J Korean Soc Spine Surg.
2005 Dec;12(4):349-357.
Comparison of the Results of Percutaneous Vertebroplasty for Treating Osteoporotic Vertebral Compression Fracture and Posttraumatic Vertebral Collapse (Kummell's disease)
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, Inje University, Ilsan Paik Hospital, Kyonggi, Korea. kimjh@ilsanpaik.ac.kr
- 2Department of Orthopaedic Surgery, College of Medicine, Inje University, Seoul Paik Hospital, Seoul Korea.
Abstract
- STUDY DESIGN: The comparison was based on the radiographc and clinically differences of 96 vertebroplasty cases.
PURPOSE: This study evaluated the clinical and radiological results of performing percutaneous vertebroplasty for acute or subacute osteoporotic vertebral compression fracture (group A) and for posttraumatic vertebral collapse (Kummell's disease) (group B).
SUMMARY OF LITERATURE REVIEW: Percutaneous vertebroplasty is a minimal invasive procedure for the treatment of a painful collapsed vertebral body
MATERIALS AND METHODS
We experienced 67 cases of group A and 29 cases of group B, and we followed these patients for 2 years or more. We evaluated the clinical results by using the serial visual analogue scale (VAS) and the radiological results were evaluated by measuring the restoration of the anterior vertebral height and the change of the kyphotic angle. We also compared both groups for their bone mineral density (BMD) and new fracture rate.
RESULTS
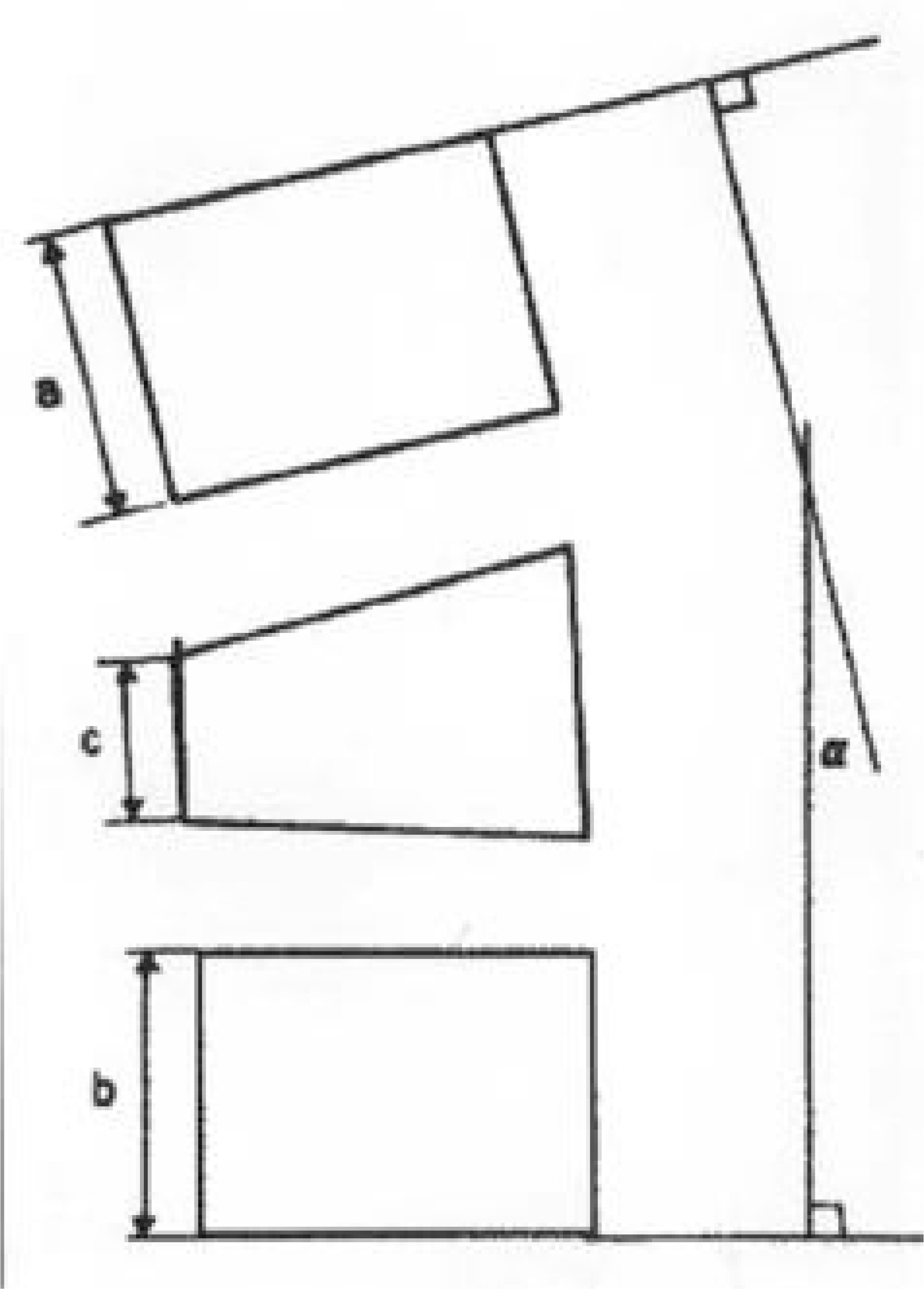
Statistically significant pain relief was obtained by both groups in the perioperative period. The average VAS change was 6.5 (from 8.7 preoperatively to 2.2 postoperatively) in group A, and 7.1 (from 9.1 preoperatively to 2.0 postoperatively) in group B on a 10 point pain scale. The anterior vertebral height increased an average of 4.9mm (16.5%), (from 16.8mm preoperatively to 21.7 mm postoperatively) in group A, and 6.5 mm (21%) (from 12.8 mm preoperatively to 19.3 mm postoperatively) in group B on the perioperative period. But the height was minimally decreased more that it was measured at the immediate postoperative period: 18.7 mm in group A, and 16.2 mm in group B on the last follow up. The kyphotic angle was