Korean J Urol.
2013 Feb;54(2):127-134.
Parent and Physician Perspectives on the Treatment of Primary Nocturnal Enuresis in Korea
- Affiliations
-
- 1Department of Urology, Eulji University Hospital, Daejeon, Korea. woosing@eulji.ac.kr
- 2Department of Pediatrics, Eulji University Hospital, Daejeon, Korea.
- 3Department of Urology, Pusan National University Children Hospital, Yangsan, Korea.
- 4Department of Urology, Korea University Guro Hospital, Seoul, Korea.
- 5Department of Urology, Chonnam National University Medical School, Gwangju, Korea.
- 6Department of Pediatrics, Hallym University Kangnam Sacred Heart Hospital, Seoul, Korea.
- 7Department of Urology, Soonchunhyang University School of Medicine, Cheonan, Korea.
Abstract
- PURPOSE
Parental decisions about the treatment of nocturnal enuresis (NE) are generally based on silent agreement with a physician's recommendation. However, physicians may have an insufficient understanding about parents' concerns and expectations regarding treatment. The aim of this study was to clarify the discrepancies between the perceptions of parents and physicians and to better understand the attitudes related to NE treatment.
MATERIALS AND METHODS
A survey was conducted in six centers and included 105 parents and 102 physicians. Two questionnaires, one for parents and another for physicians, were prepared. Each contained items on demographic characteristics, concerns, and NE treatment preferences. The parents completed the questionnaire during their child's first clinical visit, and the physicians completed the questionnaire via e-mail or individual interviews.
RESULTS
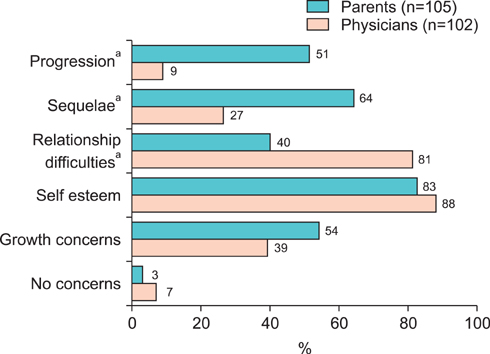
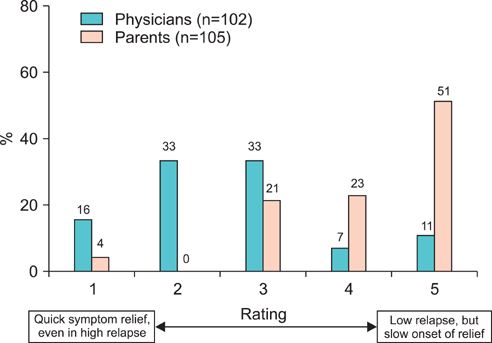
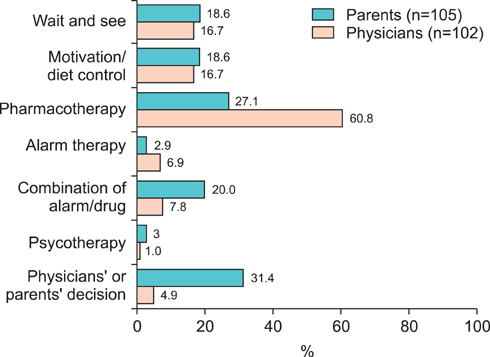
Low self-esteem was the most common concern among both parents and physicians. Parents showed a more serious concern regarding disease progression and sequelae than did physicians. In the parent group, parents of younger children were mainly concerned about growth, whereas parents of children with daytime symptoms were mainly concerned about disease progression and relationships. Treatment outcome preferences differed significantly between the two groups. Physicians preferred treatments yielding immediate results, whereas parents preferred long-term treatments that would result in low recurrence.
CONCLUSIONS
This survey presents the differences between parents and physicians regarding NE concerns and therapeutic preferences. Our study may provide valuable insight for physicians regarding parental attitudes toward NE treatment.
