Tuberc Respir Dis.
2009 Jan;66(1):47-51.
A Case of Hepatopulmonary Syndrome in a Patient with Child-Pugh Class A Liver Cirrhosis
- Affiliations
-
- 1Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea.
- 2Department of Internal Medicine and Sejong Medical Research Institute, Sejong General Hospital, Bucheon, Korea. masque@sejongh.co.kr
Abstract
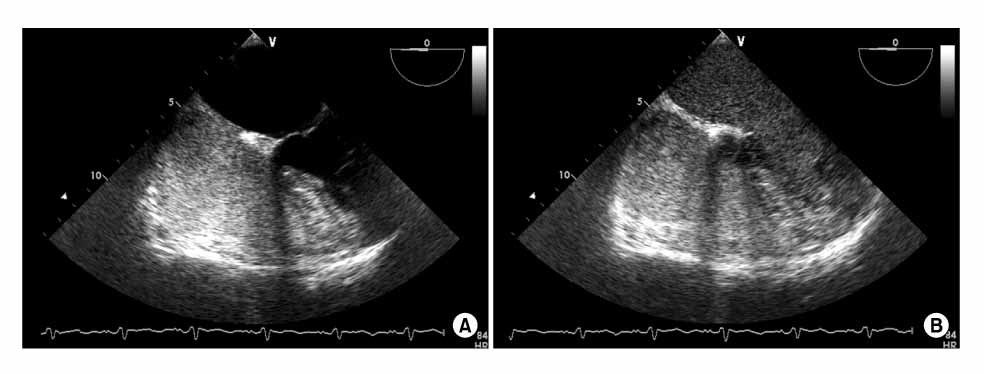
- Hepatopulmonary syndrome (HPS) is characterized by a defect in arterial oxygenation that's induced by pulmonary vascular dilatation in the setting of liver disease. Some studies have shown the relationship between the presence of the HPS and the severity of liver disease, but there are only rare cases of HPS inpatient with Child-Pugh class A liver cirrhosis. We report here on a case of a 58 years-old male who suffered from progressive dyspnea for the previous few years. He was diagnosed with alcoholic liver cirrhosis 5 years previously. There was no significant abnormality on the chest radiograph and transthoracic echocardiography, but the arterial blood gas analysis revealed severe hypoxemia. Contrast-enhanced transesophageal echocardiograpy with agitated saline demonstrated a delayed appearance of microbubbles in the left cardiac chambers. Thus, he was finally diagnosed with HPS. This case suggests that we should consider HPS when a patient with compensated liver cirrhosis has unexplained dyspnea.
MeSH Terms
Figure
Reference
-
1. Hoeper MM, Krowka MJ, Strassburg CP. Portopulmonary hypertension and hepatopulmonary syndrome. Lancet. 2004. 363:1461–1468.2. Rodríguez-Roisin R, Krowka MJ. Hepatopulmonary syndrome: a liver-induced lung vascular disorder. N Engl J Med. 2008. 358:2378–2387.3. Abrams GA, Jaffe CC, Hoffer PB, Binder HJ, Fallon MB. Diagnostic utility of contrast echocardiography and lung perfusion scan in patients with hepatopulmonary syndrome. Gastroenterology. 1995. 109:1283–1288.4. Schenk P, Fuhrmann V, Madl C, Funk G, Lehr S, Kandel O, et al. Hepatopulmonary syndrome: prevalence and predictive value of various cut offs for arterial oxygenation and their clinical consequences. Gut. 2002. 51:853–859.5. Lee JM, Choi MS, Lee SC, Park SW, Bae MH, Lee JH, et al. Prevalence and risk factors of significant intrapulmonary shunt in cirrhotic patients awaiting liver transplantation. Taehan Kan Hakhoe Chi. 2002. 8:271–276.6. Lee JH, Lee DH, Zo JH, Kim TH, Lee KL, Chung HS, et al. Hepatopulmonary syndrome in poorly compensated postnecrotic liver cirrhosis by hepatitis B virus in Korea. Korean J Intern Med. 2001. 16:56–61.7. Kim JW, Kang KW, Hwang JH, Jang IG, Park HK, Park CW, et al. A case of hepatopulmonary syndrome. Korean J Med. 1997. 53:596–604.8. Park DY, Cha SD, Kim J, Kim BG, Yoo CG, Sohn DW, et al. A case of hepatopulmonary syndrome due to intrapulmonary shunting in a patient with liver cirrhosis. Korean J Med. 1997. 