J Korean Acad Prosthodont.
2008 Dec;46(6):602-609.
Marginal tissue response to different Implant neck design
- Affiliations
-
- 1Department of Prosthodontics, Yonsei University College of Dentistry, Seoul, Korea. donghoohan@yuhs.ac
- 2Department of Oral and Maxillofacial Surgery, Yonsei University College of Dentistry, Seoul, Korea.
Abstract
-
STATEMENT OF PROBLEM: Loss of the marginal bone to the first thread have been accepted but continuous effort have been made to reduce this bone loss by varying implant design and surface texture.
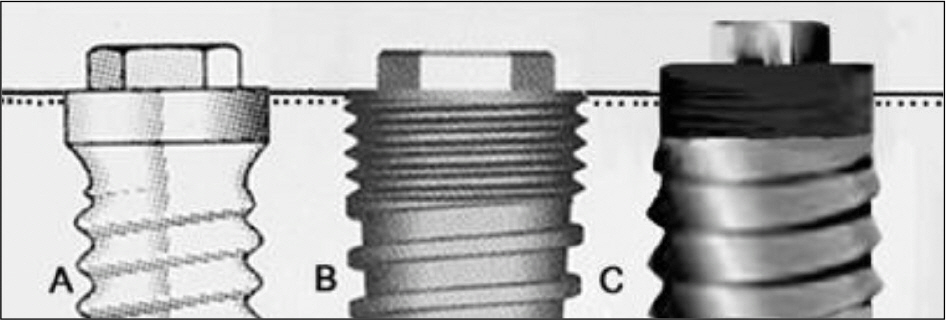
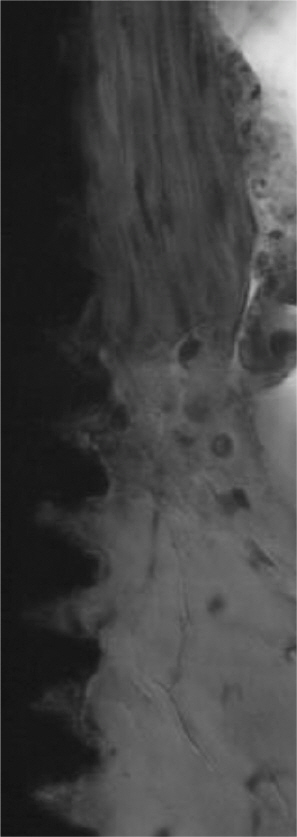
PURPOSE: This animal study has examined the histomorphometric variations between implants with micro-thread, micro-grooved and turned surfaced neck designs.
MATERIAL AND METHODS: Four mongrel dogs have been used the premolars removed and left to heal for three months. One of each implant systems with turned neck, micro-thread and micro-grooved were placed according to the manufacturers' protocol and left submerged for 8 and 12 weeks. These were then harvested for histological examination.
