Korean J Urol.
2010 Sep;51(9):625-630.
Prevalence and Treatment Efficacy of Genitourinary Mycoplasmas in Women with Overactive Bladder Symptoms
- Affiliations
-
- 1Department of Urology, Sungkyunkwan University School of Medicine, Seoul, Korea. ksleedr@skku.edu
- 2Department of Urology, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of Urology, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 4Department of Urology, Inha University College of Medicine, Incheon, Korea.
Abstract
- PURPOSE
To evaluate the incidence of genitourinary mycoplasmas and the efficacy of antibiotics in women with overactive bladder (OAB) symptoms.
MATERIALS AND METHODS
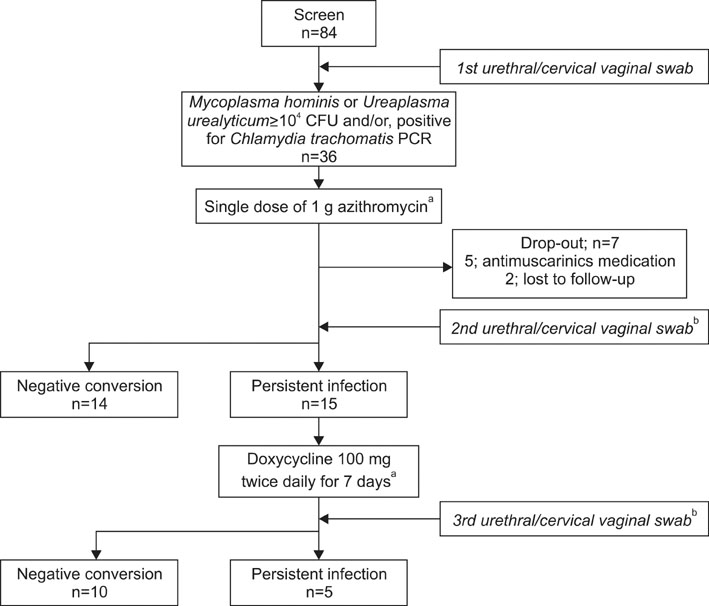
Women with OAB symptoms (micturition > or =8/24 hours and urgency > or =1/24 hours) for > or =3 months were screened for Mycoplasma hominis (M. hominis), Ureaplasma urealyticum (U. urealyticum), and Chlamydia trachomatis (C. trachomatis). Specimens from urethral and cervical vaginal swabs were examined for M. hominis and U. urealyticum by using the Mycoplasma IST2 kit and for C. trachomatis by using PCR. Women with positive results were treated with a 1 g dose of azithromycin. Persistent infection was treated with doxycycline. Changes in a 3-day bladder diary, Patient Perception of Bladder Condition (PPBC), and International Consultation on Incontinence Questionnaire-Female Lower Urinary Tract Symptoms (ICIQ-FLUTS) were evaluated 4 weeks after negative conversion. Patient satisfaction was assessed.
RESULTS
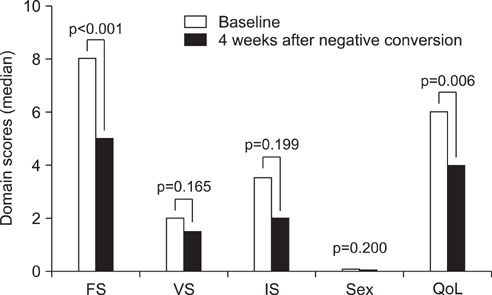
Of 84 women screened, 42.8% were positive (U. urealyticum, 40.5%; M. hominis, 7.1%; C. trachomatis, 3.6%; two organisms, 8.3%). After treatment, 82.7% obtained negative conversion, and their median number of micturition episodes decreased from 10.6/24 hours to 8.1/24 hours (p=0.002). PPBC and domain scores of the ICIQ-FLUTS (filling and quality of life) significantly improved. About 87.5% women with negative conversion were satisfied with the treatment.
CONCLUSIONS
Considering diagnostic tests and treatment for genitourinary mycoplasmas might be beneficial before invasive workup or treatment in women with OAB symptoms.
