Tuberc Respir Dis.
2012 Aug;73(2):115-121.
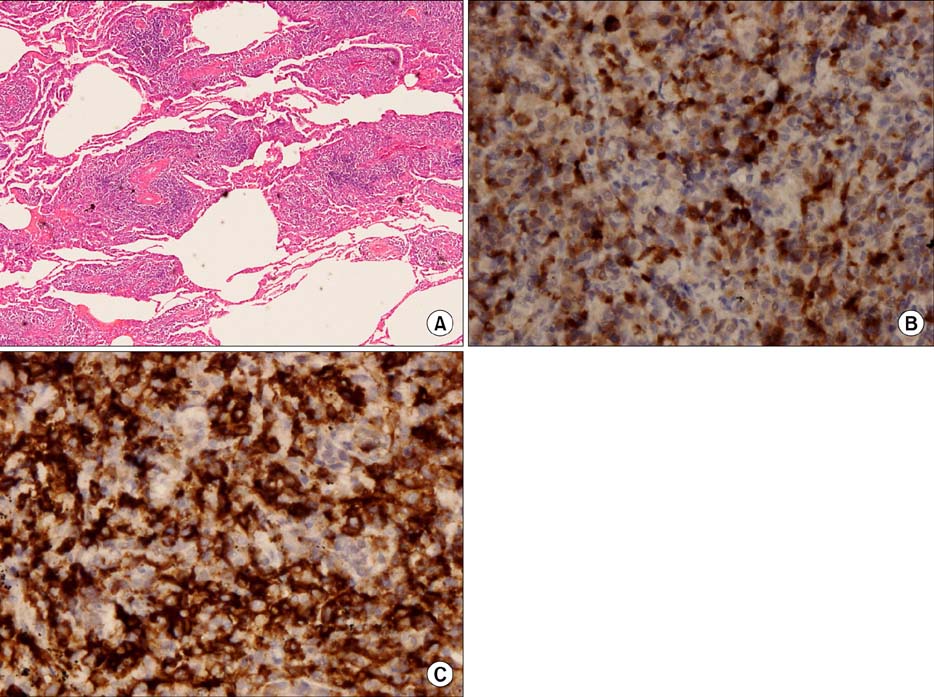
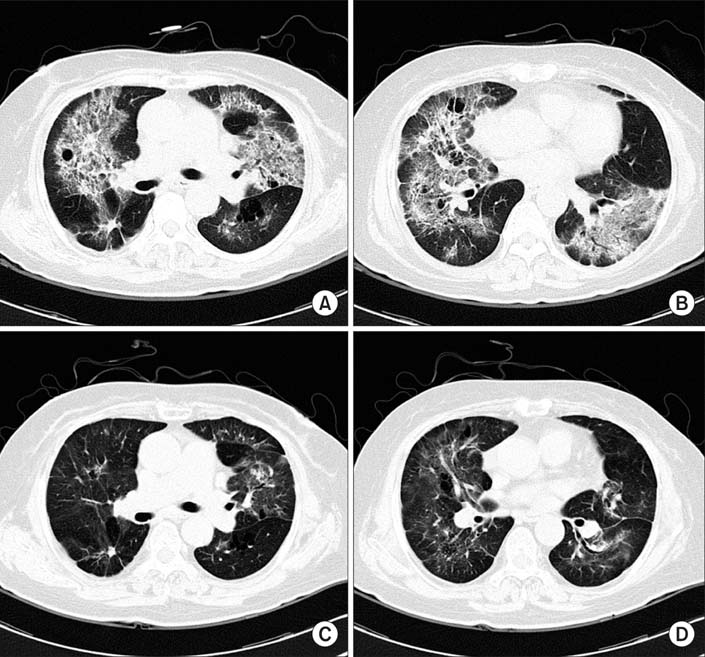
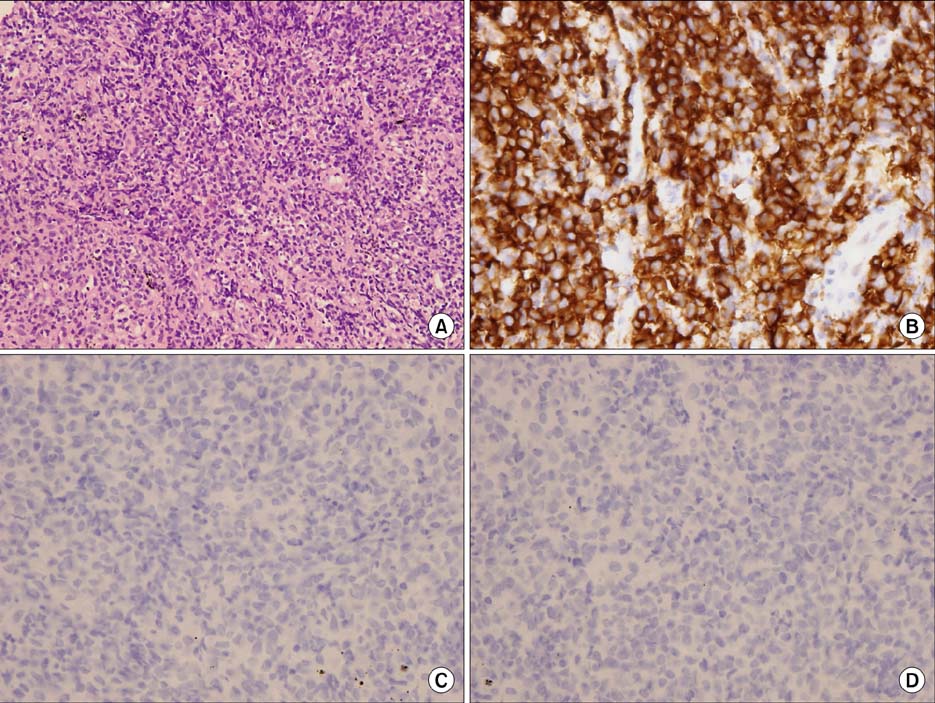
A Case of Pulmonary MALT Lymphoma Arising from Lymphocytic Interstitial Pneumonitis
- Affiliations
-
- 1Department of Internal Medicine, Bucheon St. Mary's Hospital, The Catholic University of Korea School of Medicine, Bucheon, Korea. kyh30med@catholic.ac.kr
- 2Department of Radiology, Bucheon St. Mary's Hospital, The Catholic University of Korea School of Medicine, Bucheon, Korea.
