Korean J Urol.
2011 Sep;52(9):616-621.
Laparoendoscopic Single-Site Pyeloplasty Using Additional 2 mm Instruments: A Comparison with Conventional Laparoscopic Pyeloplasty
- Affiliations
-
- 1Department of Urology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. deokhyun.han@samsung.com
Abstract
- PURPOSE
Despite a recent surge in the performance of laparoendoscopic single-site surgery (LESS), concerns remain about performing LESS pyeloplasty (LESS-P) because of the technical difficulty in suturing. We report our techniques and initial experiences with LESS-P using additional needlescopic instruments and compare the results with conventional laparoscopic pyeloplasty (CL-P).
MATERIALS AND METHODS
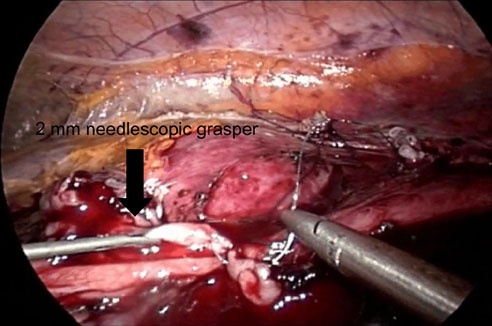
Nine patients undergoing LESS-P were matched 2:1 with regard to age and side of surgery to a previous cohort of 18 patients who underwent CL-P. In both groups, the operating procedures were performed equally except for the number of access points. In the LESS-P group, we made a single 2 cm incision at the umbilicus and used a homemade port. We also used additional 2 mm needlescopic instruments at the subcostal area to facilitate suturing and the ureteral stenting.
RESULTS
The preoperative characteristics were comparable in both groups. Postoperatively, no significant differences were noted between the LESS-P and CL-P cases in regard to length of stay, estimated blood loss, analgesics required, and complications. But, LESS-P was associated with a shorter operative time (252.2 vs. 309.7 minutes, p=0.044) and less pain on postoperative day one (numeric rating scale 3.7 vs. 5.6, p=0.024). The success rate was 94% with CL-P (median, 23 months) and 100% with LESS-P (median, 14 months).
CONCLUSIONS
Our initial experiences suggest that LESS-P is a feasible and safe procedure. The use of additional 2 mm instruments can help to overcome the difficulties associated with LESS surgery.
MeSH Terms
Figure
Reference
-
1. Chamie K, Tanaka ST, Hu B, Kurzrock EA. Short stay pyeloplasty: variables affecting pain and length of stay. J Urol. 2008. 179:1549–1552.2. Schuessler WW, Grune MT, Tecuanhuey LV, Preminger GM. Laparoscopic dismembered pyeloplasty. J Urol. 1993. 150:1795–1799.3. Winfield HN. Management of adult ureteropelvic junction obstruction--is it time for a new gold standard? J Urol. 2006. 176:866–867.4. Raman JD, Bagrodia A, Cadeddu JA. Single-incision, umbilical laparoscopic versus conventional laparoscopic nephrectomy: a comparison of perioperative outcomes and short-term measures of convalescence. Eur Urol. 2009. 55:1198–1204.5. Raybourn JH 3rd, Rane A, Sundaram CP. Laparoendoscopic single-site surgery for nephrectomy as a feasible alternative to traditional laparoscopy. Urology. 2010. 75:100–103.6. Canes D, Berger A, Aron M, Brandina R, Goldfarb DA, Shoskes D, et al. Laparo-endoscopic single site (LESS) versus standard laparoscopic left donor nephrectomy: matched-pair comparison. Eur Urol. 2010. 57:95–101.7. Tracy CR, Raman JD, Bagrodia A, Cadeddu JA. Perioperative outcomes in patients undergoing conventional laparoscopic versus laparoendoscopic single-site pyeloplasty. Urology. 2009. 74:1029–1034.8. White WM, Goel RK, Kaouk JH. Single-port laparoscopic retroperitoneal surgery: initial operative experience and comparative outcomes. Urology. 2009. 73:1279–1282.9. Desai MM, Rao PP, Aron M, Pascal-Haber G, Desai MR, Mishra S, et al. Scarless single port transumbilical nephrectomy and pyeloplasty: first clinical report. BJU Int. 2008. 101:83–88.10. Stein RJ, Berger AK, Brandina R, Patel NS, Canes D, Irwin BH, et al. Laparoendoscopic single-site pyeloplasty: a comparison with the standard laparoscopic technique. BJU Int. 2011. 107:811–815.11. Kim TH, Jeong BC, Seo SI, Jeon SS, Han DH. Transumbilical laparoendoscopic single-site ureterolithotomy for large impacted ureteral stones: initial experiences. Korean J Urol. 2010. 51:403–408.12. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004. 240:205–213.13. Calvert RC, Morsy MM, Zelhof B, Rhodes M, Burgess NA. Comparison of laparoscopic and open pyeloplasty in 100 patients with pelvi-ureteric junction obstruction. Surg Endosc. 2008. 22:411–414.14. Rassweiler JJ, Teber D, Frede T. Complications of laparoscopic pyeloplasty. World J Urol. 2008. 26:539–547.15. Moon DA, El-Shazly MA, Chang CM, Gianduzzo TR, Eden CG. Laparoscopic pyeloplasty: evolution of a new gold standard. Urology. 2006. 67:932–936.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoendoscopic Single-Site Urologic Surgery in Children Less Than 5 Years of Age
- Experiences on Anderson-Hynes Pyeloplasty
- Comparison of intraoperative and short-term postoperative outcomes between robot-assisted laparoscopic multi-port pyeloplasty using the da Vinci Si system and single-port pyeloplasty using the da Vinci SP system in children
- Concomitant Laparoendoscopic Single-Site Surgery for Ureterolithotomy and Contralateral Renal Cyst Marsupialization
- Hybrid laparoscopic myomectomy: A novel technique