Tuberc Respir Dis.
2006 Aug;61(2):129-136.
Effect of the Changing the Lower Limits of Normal and the Interpretative Strategies for Lung Function Tests
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine and the Clinical Research Center for Chronic Obstructive Airway Diseases, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. ymoh55@amc.seoul.kr
Abstract
-
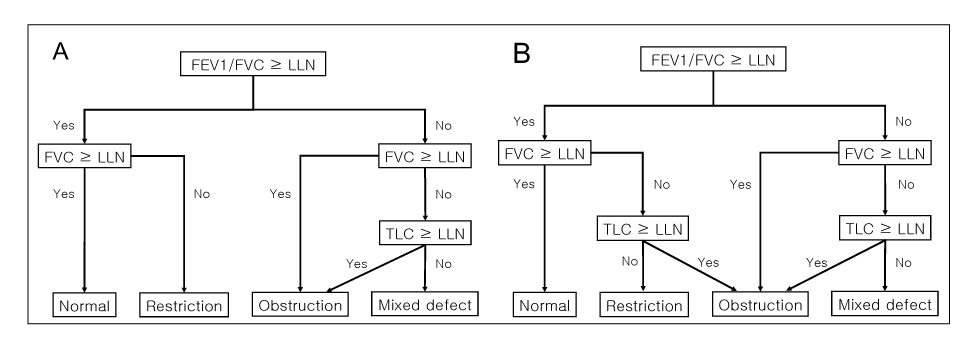
BACKGROUND: To interpret lung function tests, it is necessary to determine the lower limits of normal (LLN) and to derive a consensus on the interpretative algorithm. '0.7 of LLN for the FEV1/FVC' was suggested by the COPD International Guideline (GOLD) for defining obstructive disease. A consensus on a new interpretative algorithm was recently achieved by ATS/ERS in 2005. We evaluated the accuracy of '0.7 of LLN for the FEV1/FVC' for diagnosing obstructive diseases, and we also determined the effect of the new algorithm on diagnosing ventilatory defects.
METHODS
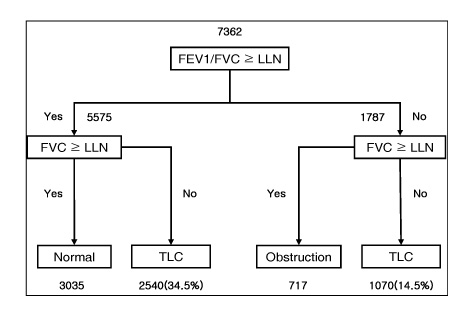
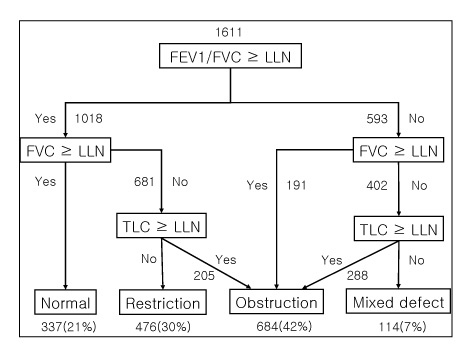
We obtained the age, gender, height, weight, FEV1, FVC, and FEV1/FVC from 7362 subjects who underwent spirometry in 2005 at the Asan Medical Center, Korea. For diagnosing obstructive diseases, the accuracy of '0.7 of LLN for the FEV1/FVC' was evaluated in reference to the 5th percentile of the LLN. By applying the new algorithm, we determined how many more subjects should have lung volumes testing performed. Evaluation of 1611 patients who had lung volumes testing performed as well as spirometry during the period showed how many more subjects were diagnosed with obstructive diseases according to the new algorithm.
RESULTS
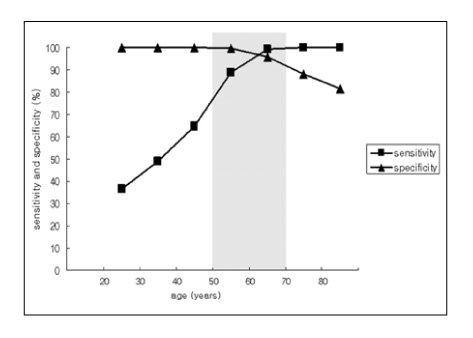
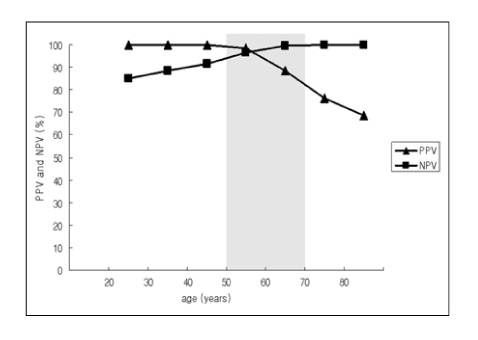
1) The sensitivity of '0.7 of LLN for the FEV1/FVC' for diagnosing obstructive diseases increased according to age, but the specificity was decreased according to age; the positive predictive value decreased, but the negative predictive value increased. 2) By applying the new algorithm, 34.5% (2540/7362) more subjects should have lung volumes testing performed. 3) By applying the new algorithm, 13% (205/1611) more subjects were diagnosed with obstructive diseases; these subjects corresponded to 30% (205/681) of the subjects who had been diagnosed with restrictive diseases by the old interpretative algorithm.
