Tuberc Respir Dis.
2014 Apr;76(4):184-187.
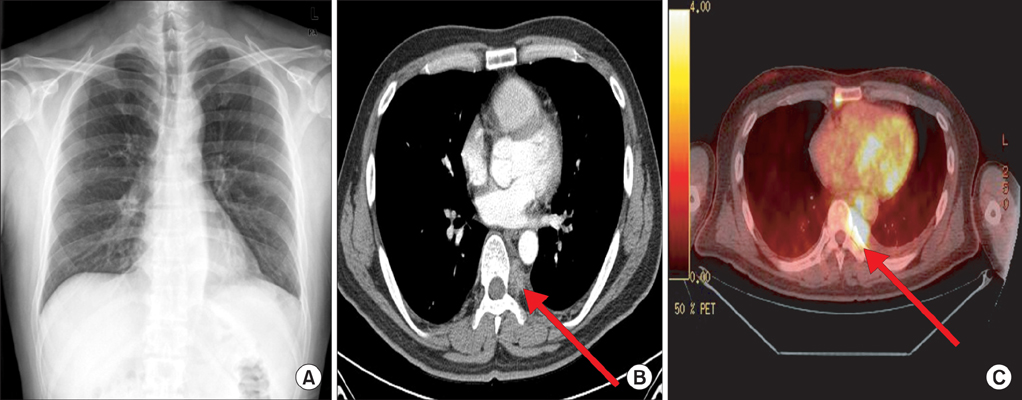
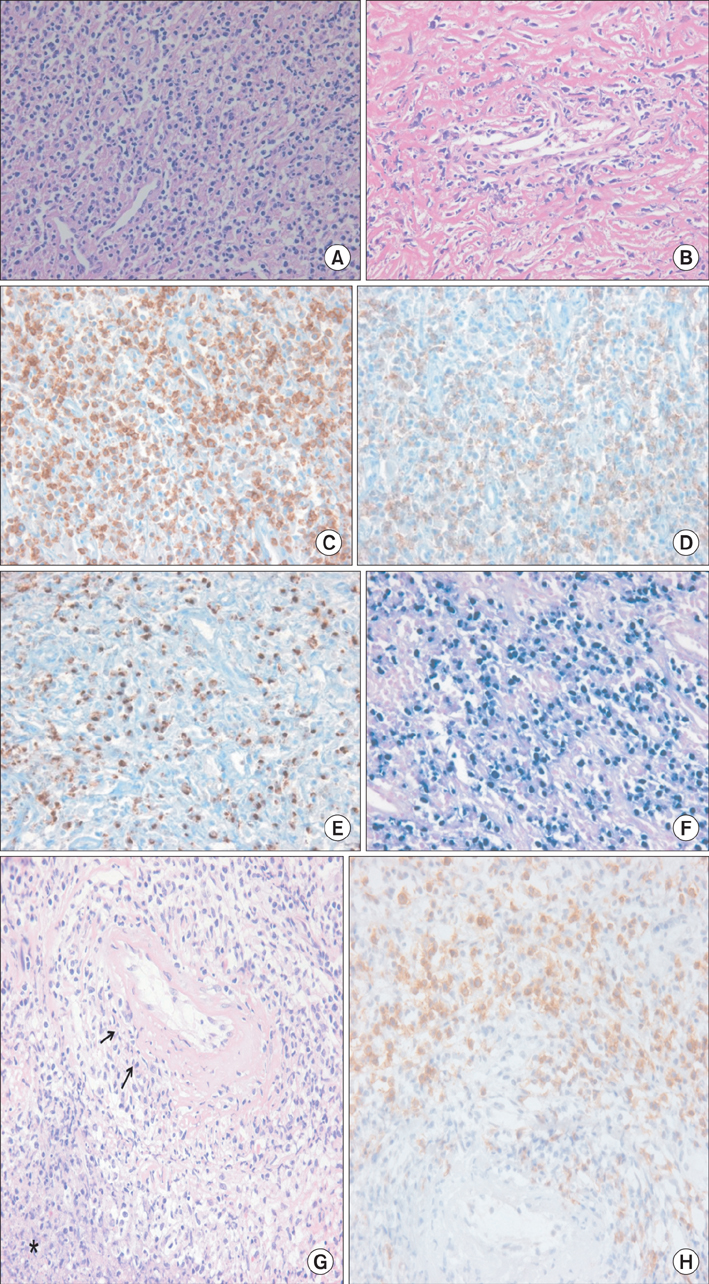
Single Pleural Relapse of a Nasal-Type Extranodal Natural Killer/T-Cell Lymphoma: A Case Report
- Affiliations
-
- 1Department of Internal Medicine, Chungbuk National University College of Medicine, Cheongju, Korea. drahnjy@chungbuk.ac.kr
- 2Department of Pathology, Chungbuk National University College of Medicine, Cheongju, Korea.
