Tuberc Respir Dis.
2011 Dec;71(6):454-458.
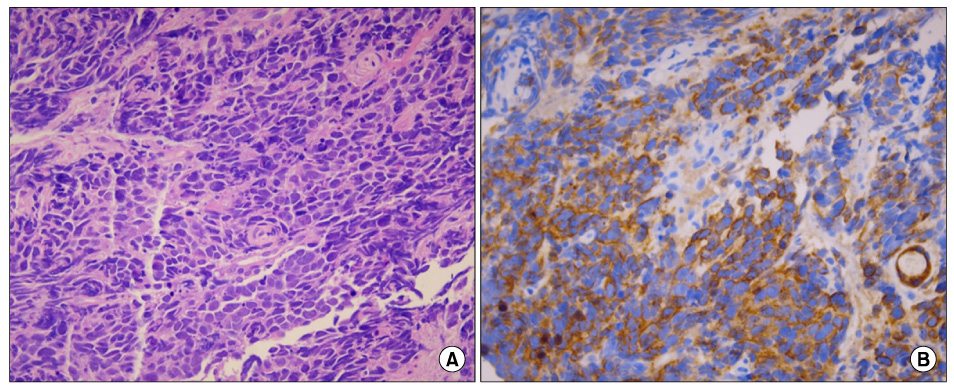
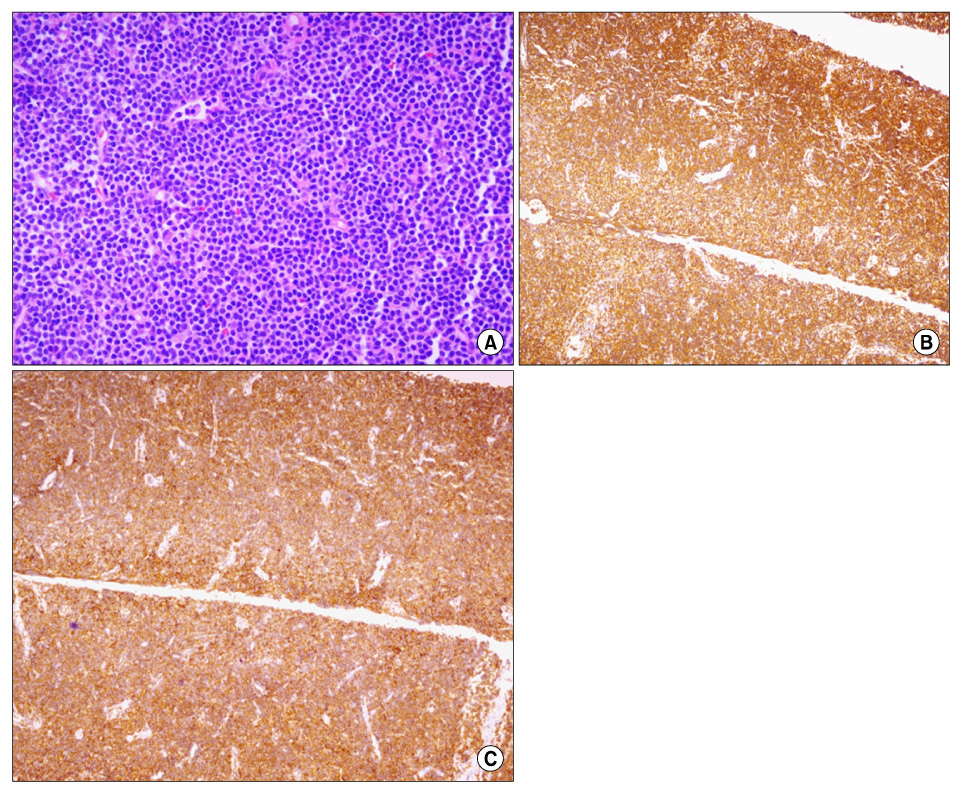
A Case of Small Cell Lung Cancer Coexisting with Chronic Lymphocytic Leukemia
- Affiliations
-
- 1Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea. jwsohn@hanyang.ac.kr
- 2Department of Pathology, Hanyang University College of Medicine, Seoul, Korea.