RESULTS
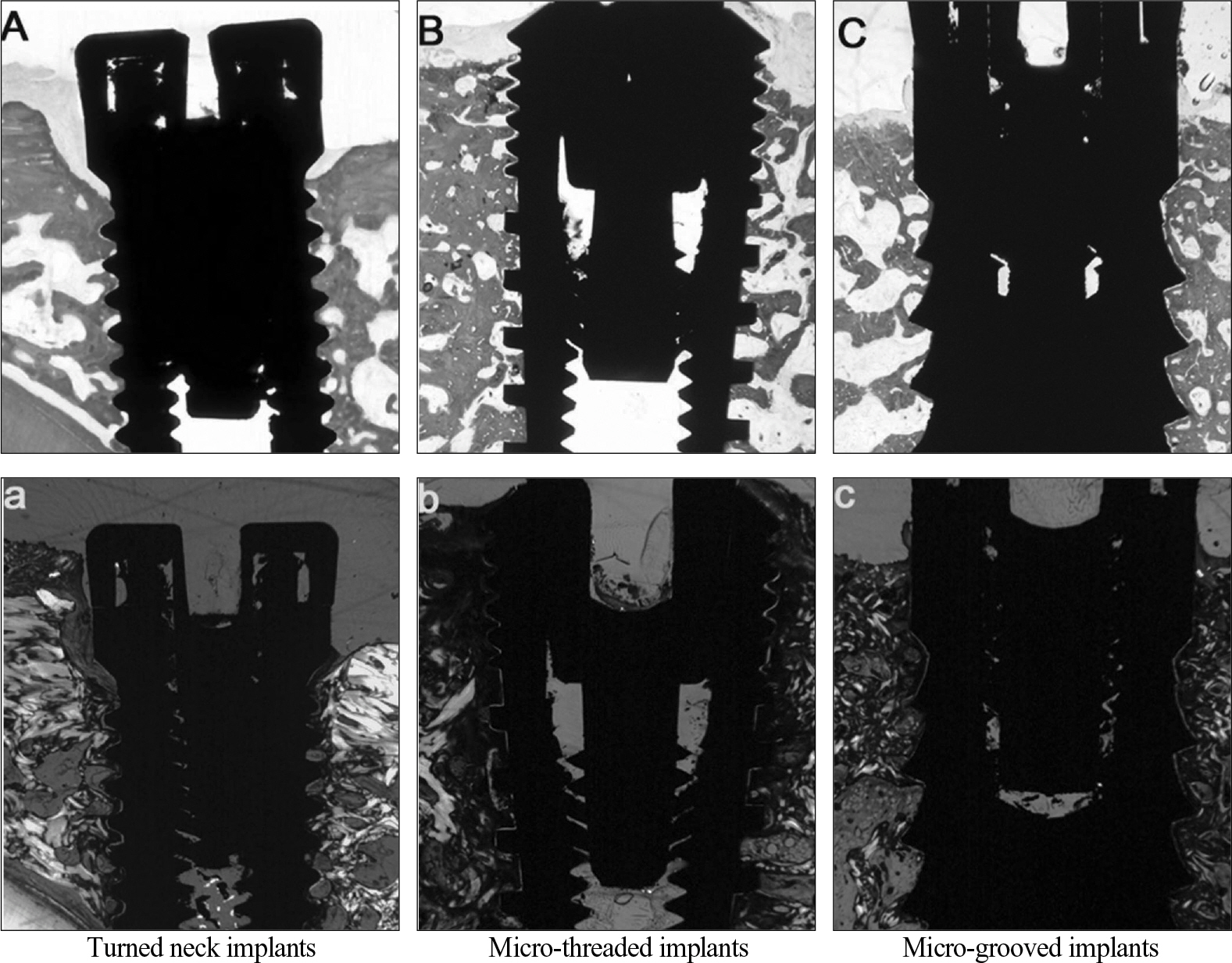
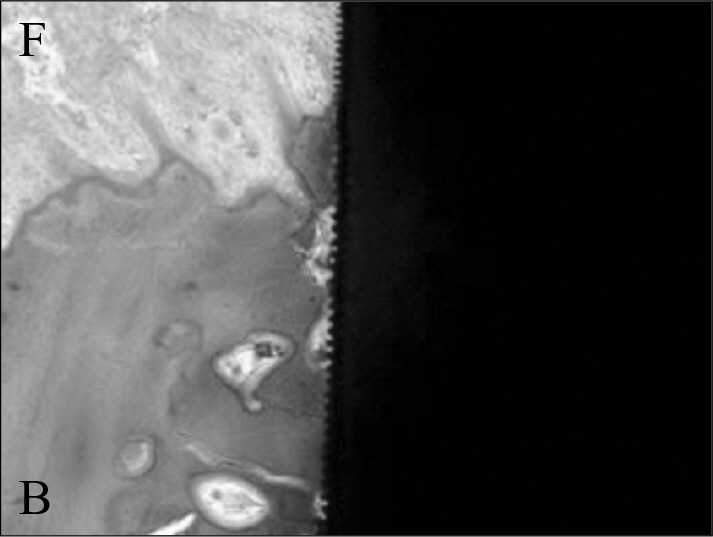
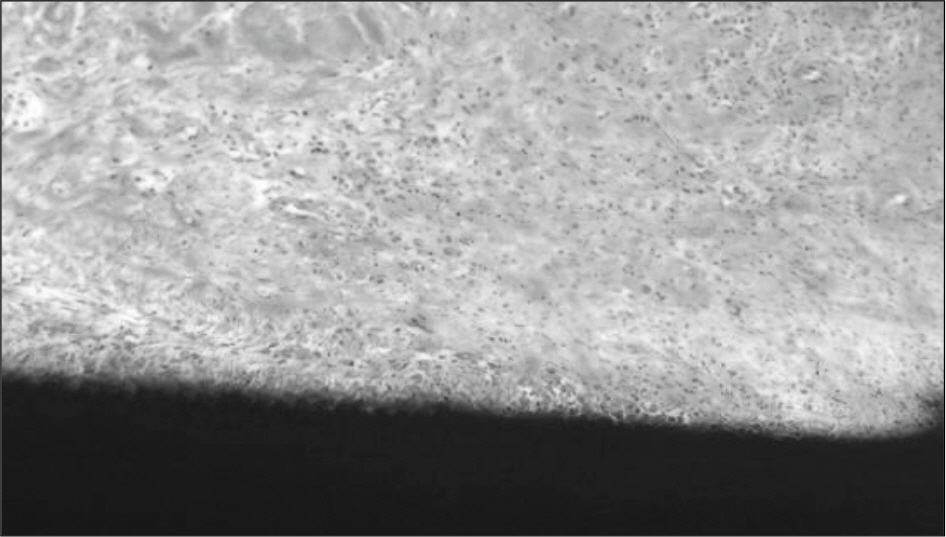
The histologically all samples were successfully ossointegrated and active bone remodelling adjacent to implants. With the micro-grooved implants 0.40 mm and 0.26 mm of the marginal bone level changes were observed at 8 and 12 weeks respectively. The micro-threaded implants had changes of 0.79 mm and 0.56 mm at 8 and 12 weeks respectably. The turned neck designed implants had marginal bone level changes of 1.61 mm and 1.63 mm in 8 and 12 weeks specimens. A complex soft tissue arrangement could be observed against micro-threaded and micro-grooved implant surfaces.
CONCLUSION
Within the limitations of this study, it could be concluded that implants with micro-grooved had the least and the turned neck designed implants had the most changes in the marginal bone level. The textured implant surfaces affect soft tissue responses.
Keyword
Figure
Reference
-
1.Adell R., Lekholm U., Rockler B., Bra ° nemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981. 10:387–416.
Article2.Albrektsson T., Zarb G., Worthington P., Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986. 1:11–25.3.Smith DE., Zarb GA. Criteria for success of osseointegrated endosseous implants. J Prosthet Dent. 1989. 62:567–72.
Article4.Lekholm U., Gunne J., Henry P., Higuchi K., Linde ´ n U., Bergstro ¨ m C., van Steenberghe D. Survival of the Bra ° nemark implant in partially edentulous jaws: a 10-year prospective multicenter study. Int J Oral Maxillofac Implants. 1999. 14:639–45.5.Buser D., Mericske-Stern R., Bernard JP., Behneke A., Behneke N., Hirt HP., Belser UC., Lang NP. Long-term evaluation of non-submerged ITI implants. Part 1: 8-year life table analysis of a prospective multicenter study with 2359 implants. Clin Oral Implants Res. 1997. 8:161–72.
Article6.Jemt T., Pettersson P. A 3-year follow-up study on single implant treatment. J Dent. 1993. 21:203–8.
