Pediatr Gastroenterol Hepatol Nutr.
2015 Mar;18(1):60-65. 10.5223/pghn.2015.18.1.60.
Disseminated Cytomegalovirus Infection and Protein Losing Enteropathy as Presenting Feature of Pediatric Patient with Crohn's Disease
- Affiliations
-
- 1Department of Pediatric Gastroenterology Hepatology and Nutrition, Karadeniz Technical University, Trabzon, Turkey. muratcak@hotmail.com
- 2Department of Pathology, Faculty of Medicine, Karadeniz Technical University, Trabzon, Turkey.
- KMID: 2315537
- DOI: http://doi.org/10.5223/pghn.2015.18.1.60
Abstract
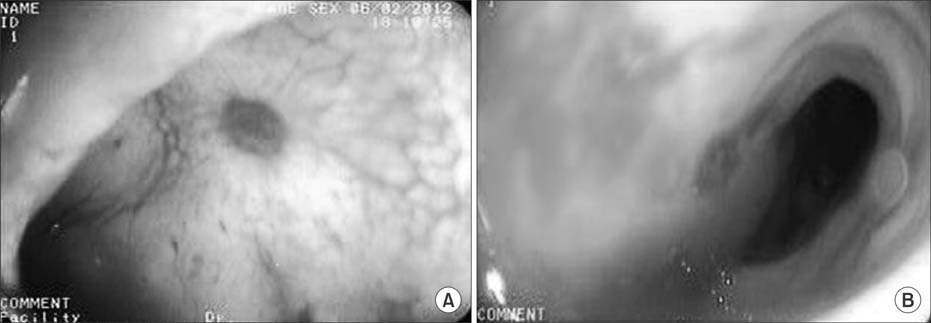
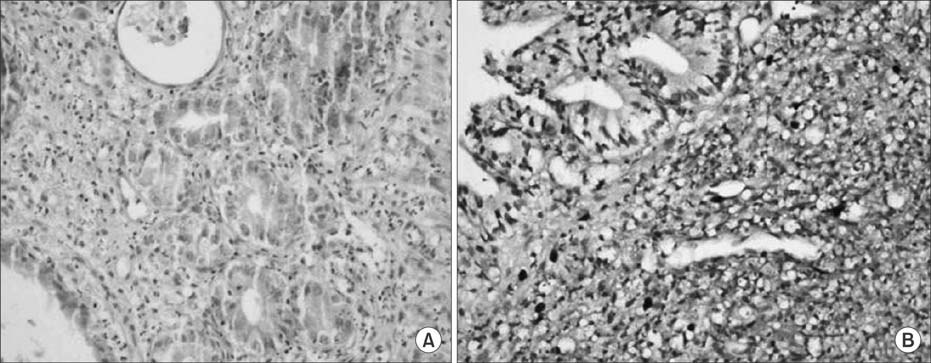
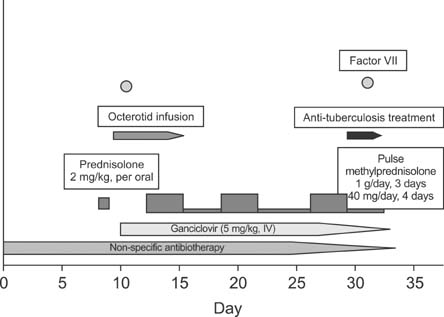
- We report a pediatric patient admitted with abdominal pain, diffuse lower extremity edema and watery diarrhea for two months. Laboratory findings including complete blood count, serum albumin, lipid and immunoglobulin levels were compatible with protein losing enteropathy. Colonoscopic examination revealed diffuse ulcers with smooth raised edge (like "punched out holes") in the colon and terminal ileum. Histopathological examination showed active colitis, ulcerations and inclusion bodies. Immunostaining for cytomegalovirus was positive. Despite supportive management, antiviral therapy, the clinical condition of the patient worsened and developed disseminated cytomegalovirus infection and the patient died. Protein losing enteropathy and disseminated cytomegalovirus infection a presenting of feature in steroid-naive patient with inflammatory bowel disease is very rare. Hypogammaglobulinemia associated with protein losing enteropathy in Crohn's disease may predispose the cytomegalovirus infection in previously healthy children.
MeSH Terms
Figure
Reference
-
1. Crough T, Khanna R. Immunobiology of human cytomegalovirus: from bench to bedside. Clin Microbiol Rev. 2009; 22:76–98.