53:272–276.9. Ryu DS, Jung BH, Jung SS, Kim HD, Yoo CH, Kang KH, et al. A case of hepatopulmonary syndrome with cyanosis. Tuberc Respir Dis. 1999. 46:420–425.10. Oh HT, Lee MY, Song IH, Park SG. A case of hepatopulmonary syndrome diagnosed by 99mTc-MAA perfusion lung scan. Korean J Nucl Med. 2002. 36:203–208.11. Rodriguez-Roisin R, Krowka MJ, Herve P, Fallon MB. Pulmonary-hepatic vascular disorders (PHD). Eur Respir J. 2004. 24:861–880.12. Kim BJ, Lee SC, Park SW, Choi MS, Koh KC, Paik SW, et al. Characteristics and prevalence of intrapulmonary shunt detected by contrast echocardiography with harmonic imaging in liver transplant candidates. Am J Cardiol. 2004. 94:525–528.13. Krowka MJ, Wiseman GA, Burnett OL, Spivey JR, Therneau T, Porayko MK, et al. Hepatopulmonary syndrome: a prospective study of relationships between severity of liver disease, PaO(2) response to 100% oxygen, and brain uptake after (99m)Tc MAA lung scanning. Chest. 2000. 118:615–624.14. Swanson KL, Wiesner RH, Krowka MJ. Natural history of hepatopulmonary syndrome: Impact of liver transplantation. Hepatology. 2005. 41:1122–1129.15. Nunes H, Lebrec D, Mazmanian M, Capron F, Heller J, Tazi KA, et al. Role of nitric oxide in hepatopulmonary syndrome in cirrhotic rats. Am J Respir Crit Care Med. 2001. 164:879–885.16. Cremona G, Higenbottam TW, Mayoral V, Alexander G, Demoncheaux E, Borland C, et al. Elevated exhaled nitric oxide in patients with hepatopulmonary syndrome. Eur Respir J. 1995. 8:1883–1885.17. Tumgor G, Berdeli A, Arikan C, Levent E, Aydogdu S. Mcp-1, eNOS, tPA and PAI-1 gene polymorphism and correlation of genotypes and phenotypes in hepatopulmonary syndrome. Dig Dis Sci. 2008. 53:1345–1351.18. Schenk P, Madl C, Rezaie-Majd S, Lehr S, Müller C. Methylene blue improves the hepatopulmonary syndrome. Ann Intern Med. 2000. 133:701–706.19. Gómez FP, Barberá JA, Roca J, Burgos F, Gistau C, Rodríguez-Roisin R. Effects of nebulized N(G)-nitro-L-arginine methyl ester in patients with hepatopulmonary syndrome. Hepatology. 2006. 43:1084–1091.20. Brussino L, Bucca C, Morello M, Scappaticci E, Mauro M, Rolla G. Effect on dyspnoea and hypoxaemia of inhaled NG-nitro-L-arginine methyl ester in hepatopulmonary syndrome. Lancet. 2003. 362:43–44.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence and Risk Factors of Significant Intrapulmonary Shunt in Cirrhotic patients awaiting liver transplantation
- Hepatopulmonary Syndrome with Finger Clubbing
- A Case of Hepatopulmonary Syndrome Due to Intrapulmonary Shunting in a Patient with Liver Cirrhosis
- Child-Pugh Score Is an Independent Risk Factor for Immediate Bleeding after Colonoscopic Polypectomy in Liver Cirrhosis
- A case of hepatopulmonary syndrome in a child with fatty liver disease secondary to hypopituitarism after craniopharyngioma resection