Article7.Chou CT., Morris HF., Ochi S., Walker L., DesRosiers D. AICRG, Part II: Crestal bone loss associated with the Ankylos implant: loading to 36 months. J Oral Implantol. 2004. 30:134–43.
Article8.de Bruyn H., Collaert B., Linde ´ n U., Bjo ¨ rn AL. Patient' s opinion and treatment outcome of fixed rehabilitation on Bra ° nemark implants. A 3-year follow-up study in private dental practices. Clin Oral Implants Res. 1997. 8:265–71.9.Kan JY., Rungcharassaeng K., Lozada J. Immediate placement and provisionalization of maxillary anterior single implants: 1-year prospective study. Int J Oral Maxillofac Implants. 2003. 18:31–9.10.Tarnow DP., Cho SC., Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000. 71:546–9.
Article11.Khang W., Feldman S., Hawley CE., Gunsolley J. A multicenter study comparing dual acid-etched and machined-surfaced implants in various bone qualities. J Periodontol. 2001. 72:1384–90.
Article12.Ellingsen JE., Johansson CB., Wennerberg A., Holme ´ n A. Improved retention and bone-tolmplant contact with fluoride-modified titanium implants. Int J Oral Maxillofac Implants. 2004. 19:659–66.13.Jung YC., Han CH., Lee KW. A 1-year radiographic evaluation of marginal bone around dental implants. Int J Oral Maxillofac Implants. 1996. 11:811–8.14.Abrahamsson I., Berglundh T., Wennstro ¨ m J., Lindhe J. Department of Periodontology, Go ¨teborg University, Sweden. The peri-implant hard and soft tissues at different implant systems. A comparative study in the dog. Clin Oral Implants Res. 1996. 7:212–9.15.Astrand P., Engquist B., Dahlgren S., Gro ¨ ndahl K., Engquist E., Feldmann H. Astra Tech and Bra ° nemark system implants: a 5-year prospective study of marginal bone reactions. Clin Oral Implants Res. 2004. 15:413–20.16.Hansson S. The implant neck: smooth or provided with retention elements. A biomechanical approach. Clin Oral Implants Res. 1999. 10:394–405.
Article17.Frenkel SR., Simon J., Alexander H., Dennis M., Ricci JL. Osseointegration on metallic implant surfaces: effects of microgeometry and growth factor treatment. J Biomed Mater Res. 2002. 63:706–13.
Article18.Sennerby L., Ericson LE., Thomsen P., Lekholm U., Astrand P. Structure of the bone-titanium interface in retrieved clinical oral implants. Clin Oral Implants Res. 1991. 2:103–11.
Article19.Mohammadi S., Esposito M., Hall J., Emanuelsson L., Krozer A., Thomsen P. Long-term bone response to titanium implants coated with thin radiofrequent magnetron-sputtered hydroxyapatite in rabbits. Int J Oral Maxillofac Implants. 2004. 19:498–509.20.Kan JY., Rungcharassaeng K., Lozada J. Immediate placement and provisionalization of maxillary anterior single implants: 1-year prospective study. Int J Oral Maxillofac Implants. 2003. 18:31–9.21.Gotfredsen K. A 5-year prospective study of single-tooth replacements supported by the Astra Tech implant: a pilot study. Clin Implant Dent Relat Res. 2004. 6:1–8.
Article22.Tarnow D., Elian N., Fletcher P., Froum S., Magner A., Cho SC., Salama M., Salama H., Garber DA. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J Periodontol. 2003. 74:1785–8.
Article23.Tarnow DP., Cho SC., Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000. 71:546–9.
Article24.Pikos MA. Block autografts for localized ridge augmentation: Part I. The posterior maxilla. Implant Dent. 1999. 8:279–85.25.Woo I., Le BT. Maxillary sinus floor elevation: review of anatomy and two techniques. Implant Dent. 2004. 13:28–32.