- 3Department of Pathology, Bucheon St. Mary's Hospital, The Catholic University of Korea School of Medicine, Bucheon, Korea.
- 4Department of Internal Medicine, Catholic Medical Center, The Catholic University of Korea School of Medicine, Seoul, Korea.
Abstract
- Pulmonary mucosa-associated lymphoid tissue-derived (MALT) lymphoma is a rare disease. This disorder is considered to be a model of antigen-driven lymphoma, which is driven either by autoantigens or by chronic inflammatory conditions. Low-grade B-cell MALT lymphoma may develop from a nonneoplastic pulmonary lymphoproliferative disorder, such as lymphocytic interstitial pneumonitis (LIP). A recent estimate predicts that less than 5% of LIP patients acquire malignant, low-grade, B-cell lymphoma. In Korea, there has been no previous report of malignant low-grade, B-cell lymphoma, acquired from LIP. Here, we present the case of a patient with LIP that developed into pulmonary MALT lymphoma, six years after diagnosis.
MeSH Terms
Figure
Reference
-
1. Cadranel J, Wislez M, Antoine M. Primary pulmonary lymphoma. Eur Respir J. 2002. 20:750–762.2. Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, Cleary ML, et al. A revised European-American classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group. Blood. 1994. 84:1361–1392.3. Isaacson P, Wright DH. Extranodal malignant lymphoma arising from mucosa-associated lymphoid tissue. Cancer. 1984. 53:2515–2524.4. Sminia T, van der Brugge-Gamelkoorn GJ, Jeurissen SH. Structure and function of bronchus-associated lymphoid tissue (BALT). Crit Rev Immunol. 1989. 9:119–150.5. Royer B, Cazals-Hatem D, Sibilia J, Agbalika F, Cayuela JM, Soussi T, et al. Lymphomas in patients with Sjogren's syndrome are marginal zone B-cell neoplasms, arise in diverse extranodal and nodal sites, and are not associated with viruses. Blood. 1997. 90:766–775.6. Suarez F, Lortholary O, Hermine O, Lecuit M. Infection-associated lymphomas derived from marginal zone B cells: a model of antigen-driven lymphoproliferation. Blood. 2006. 107:3034–3044.7. Swigris JJ, Berry GJ, Raffin TA, Kuschner WG. Lymphoid interstitial pneumonia: a narrative review. Chest. 2002. 122:2150–2164.8. Teruya-Feldstein J, Kingma DW, Weiss A, Sorbara L, Burd PR, Raffeld M, et al. Chemokine gene expression and clonal analysis of B cells in tissues involved by lymphoid interstitial pneumonitis from HIV-infected pediatric patients. Mod Pathol. 2001. 14:929–936.9. Do KH, Lee JS, Seo JB, Song JW, Chung MJ, Heo JN, et al. Pulmonary parenchymal involvement of low-grade lymphoproliferative disorders. J Comput Assist Tomogr. 2005. 29:825–830.10. Guinee DG Jr. Update on nonneoplastic pulmonary lymphoproliferative disorders and related entities. Arch Pathol Lab Med. 2010. 134:691–701.11. Nicholson AG, Wotherspoon AC, Diss TC, Hansell DM, Du Bois R, Sheppard MN, et al. Reactive pulmonary lymphoid disorders. Histopathology. 1995. 26:405–412.12. Bae YA, Lee KS, Han J, Ko YH, Kim BT, Chung MJ, et al. Marginal zone B-cell lymphoma of bronchus-associated lymphoid tissue: imaging findings in 21 patients. Chest. 2008. 133:433–440.13. Borie R, Wislez M, Thabut G, Antoine M, Rabbat A, Couderc LJ, et al. Clinical characteristics and prognostic factors of pulmonary MALT lymphoma. Eur Respir J. 2009. 34:1408–1416.14. Zucca E, Dreyling M. ESMO Guidelines Working Group. Gastric marginal zone lymphoma of MALT type: ESMO clinical recommendations for diagnosis, treatment and follow-up. Ann Oncol. 2008. 19:Suppl 2. ii70–ii71.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lymphocytic Gastritis in Helicobacter pylori-positive Gastric MALT Lymphoma: Report of Two Cases
- A case report of the Pulmonary Malignant Lymphomaof the mucosa-associated lymphoid tissue(MALT)
- A Case of Gastroduodenal Mucosa-associated Lymphoid Tissue Lymphoma Regression after Eradication of Helicobacter pylori
- A Case of Primary Pulmonary Extranodal Marginal Zone B-Cell Lymphoma of the MALT Type
- Lymphocytic Interstitial Pneumonitis Associated with Epstein-Barr virus in Systemic Lupus Erythematosus and Sjgren's Syndrome: Complete remission with corticosteroid and cyclophosphamide