Keyword
MeSH Terms
-
Anti-Bacterial Agents
Azithromycin
Chlamydia trachomatis
Diagnostic Tests, Routine
Doxycycline
Female
Humans
Incidence
Lower Urinary Tract Symptoms
Mycoplasma
Mycoplasma hominis
Patient Satisfaction
Polymerase Chain Reaction
Prevalence
Treatment Outcome
Ureaplasma urealyticum
Urinary Bladder
Urinary Bladder, Overactive
Urination
Anti-Bacterial Agents
Azithromycin
Doxycycline
Figure
Reference
-
1. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002. 21:167–178.2. Potts JM, Ward AM, Rackley RR. Association of chronic urinary symptoms in women and Ureaplasma urealyticum. Urology. 2000. 55:486–489.3. Burkhard FC, Blick N, Hochreiter WW, Studer UE. Urinary urgency and frequency, and chronic urethral and/or pelvic pain in females. Can doxycycline help? J Urol. 2004. 172:232–235.4. Baka S, Kouskouni E, Antonopoulou S, Sioutis D, Papakonstantinou M, Hassiakos D, et al. Prevalence of ureaplasma urealyticum and mycoplasma hominis in women with chronic urinary symptoms. Urology. 2009. 74:62–66.5. Razin S. Balows A, Truper HG, Dworkin M, Harder W, Schleifer KH, editors. The genera mycoplasma, ureaplasma, acholeplasma, anaeroplasma, and asteroleplasma. The prokaryotes. 1991. 2nd ed. New York: Springer-Verlag;1937–1959.6. Krause DC, Taylor-Robinson D. Maniloff RN, Mcelhaney LR, Finch JB, editors. Mycoplasmas which infect humans. Mycoplasmas: molecular biology and pathogenesis. 1992. Washington DC: American Society for Microbiology;417–444.7. Dallo SF, Baseman JB. Intracellular DNA replication and long-term survival of pathogenic mycoplasmas. Microb Pathog. 2000. 29:301–309.8. Brewster-Jordan JL, Guan Z, Green HL, Jumadilova Z, Coyne KS. Establishing the content validity of the Urinary Sensation Scale (USS). 2005. Washington, DC: International Society for Pharmacoeconomics and Outcomes Research.9. Coyne KS, Matza LS, Kopp Z, Abrams P. The validation of the patient perception of bladder condition (PPBC): a single-item global measure for patients with overactive bladder. Eur Urol. 2006. 49:1079–1086.10. Brookes ST, Donovan JL, Wright M, Jackson S, Abrams P. A scored form of the Bristol Female Lower Urinary Tract Symptoms questionnaire: data from a randomized controlled trial of surgery for women with stress incontinence. Am J Obstet Gynecol. 2004. 191:73–82.11. Kilic D, Basar MM, Kaygusuz S, Yilmaz E, Basar H, Batislam E. Prevalence and treatment of Chlamydia trachomatis, Ureaplasma urealyticum, and Mycoplasma hominis in patients with non-gonococcal urethritis. Jpn J Infect Dis. 2004. 57:17–20.12. Pleil AM, Coyne KS, Reese PR, Jumadilova Z, Rovner ES, Kelleher CJ. The validation of patient-rated global assessments of treatment benefit, satisfaction, and willingness to continue--the BSW. Value Health. 2005. 8:Suppl 1. S25–S34.13. Manhart LE, Holmes KK, Hughes JP, Houston LS, Totten PA. Mycoplasma genitalium among young adults in the United States: an emerging sexually transmitted infection. Am J Public Health. 2007. 97:1118–1125.14. Clegg A, Passey M, Yoannes M, Michael A. High rates of genital mycoplasma infection in the highlands of Papua New Guinea determined both by culture and by a commercial detection kit. J Clin Microbiol. 1997. 35:197–200.15. Tibaldi C, Cappello N, Latino MA, Masuelli G, Marini S, Benedetto C. Vaginal and endocervical microorganisms in symptomatic and asymptomatic non-pregnant females: risk factors and rates of occurrence. Clin Microbiol Infect. 2009. 15:670–679.16. Falk L, Fredlund H, Jensen JS. Signs and symptoms of urethritis and cervicitis among women with or without Mycoplasma genitalium or Chlamydia trachomatis infection. Sex Transm Infect. 2005. 81:73–78.17. Uno M, Deguchi T, Komeda H, Hayasaki M, Iida M, Nagatani M, et al. Mycoplasma genitalium in the cervices of Japanese women. Sex Transm Dis. 1997. 24:284–286.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Overactive Bladder and Urinary Incontinence in Adult Women: Prevalence and Effects on Daily Life and Sexual Activity
- Overactive Bladder
- Correlation between Overactive Bladder Syndrome and Obsessive Compulsive Disorder in Women
- The Urobiome and Its Role in Overactive Bladder
- Correlation analysis about effect of cardiovascular risk factors and disease in women on overactive bladder and stress urinary incontinence