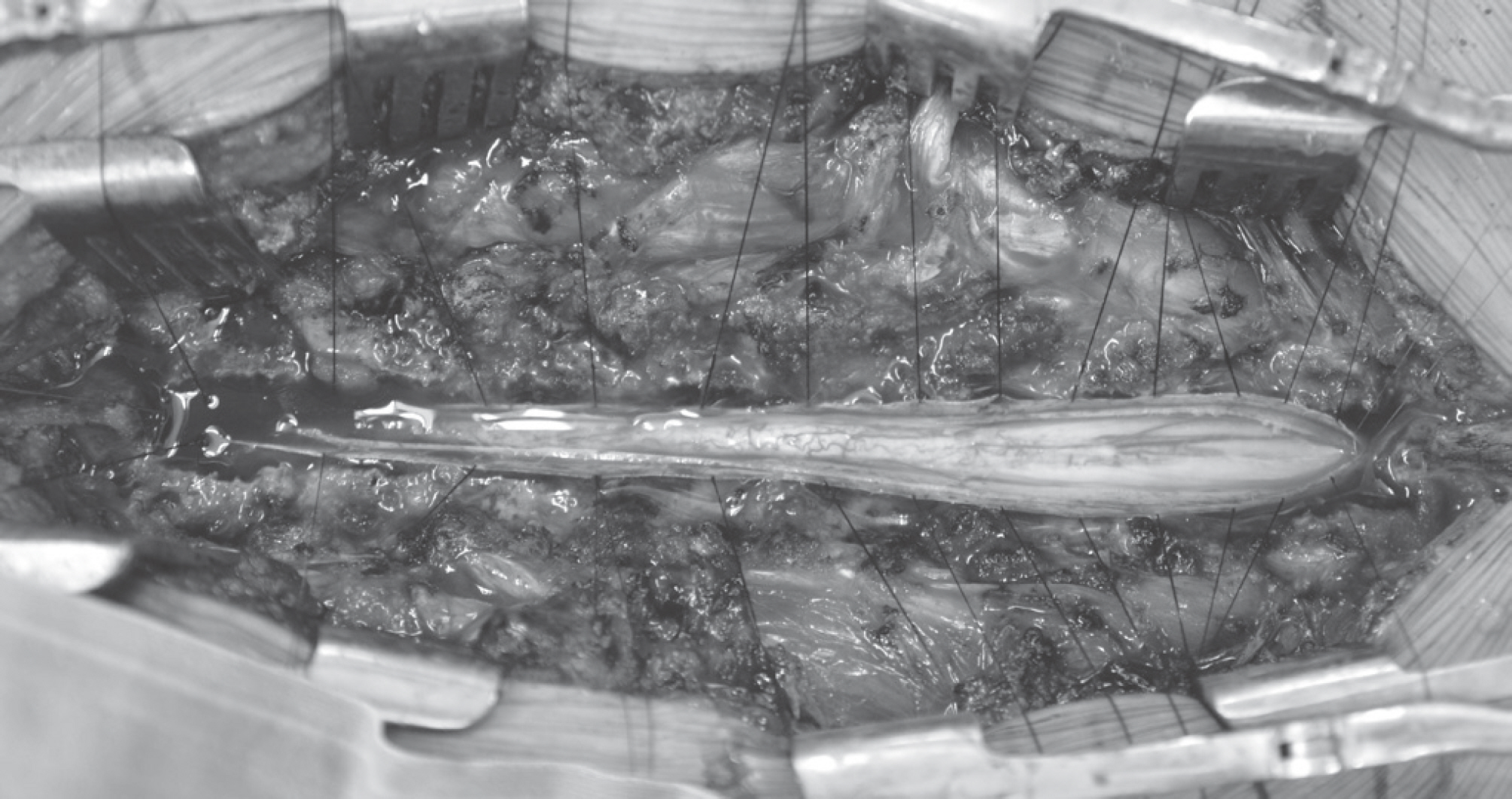
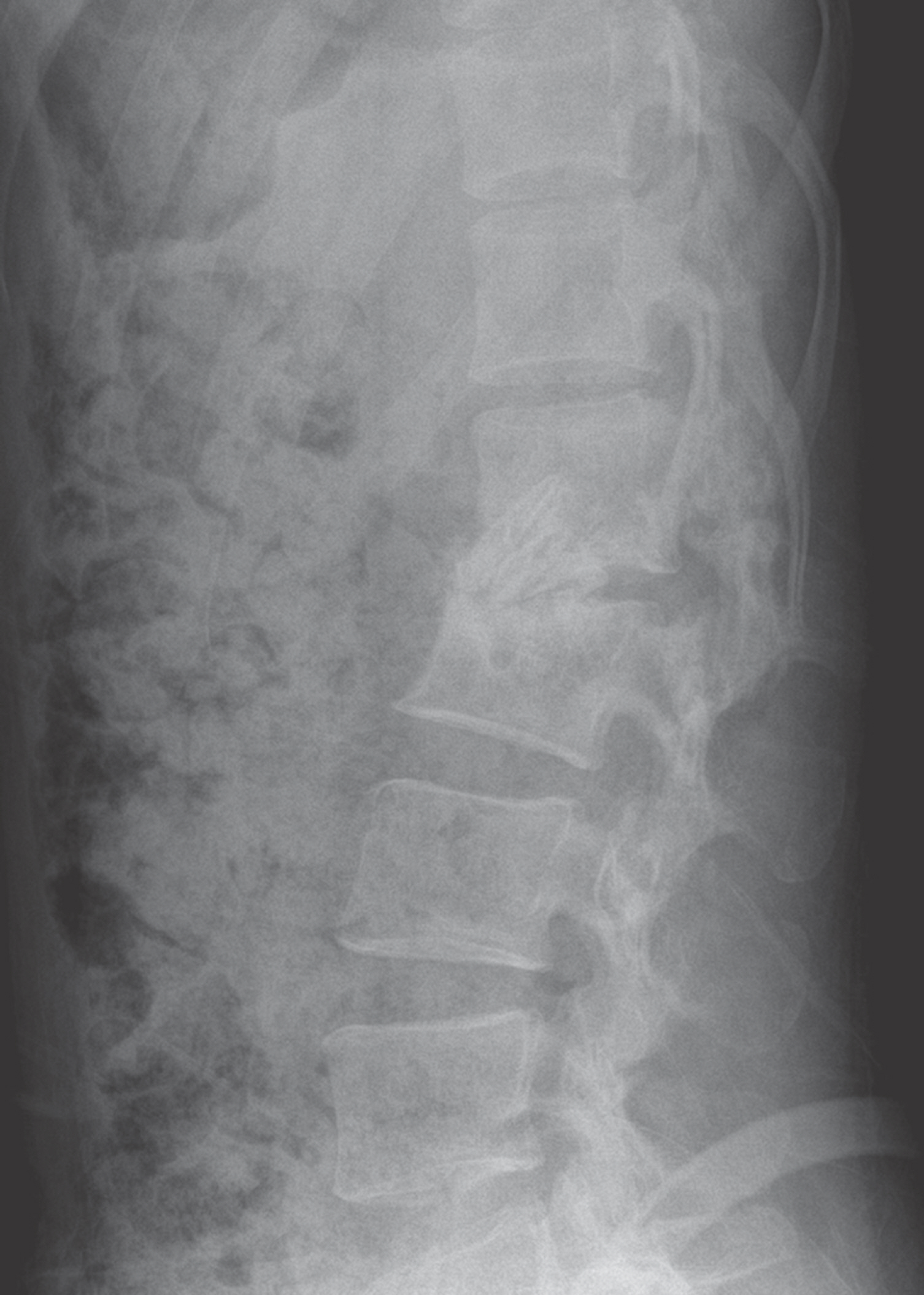
To report a rare case of a surgically treated tuberculous myelitis and arachnoiditis patient with incomplete paraplegia. SUMMARY OF LITERATURE REVIEW: Tuberculous myelitis and arachnoiditis is a rare disease with a high rate of neurologic deficit. This condition is treated using antituberculous medication and high-dose steroid therapy, but surgical treatment has rarely been reported and the outcomes vary. MATERIAL AND METHODS: A 29-year-old female had tuberculous myelitis and arachnoiditis. The patient was treated with antituberculous medication and high-dose steroid therapy, but the treatment failed and the patient could not walk because of incomplete paraplegia. The surgical treatment was performed twice; we decompressed by total laminectomy and debrided the infected arachnoid membrane. Four months after surgery, we performed anterior interbody fusion due to the development of spondylitis with kyphosis.
RESULTS
Three years after the first operation, the patient's neurologic state improved and she could walk 90 m without assistance.
CONCLUSIONS
Here, we report a very rare case of surgically treated tuberculous myelitis and arachnoiditis and provide a treatment option for this condition to spine surgeons.
Keyword
MeSH Terms
Figure
Reference
-
1. Almeida A. Tuberculosis of the spine and spinal cord. Eur J Radiol. 2005; 55:193–201.