Abstract
- Chronic lymphocytic leukemia (CLL) is the most common type of leukemia occurring in Western nations. In CLL it is well known that the risk of a secondary malignancy is higher than in the normal population. But in Korea, CLL is a rare type of leukemia, so there have been only a few reported cases with a secondary malignancy. CLL is characterized by progressive defects in both cell-mediated and humoral immunity. It is known that defects in the immune system of patients with CLL contribute to the development of a secondary malignancy. We experienced a case of a 71-year-old man who suffered from a chronic cough and was diagnosed with small cell lung cancer coexisting with CLL. Until this case, there was no reported case in Korea of small cell lung cancer coexisting with CLL. We now report a case of small cell lung cancer coexisting with CLL and present a literature review.
MeSH Terms
Figure
Reference
-
1. Dasanu CA, Alexandrescu DT. Risk for second nonlymphoid neoplasms in chronic lymphocytic leukemia. MedGenMed. 2007. 9:35.2. Nam SH, Kwon JM, Mun YC, Lee KE, Lee SY, Chung WS, et al. A case of coexistent chronic lymphocytic leukemia and multiple myeloma. Korean J Hematol. 2005. 40:41–44.3. Lee JL, Kang HJ, Oh HA, Lee G, Lee KH, Hyun MS, et al. A case of pure red cell aplasia associated with B-cell chronic lymphocytic leukemia. Korean J Hematol. 2002. 37:60–64.4. Lee SA, Kim YJ, Lim KC, Jung CI, Jung SY, Shin MK, et al. A case of adenocarcinoma of the lung in patient with chronic lymphpcoytic leukemia. J Korean Cancer Assoc. 1998. 30:613–619.5. Kim DK, Park JC, Choi WH, Kim JH, Han CW. A case of chronic lymphocytic leukemia coexisting with basal cell carcinoma and lung cancer. Korean J Hematol. 2009. 44:133–138.6. Parekh K, Rusch V, Kris M. The clinical course of lung carcinoma in patients with chronic lymphocytic leukemia. Cancer. 1999. 86:1720–1723.7. Schöllkopf C, Rosendahl D, Rostgaard K, Pipper C, Hjalgrim H. Risk of second cancer after chronic lymphocytic leukemia. Int J Cancer. 2007. 121:151–156.8. Ravandi F, O'Brien S. Immune defects in patients with chronic lymphocytic leukemia. Cancer Immunol Immunother. 2006. 55:197–209.9. Billroth T, von Winiwarter A. Die allgemeine chirurgische pathologie und therapie in 51 vorlesungen. Ein handbuch für studierende und aerzte, 14 Auflage. 1889. Berlin, Germany: G. Reimer.10. Warren S, Gates O. Multiple primary malignant tumours: a survey of the literature and statistical study. Am J Cancer. 1932. 162:1358–1414.11. Moertel CG. Multiple primary malignant neoplasms: historical perspectives. Cancer. 1977. 40:4 Suppl. 1786–1792.12. Fried BM. Primary multiple cancers. AMA Arch Surg. 1958. 77:730–741.13. Kiriu H, Yokozaki H, Yasui W, Ito K, Tahara E. Microsatellite instability associated with primary head and neck cancers and secondary esophageal cancers. Jpn J Clin Oncol. 1998. 28:733–739.14. Sigurdson AJ, Jones IM. Second cancers after radiotherapy: any evidence for radiation-induced genomic instability? Oncogene. 2003. 22:7018–7027.15. Hayashi T, Arai M, Ueno M, Kinoshita H, Tada Y, Koizumi K, et al. Frequency of immunohistochemical loss of mismatch repair protein in double primary cancers of the colorectum and stomach in Japan. Dis Colon Rectum. 2006. 49:10 Suppl. S23–S29.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Chronic Lymphocytic Leukemia Coexisting with Basal Cell Carcinoma and Lung Cancer
- A case of B cell chronic lymphocytic leukemia involving thyroidgland
- A Case of Leukemia Cutis Associated with B-cell Chronic Lymphocytic Leukemia
- First Case of Transformation of Immunoglobulin Heavy Chain Variable-Mutated Chronic Lymphocytic Leukemia Into Chronic Myeloid Leukemia
- Large cell lymphoma as initial presentation of undetected chronic lymphocytic leukemia