Article26.McAllister BS. Histologic and radiographic evidence of vertical ridge augmentation utilizing distraction osteogenesis: 10 consecutively placed distractors. J Periodontol. 2001. 72:1767–79.
Article27.Mazzonetto R., Serra E., Silva FM., Ribeiro Torezan JF. Clinical assessment of 40 patients subjected to alveolar distraction osteogenesis. Implant Dent. 2005. 14:149–53.
Article28.Schwartz-Arad D., Levin L., Ashkenazi M. Treatment options of untreatable traumatized anterior maxillary teeth for future use of dental implantation. Implant Dent. 2004. 13:11–9.
Article29.Berglundh T., Abrahamsson I., Lang NP., Lindhe J. De novo alveolar bone formation adjacent to endosseous implants. Clin Oral Implants Res. 2003. 14:251–62.
Article30.Astrand P., Engquist B., Anze ´ n B., Bergendal T., Hallman M., Karlsson U., Kvint S., Lysell L., Rundcrantz T. Nonsubmerged and submerged implants in the treatment of the partially edentulous maxilla. Clin Implant Dent Relat Res. 2002. 4:115–27.31.Engquist B., Astrand P., Anzen B., Dahlgren S., Engquist E., Feldmann H., Karlsson U., Nord PG., Sahlholm S., Sva ¨ rdstr-o ¨ m P. Simplified methods of implant treatment in the edentulous lower jaw. A controlled prospective study. Part I: one-stage versus two-stage surgery. Clin Implant Dent Relat Res. 2002. 4:93–103.
Article32.Quirynen M., Naert I., van Steenberghe D. Fixture design and overload influence marginal bone loss and fixture success in the Bra ° nemark system. Clin Oral Implants Res. 1992. 3:104–11.33.Wiskott HW., Belser UC. Lack of integration of smooth titanium surfaces: a working hypothesis based on strains generated in the surrounding bone. Clin Oral Implants Res. 1999. 10:429–44.
Article34.Hansson S., Werke M. The implant thread as a retention element in cortical bone: the effect of thread size and thread profile: a finite element study. J Biomech. 2003. 36:1247–58.
Article35.Ricci JL., Charvet J., Frenkel R., Chang P., Nadkarni P., Turner J., Alexander H. Bone response to laser microtextured surfaces. In: Bone Engineering, edited by JE Davies, Em2 Inc., Toronto, Ont. Canada, Chapter 25, pp. 282–94. 2000.36.Buser D., Weber HP., Donath K., Fiorellini JP., Paquette DW., Williams RC. Soft tissue reactions to non-submerged unloaded titanium implants in beagle dogs. J Periodontol. 1992. 63:225–35.
Article37.Abrahamsson I., Zitzmann NU., Berglundh T., Linder E., Wennerberg A., Lindhe J. The mucosal attachment to titanium implants with different surface characteristics: an experimental study in dogs. J Clin Periodontol. 2002. 29:448–55.
Article38.Chehroudi B., Gould TR., Brunette DM. Titanium-coated micromachined grooves of different dimensions affect epithelial and connective-tissue cells differently in vivo. J Biomed Mater Res. 1990. 24:1203–19.39.Kim H., Murakami H., Chehroudi B., Textor M., Brunette DM. Effects of surface topography on the connective tissue attachment to subcutaneous implants. Int J Oral Maxillofac Implants. 2006. 21:354–65.40.Albrektsson T. Is surgical skill more important for clinical success than changes in implant hardware? Clin Implant Dent Relat Res. 2001. 3:174–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Considerations in implant crestal module to preserve peri-implant tissue
- Effects of implant collar design on marginal bone and soft tissue
- The effect of implant system with reverse beveled platform design on marginal bone stress distribution
- The influence of collar design on peri-implant marginal bone tissue
- Three-dimensional finite element analysis for influence of marginal bone resorption on stress distribution in internal conical joint type implant fixture