MeSH Terms
Figure
Reference
-
1. Neveus T, Eggert P, Evans J, Macedo A, Rittig S, Tekgul S, et al. Evaluation of and treatment for monosymptomatic enuresis: a standardization document from the International Children's Continence Society. J Urol. 2010. 183:441–447.2. Butler RJ, Holland P, Gasson S, Norfolk S, Houghton L, Penney M. Exploring potential mechanisms in alarm treatment for primary nocturnal enuresis. Scand J Urol Nephrol. 2007. 41:407–413.3. Butler RJ, Golding J, Heron J. ALSPAC Study Team. Nocturnal enuresis: a survey of parental coping strategies at 7 1/2 years. Child Care Health Dev. 2005. 31:659–667.4. Jang WS, Cho JS, Kim JM, Hong CH. Application and treatment result of an enuresis alarm based on a questionnaire in children with enuresis? Korean J Urol. 2008. 49:745–752.5. Hagglof B, Andren O, Bergstrom E, Marklund L, Wendelius M. Self-esteem before and after treatment in children with nocturnal enuresis and urinary incontinence. Scand J Urol Nephrol Suppl. 1997. 183:79–82.6. Meydan EA, Civilibal M, Elevli M, Duru NS, Civilibal N. The quality of life of mothers of children with monosymptomatic enuresis nocturna. Int Urol Nephrol. 2012. 44:655–659.7. Bower WF, Moore KH, Shepherd RB, Adams RD. The epidemiology of childhood enuresis in Australia. Br J Urol. 1996. 78:602–606.8. Lee SD, Sohn DW, Lee JZ, Park NC, Chung MK. An epidemiological study of enuresis in Korean children. BJU Int. 2000. 85:869–873.9. Shelov SP, Gundy J, Weiss JC, McIntire MS, Olness K, Staub HP, et al. Enuresis: a contrast of attitudes of parents and physicians. Pediatrics. 1981. 67:707–710.10. Liu X, Sun Z, Uchiyama M, Li Y, Okawa M. Attaining nocturnal urinary control, nocturnal enuresis, and behavioral problems in Chinese children aged 6 through 16 years. J Am Acad Child Adolesc Psychiatry. 2000. 39:1557–1564.11. Yeung CK, Sreedhar B, Sihoe JD, Sit FK, Lau J. Differences in characteristics of nocturnal enuresis between children and adolescents: a critical appraisal from a large epidemiological study. BJU Int. 2006. 97:1069–1073.12. Redsell SA, Collier J. Bedwetting, behaviour and self-esteem: a review of the literature. Child Care Health Dev. 2001. 27:149–162.13. Inan M, Tokuc B, Aydiner CY, Aksu B, Oner N, Basaran UN. Personal characteristics of enuretic children: an epidemiological study from South-East Europe. Urol Int. 2008. 81:47–53.14. Khan AG, Shahid A, Memon AA. Prevalence of nocturnal enuresis in children: a community study. Pak J Med Res. 2009. 48:75–78.15. Miskulin M, Miskulin I, Mujkic A, Dumic A, Puntaric D, Buljan V, et al. Enuresis in school children from eastern Croatia. Turk J Pediatr. 2010. 52:393–399.16. Gunes A, Gunes G, Acik Y, Akilli A. The epidemiology and factors associated with nocturnal enuresis among boarding and daytime school children in southeast of Turkey: a cross sectional study. BMC Public Health. 2009. 9:357.17. Foxman B, Valdez RB, Brook RH. Childhood enuresis: prevalence, perceived impact, and prescribed treatments. Pediatrics. 1986. 77:482–487.18. Kanaheswari Y. Epidemiology of childhood nocturnal enuresis in Malaysia. J Paediatr Child Health. 2003. 39:118–123.19. Ozkan S, Durukan E, Iseri E, Gurocak S, Maral I, Ali Bumin M. Prevalence and risk factors of monosymptomatic nocturnal enuresis in Turkish children. Indian J Urol. 2010. 26:200–205.20. Hanafin S. Sociodemographic factors associated with nocturnal enuresis. Br J Nurs. 1998. 7:403–408.21. Ozkan KU, Garipardic M, Toktamis A, Karabiber H, Sahinkanat T. Enuresis prevalence and accompanying factors in schoolchildren: a questionnaire study from southeast Anatolia. Urol Int. 2004. 73:149–155.22. Robson WL. Clinical practice. Evaluation and management of enuresis. N Engl J Med. 2009. 360:1429–1436.23. Moffatt ME, Harlos S, Kirshen AJ, Burd L. Desmopressin acetate and nocturnal enuresis: how much do we know? Pediatrics. 1993. 92:420–425.24. Evans JH, Meadow SR. Desmopressin for bed wetting: length of treatment, vasopressin secretion, and response. Arch Dis Child. 1992. 67:184–188.25. Ye JW, Lee SD. The comparison of therapeutic effect between imipramine and desmopressin on enuretic patients. Korean J Urol. 2001. 42:75–79.26. Wille S. Comparison of desmopressin and enuresis alarm for nocturnal enuresis. Arch Dis Child. 1986. 61:30–33.27. Kim WB, Kim KD. The epidemiology of childhood enuresis in Seoul and Kyunggi province. Korean J Urol. 1998. 39:1166–1170.28. Cho SC, Kim JW, Shin MS, Hwang JW, Han SW, Park KH, et al. Behavioral and emotional problems in children with nocturnal enuresis: results of a multicenter study. J Korean Neuropsychiatr Assoc. 2005. 44:730–735.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Oxybutynin Hydrochloride in 3 Cases of Clozapine Induced Nocturnal Enuresis
- Management of patients with refractory nocturnal enuresis
- The Relations between Enuresis in Childhood and Nocturnal Polyuria Syndrome in Adult Life
- Nocturnal Enuresis
- A Survey on the Conception and Cognition about Enuresis of Primary Care Physicians in Daegu City