Tuberc Respir Dis.
2014 Jan;76(1):30-33.
The First Korean Case of Nontuberculous Mycobacterial Lung Disease Caused by Mycobacterium abscessus Subspecies bolletii in a Patient with Bronchiectasis
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. wjkoh@skku.edu
- 2Department of Laboratory Medicine and Genetics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Microbiology, Yonsei University College of Medicine, Seoul, Korea.
Abstract
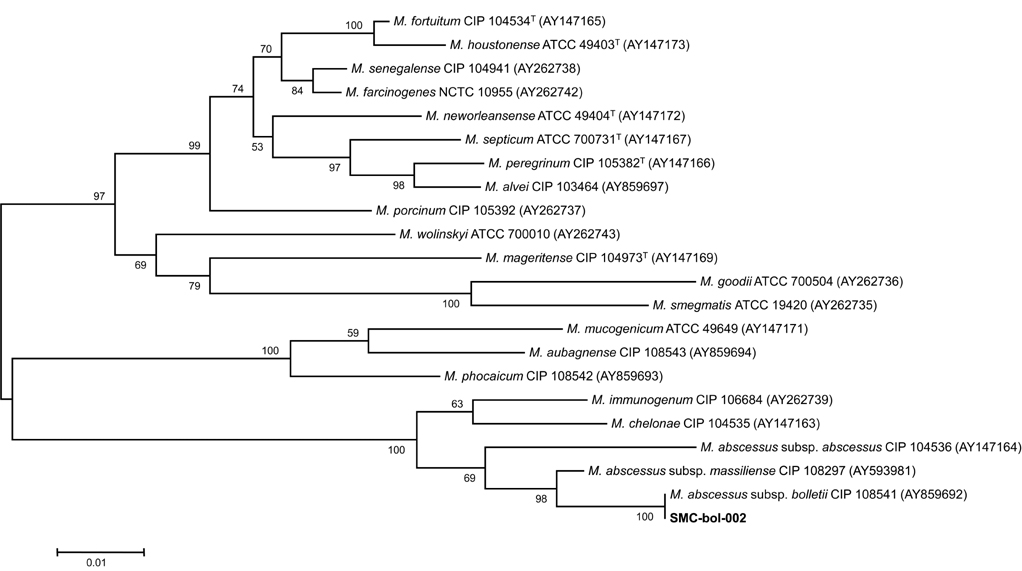
- We report the first Korean case of lung diseases caused by Mycobacterium abscessus subsp. bolletii in a previously healthy male, except for a previous history of pulmonary tuberculosis and bronchiectasis. All serial isolates are identified as M. abscessus subsp. bolletii by multi-locus sequence analysis based on the hsp65, rpoB, and 16S rRNA fragments. At the genetic level, the isolate has the erm(41) gene with a T28 sequevar, associated with clarithromycin resistance, and no rrl mutation. The isolate is resistant to clarithromycin. Although the symptoms and radiographic findings have improved after combination of antibiotics, the follow-up sputum cultures are persistently positive.
Keyword
MeSH Terms
Figure
Reference
-
1. Koh WJ, Kwon OJ, Jeon K, Kim TS, Lee KS, Park YK, et al. Clinical significance of nontuberculous mycobacteria isolated from respiratory specimens in Korea. Chest. 2006; 129:341–348.2. Macheras E, Roux AL, Bastian S, Leao SC, Palaci M, Sivadon-Tardy V, et al. Multilocus sequence analysis and rpoB sequencing of Mycobacterium abscessus (sensu lato) strains. J Clin Microbiol. 2011; 49:491–499.3. Koh WJ, Jeon K, Lee NY, Kim BJ, Kook YH, Lee SH, et al. Clinical significance of differentiation of Mycobacterium massiliense from Mycobacterium abscessus. Am J Respir Crit Care Med. 2011; 183:405–410.4. Koh WJ, Kwon OJ, Lee NY, Kook YH, Lee HK, Kim BJ. First case of disseminated Mycobacterium bolletii infection in a young adult patient. J Clin Microbiol. 2009; 47:3362–3366.5. Lee H, Park HJ, Cho SN, Bai GH, Kim SJ. Species identification of mycobacteria by PCR-restriction fragment length polymorphism of the rpoB gene. J Clin Microbiol. 2000; 38:2966–2971.6. Kim H, Kim SH, Shim TS, Kim MN, Bai GH, Park YG, et al. Differentiation of Mycobacterium species by analysis of the heat-shock protein 65 gene (hsp65). Int J Syst Evol Microbiol. 2005; 55(Pt 4):1649–1656.7. Clinical and Laboratory Standards Institute. Susceptibility testing of mycobacteria, nocardiae, and other aerobic actinomycetes: approved standard. 2nd ed. Wayne: CLSI;2011. Document no. M24-A2.8. Bastian S, Veziris N, Roux AL, Brossier F, Gaillard JL, Jarlier V, et al. Assessment of clarithromycin susceptibility in strains belonging to the Mycobacterium abscessus group by erm(41) and rrl sequencing. Antimicrob Agents Chemother. 2011; 55:775–781.9. Adekambi T, Drancourt M. Mycobacterium bolletii respiratory infections. Emerg Infect Dis. 2009; 15:302–305.10. van Ingen J, de Zwaan R, Dekhuijzen RP, Boeree MJ, van Soolingen D. Clinical relevance of Mycobacterium chelonae-abscessus group isolation in 95 patients. J Infect. 2009; 59:324–331.11. Moore M, Frerichs JB. An unusual acid-fast infection of the knee with subcutaneous, abscess-like lesions of the gluteal region; report of a case with a study of the organism, Mycobacterium abscessus, n. sp. J Invest Dermatol. 1953; 20:133–169.12. Adekambi T, Berger P, Raoult D, Drancourt M. rpoB gene sequence-based characterization of emerging non-tuberculous mycobacteria with descriptions of Mycobacterium bolletii sp. nov., Mycobacterium phocaicum sp. nov. and Mycobacterium aubagnense sp. nov. Int J Syst Evol Microbiol. 2006; 56(Pt 1):133–143.13. Bryant JM, Grogono DM, Greaves D, Foweraker J, Roddick I, Inns T, et al. Whole-genome sequencing to identify transmission of Mycobacterium abscessus between patients with cystic fibrosis: a retrospective cohort study. Lancet. 2013; 381:1551–1560.14. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007; 175:367–416.15. Jeon K, Kwon OJ, Lee NY, Kim BJ, Kook YH, Lee SH, et al. Antibiotic treatment of Mycobacterium abscessus lung disease: a retrospective analysis of 65 patients. Am J Respir Crit Care Med. 2009; 180:896–902.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Mycobacterium Abscessus Pulmonary Disease
- A Case of Mycobacterium abscessus Lung Disease in a Patient with Cystic Fibrosis
- A Case of Mycobacterium Abscessus Spondylitis
- Nontuberculous Mycobacterial Lung Disease Caused by Mycobacterium shinjukuense: The First Reported Case in Korea
- Nontuberculous Mycobacterial Lung Disease Caused by Mycobacterium terrae in a Patient with Bronchiectasis