Abstract
- A nasal-type extranodal natural killer/T-cell lymphoma is considered an aggressive form of non-Hodgkin's lymphoma, with approximately half of all patients relapsing during the follow-up period, and most relapses occurring within the first 2 years of remission. Here we report an unusual case of a 42-year-old man who experienced recurrence in single pleura after 8 years of remission.
MeSH Terms
Figure
Reference
-
1. Lee J, Suh C, Park YH, Ko YH, Bang SM, Lee JH, et al. Extranodal natural killer T-cell lymphoma, nasal-type: a prognostic model from a retrospective multicenter study. J Clin Oncol. 2006; 24:612–618.2. Kim GE, Cho JH, Yang WI, Chung EJ, Suh CO, Park KR, et al. Angiocentric lymphoma of the head and neck: patterns of systemic failure after radiation treatment. J Clin Oncol. 2000; 18:54–63.3. Kwong YL. Natural killer-cell malignancies: diagnosis and treatment. Leukemia. 2005; 19:2186–2194.4. Au WY, Kim SJ, Yiu HH, Ngan RK, Loong F, Kim WS, et al. Clinicopathological features and outcome of late relapses of natural killer cell lymphomas 10-29 years after initial remission. Am J Hematol. 2010; 85:362–363.5. Jaffe ES. The 2008 WHO classification of lymphomas: implications for clinical practice and translational research. Hematology Am Soc Hematol Educ Program. 2009; 523–531.6. Kim J, Kim EY, Lee SK, Kim DI, Kim CH, Kim SH, et al. Extranodal nasal-type NK/T-cell lymphoma: computed tomography findings of head and neck involvement. Acta Radiol. 2010; 51:164–169.7. Berkman N, Breuer R, Kramer MR, Polliack A. Pulmonary involvement in lymphoma. Leuk Lymphoma. 1996; 20:229–237.8. Das DK. Serous effusions in malignant lymphomas: a review. Diagn Cytopathol. 2006; 34:335–347.9. Valdes L, Alvarez D, Valle JM, Pose A, San Jose E. The etiology of pleural effusions in an area with high incidence of tuberculosis. Chest. 1996; 109:158–162.10. Valdes L, Alvarez D, San Jose E, Penela P, Valle JM, Garcia-Pazos JM, et al. Tuberculous pleurisy: a study of 254 patients. Arch Intern Med. 1998; 158:2017–2021.11. Lee YC, Rogers JT, Rodriguez RM, Miller KD, Light RW. Adenosine deaminase levels in nontuberculous lymphocytic pleural effusions. Chest. 2001; 120:356–361.12. Wu CY, Hu HY, Pu CY, Huang N, Shen HC, Li CP, et al. Aerodigestive tract, lung and haematological cancers are risk factors for tuberculosis: an 8-year population-based study. Int J Tuberc Lung Dis. 2011; 15:125–130.13. Falagas ME, Kouranos VD, Athanassa Z, Kopterides P. Tuberculosis and malignancy. QJM. 2010; 103:461–487.14. Lanjewar DN, Lanjewar SD, Chavan G. Coexistent lymphoma with tuberculosis and Kaposi's sarcoma with tuberculosis occurring in lymph node in patients with AIDS: a report of two cases. Indian J Pathol Microbiol. 2010; 53:551–554.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Extranodal Natural Killer/T Cell Lymphoma Combined With Actinomycosis
- Extranodal NK/T-Cell Lymphoma, Nasal Type, Extranasal and Ulcerative Blister Variant, Case Report
- Metachronous extranodal natural killer/T-cell lymphoma of nasal type and primary testicular lymphoma
- Delayed Diagnosis Due to Septal Perforation in Patient with Extranodal Natural Killer/T-Cell Lymphoma, Nasal Type
- A Case of Nasal Type NK/T-cell Lymphoma