Tuberc Respir Dis.
2009 Jun;66(6):431-436.
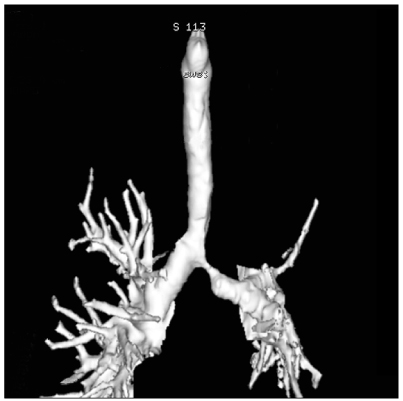
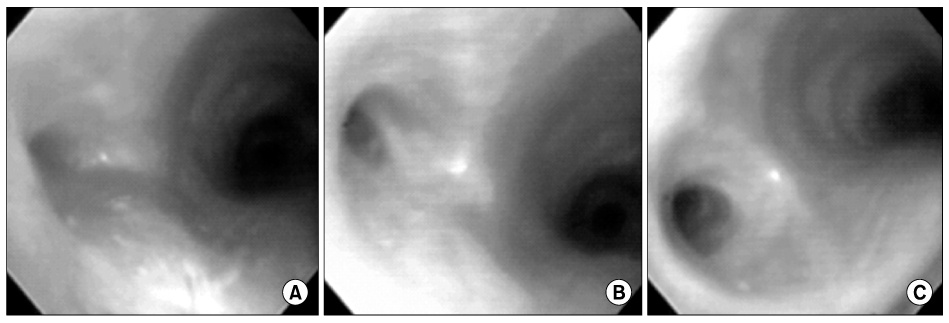
The Role of Ballooning in Patients with Post-tuberculosis Bronchial Stenosis
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. hjkim@smc.samsung.co.kr
- 2Division of Pulmonary and Critical Care Medicine, Department of Medicine, Masan Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea.
Abstract
-
BACKGROUND: In order to access the role of ballooning in patients with post-tuberculosis bronchial stenosis (PTBS), medical records of patients who underwent the procedure were reviewed.
METHODS
Twenty-nine PTBS patients underwent balloon dilatation between May 1999 and November 2000 at Samsung Medical Center. The median age was 28 (range 16~62 year) and most patients were female (n=27, 93%). The mean number of ballooning procedures was 2.4 (range 1~8) and the interval between ballooning procedures was 76.2+/-69.7 days.
RESULTS
In general, the FEV1 was improved after ballooning (from 66.2.+/-11.9% predicted to 73.5+/-13.0% predicted, p=0.0004). Among 29 patients who underwent ballooning, a clinically successful outcome was observed in 16 patients (55%). Comparison between the successful and unsuccessful groups showed that favorable factors for a successful outcome were a higher pre-ballooning FEV1 (71.1+/-8.1 vs. 60.2+/-13.3% predicted), higher post-ballooning FEV1 (89.2+/-7.8 vs. 63.4+/-9.2% predicted) and absence of left upper lobe collapse. The clinical outcome was unsuccessful in all eight patients with a pre-ballooning FEV1 < or =57% of predicted or with complete left upper lobe collapse.
CONCLUSION
In conclusion, ballooning appears to be helpful in patients with PTBS, especially when the pre-ballooning FEV1 >57% of predicted and there is no complete left upper lobe lung collapse.
Keyword
MeSH Terms
Figure
Reference
-
1. Chung HS, Lee JH. Bronchoscopic assessment of the evolution of endobronchial tuberculosis. Chest. 2000. 117:385–392.2. Kim YH, Kim HT, Lee KS, Uh ST, Cung YT, Park CS. Serial fiberoptic bronchoscopic observations of endobronchial tuberculosis before and early after antituberculosis chemotherapy. Chest. 1993. 103:673–677.3. Kurasawa T, Kuze F, Kawai M, Amitani R, Murayama T, Tanaka E, et al. Diagnosis and management of endobronchial tuberculosis. Intern Med. 1992. 31:593–598.4. Kim Y, Lee KS, Yoon JH, Chung MP, Kim H, Kwon OJ, et al. Tuberculosis of the trachea and main bronchi: CT findings in 17 patients. AJR Am J Roentgenol. 1997. 168:1051–1056.5. Shim YS. Endobronchial tuberculosis. Respirology. 1996. 1:95–106.6. Albert RK, Petty TL. Endobronchial tuberculosis progressing to bronchial stenosis: fiberoptic bronchoscopic manifestations. Chest. 1976. 70:537–539.7. Smith JL, Elliott CG, Schmidt CD, Flinner RL. Bronchial stenosis: a complication of healed endobronchial tuberculosis. West J Med. 1986. 144:361–362.8. Cohen MD, Weber TR, Rao CC. Balloon dilatation of tracheal and bronchial stenosis. AJR Am J Roentgenol. 1984. 142:477–478.9. Fowler CL, Aaland MO, Harris FL. Dilatation of bronchial stenosis with Gruentzig balloon. J Thorac Cardiovasc Surg. 1987. 93:308–309.10. Kim H. Stenting therapy for stenosing airway disease. Respirology. 1998. 3:221–228.11. Lee KH, Ko GY, Song HY, Shim TS, Kim WS. Benign tracheobronchial stenoses: long-term clinical experience with balloon dilation. J Vasc Interv Radiol. 2002. 13:909–914.12. Lee KW, Im JG, Han JK, Kim TK, Park JH, Yeon KM. Tuberculous stenosis of the left main bronchus: results of treatment with balloons and metallic stents. J Vasc Interv Radiol. 1999. 10:352–358.13. Nakamura K, Terada N, Ohi M, Matsushita T, Kato N, Nakagawa T. Tuberculous bronchial stenosis: treatment with balloon bronchoplasty. AJR Am J Roentgenol. 1991. 157:1187–1188.14. Carlin BW, Harrell JH 2nd, Moser KM. The treatment of endobronchial stenosis using balloon catheter dilatation. Chest. 1988. 93:1148–1151.15. Chhajed PN, Malouf MA, Glanville AR. Bronchoscopic dilatation in the management of benign (non-transplant) tracheobronchial stenosis. Intern Med J. 2001. 31:512–516.16. Han JK, Im JG, Park JH, Han MC, Kim YW, Shim YS. Bronchial stenosis due to endobronchial tuberculosis: successful treatment with self-expanding metallic stent. AJR Am J Roentgenol. 1992. 159:971–972.17. Kim W, Lee YC, Rhee YK. Obstruction after self-expanding metallic stents in tuberculous bronchial stenosis. Korean J Intern Med. 1995. 10:64–67.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Corticosteroid on the Treatment of Endobronchial Tuberculosis
- Balloon dilatation of bronchial stenosis in adult
- A Case of Bronchial Varices in a Patient with Severe Mitral Stenosis
- Flexible Bronchoscopic Observation of Bronchial Tuberculosis
- Left Lower Lobectomy with Bronchoplasty for Treatment of Bronchial Stricture