Tuberc Respir Dis.
2012 Feb;72(2):223-227.
A Case of Welder's Lung Disease and Concurred Non-Tuberculotic Mycobacterial Infection Confirmed with Thoracoscopic Lung Biopsy
- Affiliations
-
- 1Department of Internal Medicine, Bucheon St. Mary's Hospital, The Catholic University of Korea College of Medicine, Bucheon, Korea. kyh30med@catholic.ac.kr
Abstract
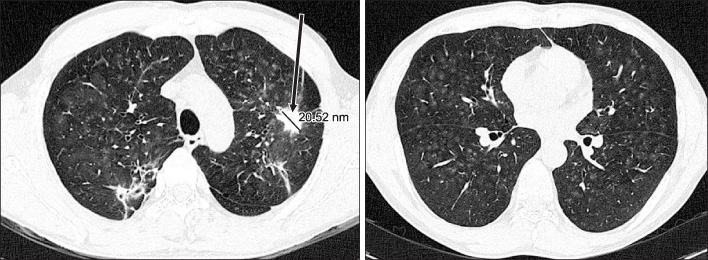
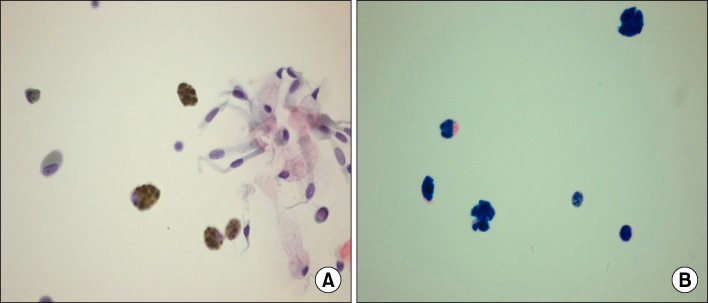
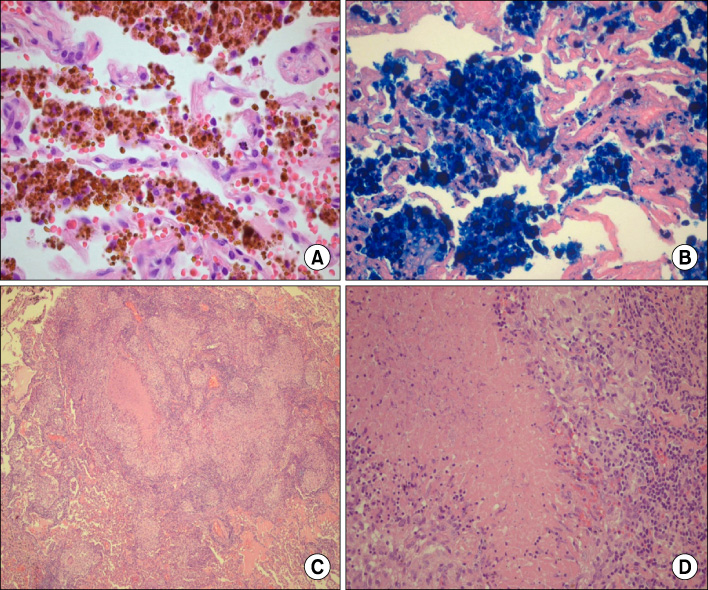
- Pulmonary siderosis, or Welder's lung disease is an occupational lung disease caused by iron-inhalation. Diagnosis of pulmonary siderosis is based on occupational history of the patient, radiologic findings, and pathologic findings of iron-laden macrophages within lung tissue or broncho-alveolar lavage fluid. We observed a case of a 43 years-old welder diagnosed with pulmonary siderosis via thoracoscopic lung biopsy. Sputum culture along with pathology also identified a non-tuberculotic mycobacterial infection with a sputum culture and the pathologic findings. The patient was treated with anti-tubercular medication and cessation of iron-exposure. And his condition improved within a few months.
Keyword
MeSH Terms
Figure
Reference
-
1. Mason RJ, Martin T, King T Jr, Schraufnagel D, Murray JF. Murray and Nadel's Textbook of Respiratory Medicine. 2010. 5th ed. Philadelphia: Saunders.2. Guidotti TL, Abraham JL, DeNee PB, Smith JR. Arc welders' pneumoconiosis: application of advanced scanning electron microscopy. Arch Environ Health. 1978. 33:117–124.3. Flors L, Domingo ML, Leiva-Salinas C, Mazón M, Roselló-Sastre E, Vilar J. Uncommon occupational lung diseases: high-resolution CT findings. AJR Am J Roentgenol. 2010. 194:W20–W26.4. Han D, Goo JM, Im JG, Lee KS, Park DM, Park SH. Thin-section CT findings of arc-welders' pneumoconiosis. Korean J Radiol. 2000. 1:79–83.5. Chong S, Lee KS, Chung MJ, Han J, Kwon OJ, Kim TS. Pneumoconiosis: comparison of imaging and pathologic findings. Radiographics. 2006. 26:59–77.6. Yamada G, Igarashi T, Sonoda H, Morita S, Suzuki K, Yoshida Y, et al. Use of bronchopulmonary lavage for eliminating inhaled fume particles from a patient with arc welder's lung. Intern Med. 1998. 37:962–964.7. Marras TK, Daley CL. Epidemiology of human pulmonary infection with nontuberculous mycobacteria. Clin Chest Med. 2002. 23:553–567.8. Sonnenberg P, Murray J, Glynn JR, Thomas RG, Godfrey-Faussett P, Shearer S. Risk factors for pulmonary disease due to culture-positive M. tuberculosis or nontuberculous mycobacteria in South African gold miners. Eur Respir J. 2000. 15:291–296.9. Corbett EL, Churchyard GJ, Clayton T, Herselman P, Williams B, Hayes R, et al. Risk factors for pulmonary mycobacterial disease in South African gold miners. A case-control study. Am J Respir Crit Care Med. 1999. 159:94–99.10. Koh WJ, Kwon OJ, Lee KS. Diagnosis and treatment of nontuberculous mycobacterial pulmonary diseases: a Korean perspective. J Korean Med Sci. 2005. 20:913–915.11. Koh WJ, Kwon OJ, Jeon K, Kim TS, Lee KS, Park YK, et al. Clinical significance of nontuberculous mycobacteria isolated from respiratory specimens in Korea. Chest. 2006. 129:341–348.12. Ryoo SW, Shin S, Shim MS, Park YS, Lew WJ, Park SN, et al. Spread of nontuberculous mycobacteria from 1993 to 2006 in Koreans. J Clin Lab Anal. 2008. 22:415–420.13. American Thoracic Society. Diagnosis and treatment of disease caused by nontuberculous mycobacteria. Am J Respir Crit Care Med. 1997. 156:S1–S25.14. Tsukamura M, Kita N, Shimoide H, Arakawa H, Kuze A. Studies on the epidemiology of nontuberculous mycobacteriosis in Japan. Am Rev Respir Dis. 1988. 137:1280–1284.15. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007. 175:367–416.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thoracoscopic Lung Biopsy for Diffuse Interstitial Lung Disease
- Surgical Lung Biopsy for Diffuse Infiltrative Lung Disease
- National Survey of Open Lung Biopsy and Thoracoscopic Lung Biopsy in Korea
- The use of lung ultrasonography to confirm lung isolation in an infant who underwent emergent video-assisted thoracoscopic surgery: a case report
- A Comparison of Thoracoscopic and Open Lung Biopsy for the Diffuse Infiltrative Lung Disease