restored an average of 5.2 degrees (from 32.4 degrees preoperatively to 27.2 degrees postoperatively) in group A, and 4.9 degrees (from 39.5 degrees preoperatively to 34.6 degrees postoperatively) in group B on the perioperative period. But the angle was increased more than that measured preoperatively: about 1.7 degree in group A and group B on the last follow up. There's no significant difference in the BMD between the groups. New fracture developed in 17.9% (12) of group A, and 20.7% (6) of group B. We did this procedure for 15 cases of new fracture, and then the VAS change was an average 5.0 immediately after the operation.
CONCLUSIONS
Percutaneous vertebroplasty was an effective treatment method for both groups and there were no statistically significant differences in the clinical and radiological results. Care must be taken due to the relatively high rate of new fracture and this can be resolved by repeat vertebroplasty
MeSH Terms
Figure
Reference
-
1). Deramond H, Depriester C, Galibert P, and Daniel Le Gar sl. Percutaneous vertebroplasty with polymethyl -methacrylate. technique, indications and results. Radiologic clinics of North America. 36:533–546. 1998.2). Hammerger KW, and DeWald RL. Senile burst fracture: A complication of osteoporosis. Orthop Trans. 13:97. 1989.3). Benedek TG, Nicholas JJ, and John Reece G. Kummell's disease: A rare cause of posttraumatic back pain. Arthritis Rheum. 23:653. 1980.4). Brower AC and Downey EF. Kummell's disease: report of a case with serial radiographs. Radiology. 141:363–364. 1981.5). Steel HH. Kummell's disease. American Journal of Surgery. 81:161–167. 1951.6). Ha KY, Moon MS, Lee NG, and Jeong CH. Kummell's disease-Report of three cases with serial radiographs. J of Korean Society of Spine Surgery. 2:131–136. 1995.7). Larde D, Mathieu D, Frija J, Gaston A, and Vasile N. Spinal vacuum phenomenon: CT diagnosis and significance. J comput assist tomogr. 6:671–6. 1982.8). Salomon C, and Chopin D. Spinal cord compression: An exceptional complication of spinal osteoporosis, Spine. 13:222–224. 1988.9). Schabel SI, Moore TE, Stanley JH, Javid LH, and Rit-tenberg GM. Vertebral vacuum phenomenon. Skeletal Radiology. 4:153–156. 1979.