CONCLUSION
The sensitivity and specificity of '0.7 of LLN for the FEV1/FVC' for diagnosing obstructive diseases changes according to age. By applying the new interpretative algorithm, it was shown that more subjects should have lung volumes testing performed, and there was a higher probability of being diagnosed with obstructive diseases.
MeSH Terms
Figure
Reference
-
1. Gold WM. Murray JF, Nadel JA, editors. Pulmonary function testing. Textbook of respiratory medicine. 2005. 4th ed. Philadelphia: Saunders;671–733.2. Oh YM, Hong SB, Shim TS, Lim CM, Koh YS, Kim WS, et al. Effect of a new spirometric reference equation on the interpretation of spirometric patterns and disease severity. Tuberc Respir Dis. 2006. 60:215–220.3. Standards for the diagnosis and management of patients with COPD [Internet]. Version 1.2. American Thoracic Society/European Respiratory Society Task Force. 2004. updated 2005 September 8. New York: American Thoracic Society;Available from: http://www.thoracic.org/copd/.4. Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001. 163:1256–1276.5. American Thoracic Society. Lung function testing: selection of reference values and interpretative strategies. Am Rev Respir Dis. 1991. 144:1202–1218.6. Celli BR, Halbert RJ, Isonaka S, Schau B. Population impact of different definitions of airway obstruction. Eur Respir J. 2003. 22:268–273.7. Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005. 26:948–968.8. American Thoracic Society. Standardization of Spirometry, 1994 update. Am J Respir Crit Care Med. 1995. 152:1107–1136.9. Choi JK, Paek DM, Lee JO. Normal predictive values of spirometry in Korean population. Tuberc Respir Dis. 2005. 58:230–242.10. Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC. Official Statement of the European Respiratory Society. Lung volumes and forced ventilatory flows: report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Eur Respir J Suppl. 1993. 16:5–40.11. Song EH, Oh YM, Hong SB, Shim TS, Lim CM, Lee SD, et al. Selection of reference equations in lung volumes and in diffusing capacity. (Unpublished).12. Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999. 159:179–187.13. Hardie JA, Buist AS, Vollmer WM, Ellingsen I, Bakke PS, Morkve O. Risk of over-diagnosis of COPD in asymptomatic elderly never-smokers. Eur Respir J. 2002. 20:1117–1122.14. Brusasco V, Pellegrino R, Rodarte JR. Vital capacities in acute and chronic airway obstruction: dependence on flow and volume histories. Eur Respir J. 1997. 10:1316–1320.15. Hyatt RE, Okeson GC, Radarte JR. Influence of expiratory flow limitation on the pattern of lung emptying in normal man. J Appl Physiol. 1973. 35:411–419.16. Rodarte JR, Hyatt RE, Cortese DA. Influence of expiratory flow on closing capacity at low expiratory flow rates. J Appl Physiol. 1975. 39:60–65.17. Olive JT Jr, Hyatt RE. Maximal expiratory flow and total respiratory resistance during induced bronchoconstriction in asthmatic subjects. Am Rev Respir Dis. 1972. 106:366–376.18. Guerry-Force ML, Muller NL, Wright JL, Wiggs B, Coppin C, Pare PD, et al. A comparison of bron chiolitis obliterans with organizing pneumonia, usual interstitial pneumonia, and small airways disease. Am Rev Respir Dis. 1987. 135:705–712.19. Macklem PT, Thurlbeck WM, Fraser RG. Chronic obstructive disease of small airways. Ann Intern Med. 1971. 74:167–177.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Difference of Interpretations of Cardiopulmonary Exercise Testing According to Interpretative Algorithms and Exercise Methods
- Pattern of Cognitive Decline with Age in the Elderly
- Non-Interpretative Analytic Techniques for Sicker Borderline Patients
- Development of Rule-based Expert System for Interpretative Report with Health Screening Tests
- The Changes due to Enflurane and Balanced Anesthesia on Liver Function in Elective Operations