Article2. Kim JJ, Simpson N, Klipfel N, Debose R, Barr N, Laine L. Cytomegalovirus infection in patients with active inflammatory bowel disease. Dig Dis Sci. 2010; 55:1059–1065.
Article3. Lawlor G, Moss AC. Cytomegalovirus in inflammatory bowel disease: pathogen or innocent bystander. Inflamm Bowel Dis. 2010; 16:1620–1627.
Article4. Umar SB, DiBaise JK. Protein-losing enteropathy: case illustrations and clinical review. Am J Gastroenterol. 2010; 105:43–49.
Article5. Ho M. The history of cytomegalovirus and its diseases. Med Microbiol Immunol. 2008; 197:65–73.
Article6. Yoshino T, Nakase H, Ueno S, Uza N, Inoue S, Mikami S, et al. Usefulness of quantitative real-time PCR assay for early detection of cytomegalovirus infection in patients with ulcerative colitis refractory to immunosuppressive therapies. Inflamm Bowel Dis. 2007; 13:1516–1521.
Article7. Matsuoka K, Iwao Y, Mori T, Sakuraba A, Yajima T, Hisamatsu T, et al. Cytomegalovirus is frequently reactivated and disappears without antiviral agents in ulcerative colitis patients. Am J Gastroenterol. 2007; 102:331–337.
Article8. Berk T, Gordon SJ, Choi HY, Cooper HS. Cytomegalovirus infection of the colon: a possible role in exacerbations of inflammatory bowel disease. Am J Gastroenterol. 1985; 80:355–360.9. Pfau P, Kochman ML, Furth EE, Lichtenstein GR. Cytomegalovirus colitis complicating ulcerative colitis in the steroid-naive patient. Am J Gastroenterol. 2001; 96:895–899.
Article10. Ghidini B, Bellaiche M, Berrebi D, Viala J, Hugot JP, Mougenot JF, et al. Cytomegalovirus colitis in children with inflammatory bowel disease. Gut. 2006; 55:582–583.
Article11. Inoue K, Wakabayashi N, Fukumoto K, Yamada S, Bito N, Yoshida N, et al. Toxic megacolon associated with cytomegalovirus infection in a patient with steroid-naïve ulcerative colitis. Intern Med. 2012; 51:2739–2743.
Article12. Ferrante M, Penninckx F, De Hertogh G, Geboes K, D'Hoore A, Noman M, et al. Protein-losing enteropathy in Crohn's disease. Acta Gastroenterol Belg. 2006; 69:384–389.
Article13. Sferra TJ, Pawel BR, Qualman SJ, Li BU. Ménétrier disease of childhood: role of cytomegalovirus and transforming growth factor alpha. J Pediatr. 1996; 128:213–219.
Article14. Orvar K, Murray J, Carmen G, Conklin J. Cytomegalovirus infection associated with onset of inflammatory bowel disease. Dig Dis Sci. 1993; 38:2307–2310.
Article15. van Dorp WT, Jonges E, Bruggeman CA, Daha MR, van Es LA, van Der Woude FJ. Direct induction of MHC class I, but not class II, expression on endothelial cells by cytomegalovirus infection. Transplantation. 1989; 48:469–472.
Article16. Domènech E, Vega R, Ojanguren I, Hernández A, Garcia-Planella E, Bernal I, et al. Cytomegalovirus infection in ulcerative colitis: a prospective, comparative study on prevalence and diagnostic strategy. Inflamm Bowel Dis. 2008; 14:1373–1379.
Article17. Turner D, Travis SP, Griffiths AM, Ruemmele FM, Levine A, Benchimol EI, et al. European Crohn's and Colitis Organization. Porto IBD Working Group, European Society of Pediatric Gastroenterology, Hepatology, and Nutrition. Consensus for managing acute severe ulcerative colitis in children: a systematic review and joint statement from ECCO, ESPGHAN, and the Porto IBD Working Group of ESPGHAN. Am J Gastroenterol. 2011; 106:574–588.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of constrictive pericarditis presenting with protein-losing enteropathy
- A case of systemic lupus erythematosus with chylothorax, chronic interstitial cystitis and protein-losing enteropathy
- A Case of Eosinophilic Gastroenteritis Associsted with Protein - losing Enteropathy
- Protein losing enteropathy
- Protein-Losing Enteropathy as a Complication of the Ketogenic Diet