Article10). Van Eenenaam DP, and EI-Khoury GY. Delayed post-traumatic vertebral collapse(Kummell's disease). case report with serial radiographs, computed tomographic scans and bone scans. Spine. 18:1236–1241. 1993.11). Hashimoto K, Yasui N, Yamagishi M, Kojimoto H, Mizuno K, and Shimomura Y. Intravertebral vacuum cleft in the fifth lumbar vertebra. Spine. 14:351–354. 1989.
Article12). Ha KY, Kim KW, Park SJ, Paek DH, and Ha JH. The surgical treatment of osteoporotic vertebral collapse caused by minor trauma. J of Korean Orthop ‘ assoc. 33:105–112. 1998.
Article13). Cho YS, Cho SD, Kim BS, Park TW, Lew SG, and Hwang SY. Kum me ll’s disease managed by percutaneous vertebroplasty. J of Korea Spine Surg. 8:226–234. 2001.14). Cho YS, Cho SD, Kim BS, Park TW, Lew SG, and Cho SH. Percutaneous vertebroplasty for osteoporotic compression fractures. J. of Korean Orthop. assoc. 37:13–18. 2002.15). Hermann G, Goldblatt J, and Desnick RJ. Kummell's disease: Delayed collapse of the traumatized spine in a patient with Gaucher type I disease. Br J Radiol. 57:833–835. 1984.16). Golimbu C, Firooznia H, and Mahvash R. the intravertebral vacuum sign. Spine. 11:1040–3. 1985.
Article17). Kumpan W, Salomonowitz E, Seidl G, and Wittich GR. The intravertebral vacuum phenomenon. Skeletal Radiol. 15:444–447. 1986.
Article18). Resnick D, Niwayama G, Guerra J, Vint V, and Usselman J. Spinal vacuum phenomena: Anatomical study and review. Radiology. 139:341–348. 1981.
Article19). Maldague BE, Noel HM, and Malghem JJ. T h e intravertebral vacuum cleft: A sign of ischemic vertebral collapse. Radiology. 129:23–29. 1978.20). Heini PF, Walchli B, and Berlemann U. Percutaneous Transpedicular vertebroplasty with PMMA: Operative technique and early results. A prospective study for the treatment of osteoporotic compression fractures. Eur Spine J. 9:445–50. 2000.21). Mathis JM, Barr JD, Stephen MB, Barr MS, Jensen ME, and Deramond H. Percutaneous vertebroplasty: A degloving standard of care for vertebral compression fractures. AJNR Am J Neuroradiol. 22:373–381. 2001.22). Benedek TG, and Nicholas JJ. Delayed traumatic vertebral body compression fracture part Ⅱ: Pathologic features. Semin Arthritis Rheum. 10(4):271–277. 1981.23). Grados F, Depriester C, Cayrolle G, Hardy N, Deramond H, and Fardellone P. Long-term observation of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology (Oxford). 39:1410–4. 2000.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posttraumatic Delayed Vertebral Collapse : Kummell's Disease
- Spontaneous Vertebral Reduction during the Procedure of Kyphoplasty in a Patient with Kummell's Disease
- A Case of Delayed Post-traumatic Vertebral Collapse (Kummell's Disease) Treated by Vertebroplasty: A case report
- Is Kummell's Disease a Independent Disease Entity?: Two Case Report
- Short-term Treatment Comparison of Teriparatide and Percutaneous Vertebroplasty in Patients with Acute Osteoporotic Vertebral Compression Fractures