Article2. Solanki GA. Spinal arachnoiditis. Palmer manual of neurosurgery. London: Churchill & Livingstone;1996. p. 769–74.3. Zuger A, Lowy FD. Tuberculosis of the brain, me-ninges, and spinal cord. Tuberculosis. Boston: Little & Brown;1996. p. 541–56.4. Jain AK. Treatment of tuberculosis of the spine with neurologic complications. Clin Orthop Relat Res. 2002; 398:75–84.
Article5. Jain AK, Dhammi IK. Tuberculosis of the spine: a review. Clin Orthop Relat Res. 2007; 460:39–49.6. Hristea A, Constantinescu RV, Exergian F, et al. Paraplegia due to non-osseous spinal tuberculosis: report of three cases and review of the literature. Int J Infect Dis. 2008; 12:425–9.
Article7. Poon TL, Ho WS, Pang KY, et al. Tuberculous meningitis with spinal tuberculous arachnoiditis. Hong Kong Med J. 2003; 9:59–61.8. Dastur H. Diagnosis and neurosurgical treatment of tuberculous disease of the CNS. Neurosurgical review. 1983; 6:111–7.
Article9. Chotmongkol V, Kitkuandee A, Limpawattana P. Tuberculous radiculomyelitis (arachnoiditis) associated with tuberculous meningitis. Southeast Asian J Trop Med Public Health. 2005; 36:722–4.10. Rand C, Smith MA. Anterior spinal tuberculosis: paraplegia following laminectomy. Ann R Coll Surg Engl. 1989; 71:105–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Tuberculous Optochiasmatic Arachnoiditis
- A Case of Diffuse Tuberculous Arachnoiditis Accompanying Tuberculous Meningoencephalitis
- Tuerculous Brain Abscess on Sellar Region: A Case Report
- Surgical Management of Syringomyelia Associated with Spinal Adhesive Arachnoiditis, a Late Complication of Tuberculous Meningitis: A Case Report
- A Case of Syringomyelia Following Cured Tuberculous Meningitis