J Korean Soc Radiol.
2013 May;68(5):385-390.
Correlation between the Volume of a Lesion or Physical Training, and Regression Time, in Congenital Torticollis Patients
- Affiliations
-
- 1Department of Radiology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. dwultra@lycos.co.kr
Abstract
- PURPOSE
This study aimed to evaluate any correlation between the volume of a lesion or physical training, and regression time, in congenital torticollis patients.
MATERIALS AND METHODS
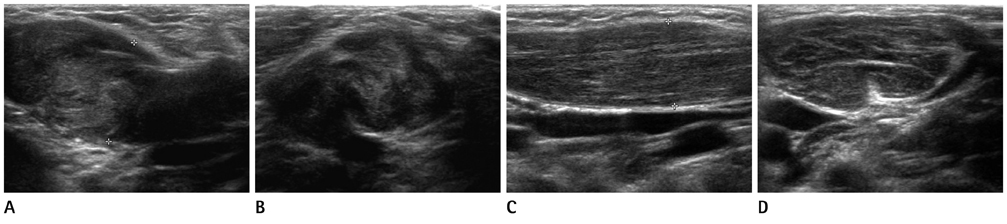
From January 2007 to December 2010, 63 infants and young children underwent neck ultrasound (US), as congenital torticollis was clinically suspected. We statistically analyzed the correlation between the volume of a lesion or physical training and the regression time, when successful regression was defined as no visible lesion on follow-up US, or no palpation of the lesion on clinical follow-up.
RESULTS
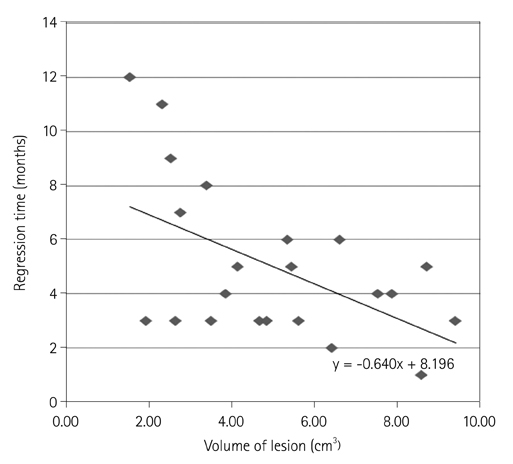
Among 63 patients, 48 were sonographically diagnosed with congenital torticollis: normal delivery (n = 39) and c-sec (n = 9). Among them, 24 were clinically followed up, and 22 showed complete regression. Among 24 patients, 9 underwent physical training, and 7 showed complete regression after physical training. There was a negative correlation between the volume of a lesion and the regression time (p = 0.011), but there was no statistical significance between physical training and the regression time (p = 0.15).
CONCLUSION
In congenital torticollis patients, the volume of a lesion was in reverse proportion to the regression time, and physical training may be unhelpful for a decrease in regression time.
Figure
Reference
-
1. Ballock RT, Song KM. The prevalence of nonmuscular causes of torticollis in children. J Pediatr Orthop. 1996. 16:500–504.2. Binder H, Eng GD, Gaiser JF, Koch B. Congenital muscular torticollis: results of conservative management with long-term follow-up in 85 cases. Arch Phys Med Rehabil. 1987. 68:222–225.3. Cheng JC, Au AW. Infantile torticollis: a review of 624 cases. J Pediatr Orthop. 1994. 14:802–808.4. Cheng JC, Wong MW, Tang SP, Chen TM, Shum SL, Wong EM. Clinical determinants of the outcome of manual stretching in the treatment of congenital muscular torticollis in infants. A prospective study of eight hundred and twenty-one cases. J Bone Joint Surg Am. 2001. 83-A:679–687.5. Haque S, Bilal Shafi BB, Kaleem M. Imaging of torticollis in children. Radiographics. 2012. 32:557–571.6. Chan YL, Cheng JC, Metreweli C. Ultrasonography of congenital muscular torticollis. Pediatr Radiol. 1992. 22:356–360.7. Lin JN, Chou ML. Ultrasonographic study of the sternocleidomastoid muscle in the management of congenital muscular torticollis. J Pediatr Surg. 1997. 32:1648–1651.8. Cheng JC, Metreweli C, Chen TM, Tang S. Correlation of ultrasonographic imaging of congenital muscular torticollis with clinical assessment in infants. Ultrasound Med Biol. 2000. 26:1237–1241.9. Som P, Curtin H. Head and Neck Imaging. 2011. St. Louis: Mosby;2715–2718.10. Davids JR, Wenger DR, Mubarak SJ. Congenital muscular torticollis: sequela of intrauterine or perinatal compartment syndrome. J Pediatr Orthop. 1993. 13:141–147.11. Hollier L, Kim J, Grayson BH, McCarthy JG. Congenital muscular torticollis and the associated craniofacial changes. Plast Reconstr Surg. 2000. 105:827–835.12. Macdonald D. Sternomastoid tumour and muscular torticollis. J Bone Joint Surg Br. 1969. 51:432–443.13. Berlin H. The differential diagnosis and management of torticollis in children. Phys Med Rehabil Clin N Am. 2000. 14:197–206.14. Wei JL, Schwartz KM, Weaver AL, Orvidas LJ. Pseudotumor of infancy and congenital muscular torticollis: 170 cases. Laryngoscope. 2001. 111(4 Pt 1):688–695.15. Slate RK, Posnick JC, Armstrong DC, Buncic JR. Cervical spine subluxation associated with congenital muscular torticollis and craniofacial asymmetry. Plast Reconstr Surg. 1993. 91:1187–1195.16. Canale ST, Griffin DW, Hubbard CN. Congenital muscular torticollis. A long-term follow-up. J Bone Joint Surg Am. 1982. 64:810–881.17. Chang PY, Tan CK, Huang YF, Sheu JC, Wang NL, Yeh ML, et al. Torticollis: a long-term follow-up study. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi. 1996. 37:173–177.18. Cheng JC, Tang SP, Chen TM, Wong MW, Wong EM. The clinical presentation and outcome of treatment of congenital muscular torticollis in infants--a study of 1,086 cases. J Pediatr Surg. 2000. 35:1091–1096.19. Ippolito E, Tudisco C, Massobrio M. Long-term results of open sternocleidomastoid tenotomy for idiopathic muscular torticollis. J Bone Joint Surg Am. 1985. 67:30–38.20. Ho BC, Lee EH, Singh K. Epidemiology, presentation and management of congenital muscular torticollis. Singapore Med J. 1999. 40:675–679.21. Persing J, James H, Swanson J, Kattwinkel J. American Academy of Pediatrics Committee on Practice and Ambulatory Medicine, Section on Plastic Surgery and Section on Neurological Surgery. Prevention and management of positional skull deformities in infants. American Academy of Pediatrics Committee on Practice and Ambulatory Medicine, Section on Plastic Surgery and Section on Neurological Surgery. Pediatrics. 2003. 112(1 Pt 1):199–202.22. Yim SY, Lee IY, Park MC, Kim JH. Differential diagnosis and management of abnormal posture of the head and neck. J Korean Med Assoc. 2009. 52:705–718.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Familial Congenital Muscular Torticollis: A Case Report
- Congenital Torticollis with Bilateral Sternocleidomastoid Muscle Contracture
- The Correlation between Outcome and Ultrasonographic Findingsin Congenital Muscular Torticollis
- Support Vector Regression-based Model to Analyze Prognosis of Infants with Congenital Muscular Torticollis
- Ultrasonographic Findings in Torticollis