Tuberc Respir Dis.
2013 Oct;75(4):161-164.
Intrapleural Corticosteroid Injection in Eosinophilic Pleural Effusion Associated with Undifferentiated Connective Tissue Disease
- Affiliations
-
- 1Department of Internal Medicine, Hallym University Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. masque@hallym.or.kr
Abstract
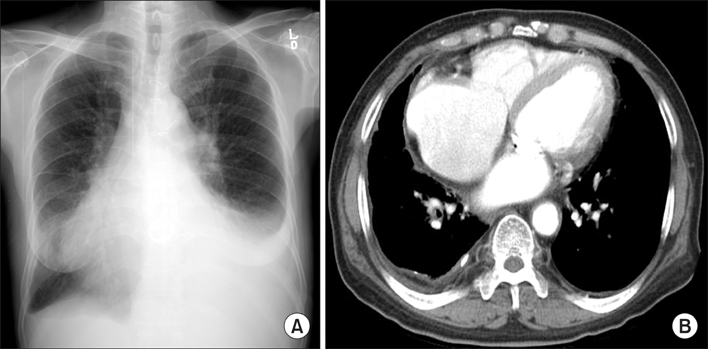
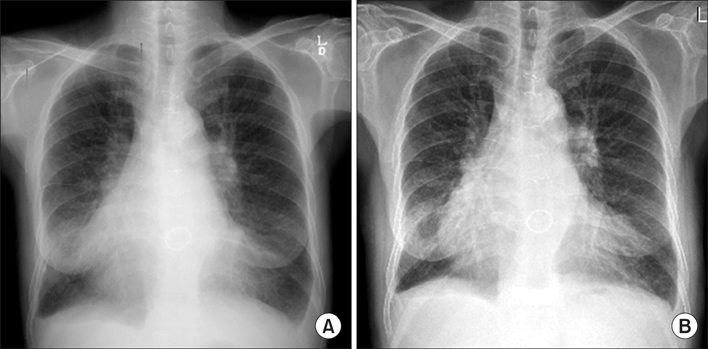
- Eosinophilic pleural effusion (EPE) is defined as a pleural effusion that contains at least 10% eosinophils. EPE occurs due to a variety of causes such as blood or air in the pleural space, infection, malignancy, or an autoimmune disease. Undifferentiated connective tissue disease (UCTD) associated with eosinophilic pleural effusion is a rare condition generally characterized by the presence of the signs and symptoms but not fulfilling the existing classification criteria. We report a case involving a 67-year-old man with UCTD and EPE, who has been successfully treated with a single intrapleural corticosteroid injection.
MeSH Terms
Figure
Reference
-
1. Kalomenidis I, Light RW. Eosinophilic pleural effusions. Curr Opin Pulm Med. 2003; 9:254–260.2. Ishiura Y, Fujimura M, Nakamura N, Jokaji H, Minami S, Matsuda T. Intrapleural corticosteroid injection therapy for post-traumatic eosinophilic pleural effusion. Respir Med. 1996; 90:501–503.3. Rubins JB, Rubins HB. Etiology and prognostic significance of eosinophilic pleural effusions: a prospective study. Chest. 1996; 110:1271–1274.4. Mosca M, Tani C, Carli L, Bombardieri S. Undifferentiated CTD: a wide spectrum of autoimmune diseases. Best Pract Res Clin Rheumatol. 2012; 26:73–77.5. Maeshima E, Nishimoto T, Yamashita M, Mune M, Yukawa S. Progressive systemic sclerosis-polymyositis overlap syndrome with eosinophilic pleural effusion. Rheumatol Int. 2003; 23:252–254.6. Ferreiro L, San Jose E, Gonzalez-Barcala FJ, Alvarez-Dobano JM, Golpe A, Gude F, et al. Eosinophilic pleural effusion: incidence, etiology and prognostic significance. Arch Bronconeumol. 2011; 47:504–509.7. Oba Y, Abu-Salah T. The prevalence and diagnostic significance of eosinophilic pleural effusions: a meta-analysis and systematic review. Respiration. 2012; 83:198–208.8. Krenke R, Nasilowski J, Korczynski P, Gorska K, Przybylowski T, Chazan R, et al. Incidence and aetiology of eosinophilic pleural effusion. Eur Respir J. 2009; 34:1111–1117.9. Samman YS, Wali SO, Abdelaal MA, Gangi MT, Krayem AB. Chronic eosinophilic pneumonia presenting with recurrent massive bilateral pleural effusion: case report. Chest. 2001; 119:968–970.10. Breuer GS, Deeb M, Fisher D, Nesher G. Therapeutic options for refractory massive pleural effusion in systemic lupus erythematosus: a case study and review of the literature. Semin Arthritis Rheum. 2005; 34:744–749.11. Felz MW, Haviland-Foley DJ. Eosinophilic pleural effusion due to dantrolene: resolution with steroid therapy. South Med J. 2001; 94:502–504.12. Cavazzana I, Franceschini F, Belfiore N, Quinzanini M, Caporali R, Calzavara-Pinton P, et al. Undifferentiated connective tissue disease with antibodies to Ro/SSa: clinical features and follow-up of 148 patients. Clin Exp Rheumatol. 2001; 19:403–409.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pleural Effusion in Connective Tissue Diseases
- Intrapleural Paclitaxel Chemotherapy in the Treatment of Breast Cancer-Related Metastatic Malignant Pleural Effusion
- Clinical Characteristics and Diagnostic Utility of Eosinophilic Pleural effusion
- Role of Intrapleural Pressure in the Positional Effect on Gas Exchange in Unilateral Pleural Effusion
- Eosinophilic Endomyocarditis Combined With Pericardial and Pleural Effusion