Korean J Urol.
2010 Dec;51(12):836-842.
Biochemical Recurrence-Free and Cancer-Specific Survival after Radical Prostatectomy at a Single Institution
- Affiliations
-
- 1Department of Urology, Asan Medical Center, Ulsan University College of Medicine, Seoul, Korea. hjahn@amc.seoul.kr
Abstract
- PURPOSE
To analyze the biochemical recurrence-free and cancer-specific survival after radical prostatectomy in a consecutive series of patients with prostate cancer.
MATERIALS AND METHODS
We retrospectively reviewed data for 1,822 patients who underwent radical prostatectomy with pelvic lymph node dissection at our institution between 1990 and 2009. After excluding 498 patients who were treated with neoadjuvant androgen deprivation therapy or who were followed up for < or =6 months, we included 1324 patients (mean age, 64.4 years; mean prostate-specific antigen [PSA] level, 12.3 ng/ml). We assessed patient age at the time of surgery, preoperative PSA concentration, biopsy and pathologic Gleason scores, pathologic stage, surgical margin status, disease progression, and survival.
RESULTS
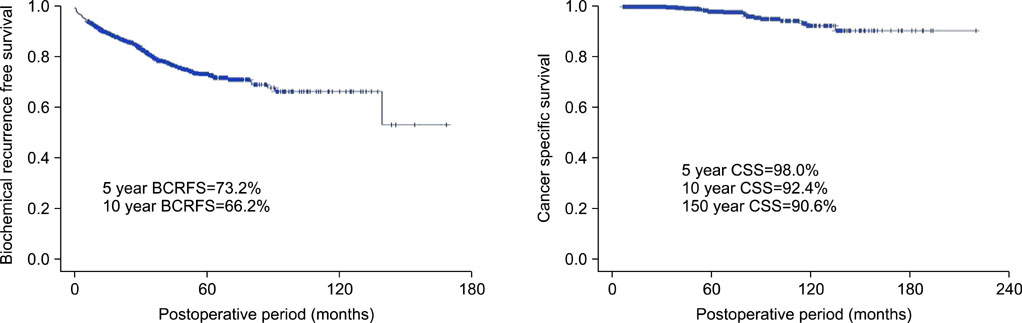
The mean follow-up time was 40 months (range, 6-193 months). The 5- and 10-year biochemical recurrence-free survival rates were 73.2% and 66.2%, respectively, and the 10-year cancer-specific survival rate was 92.4%. The mean time from surgery to biochemical recurrence was 18 months. In the multivariate analysis, Gleason score (4+3 vs. 2-6, p=0.004; 8-10 vs. 2-6, p<0.001), pathologic stage (pT3a vs. pT2, p=0.001; pT3b-4 vs. pT2, p<0.001; pN1 vs. pT2, p<0.001), and resection margin status (p<0.001) were statistically significant predictors of biochemical recurrence, with only pathologic stage (pT3b-4 vs. pT2, p=0.006; pN1 vs. pT2, p=0.010) being a statistically significant predictor of cancer-specific survival.
CONCLUSIONS
Radical prostatectomy resulted in favorable cancer control in more than 70% of patients after 5 years and a low (<10%) cancer-specific mortality rate after 10 years. The factors predictive of biochemical recurrence were Gleason score, pathologic stage, and resection margin status.
Keyword
MeSH Terms
Figure
Reference
-
1. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin. 2009. 59:225–249.2. Cooperberg MR, Lubeck DP, Mehta SS, Carroll PR. Time trends in clinical risk stratification for prostate cancer: implications for outcomes (data from CaPSURE). J Urol. 2003. 170:S21–S25.3. Schröder FH, Hugosson J, Roobol MJ, Tammela TL, Ciatto S, Nelen V, et al. Screening and prostate-cancer mortality in a randomized European study. N Engl J Med. 2009. 360:1320–1328.4. Whittemore AS. Prostate cancer. Cancer Surv. 1994. 19-20:309–322.5. The statistics report: the incidence of cancer on 2003-2005 and the survival rate on 1993-2005. National Cancer Center. 2009. accessed Apr 1, 2009. http://www.ncc.re.kr.6. Song C, Ro JY, Lee MS, Hong SJ, Chung BH, Choi HY, et al. Prostate cancer in Korean men exhibits poor differentiation and is adversely related to prognosis after radical prostatectomy. Urology. 2006. 68:820–824.7. Roehl KA, Han M, Ramos CG, Antenor JA, Catalona WJ. Cancer progression and survival rates following anatomical radical retropubic prostatectomy in 3,478 consecutive patients: long-term results. J Urol. 2004. 172:910–914.8. Hammad FT. Radical prostatectomy. Ann N Y Acad Sci. 2008. 1138:267–277.9. Reiner WG, Walsh PC. An anatomical approach to the surgical management of the dorsal vein and Santorinis plexus during radical retropubic surgery. J Urol. 1979. 121:198–200.10. Murphy GP, Busch C, Abrahamsson PA, Epstein JI, McNeal JE, Miller GJ, et al. Histopathology of localized prostate cancer. Consensus Conference on Diagnosis and Prognostic Parameters in Localized Prostate Cancer. Stockholm, Sweden, May 12-13, 1993. Scand J Urol Nephrol Suppl. 1994. 162:7–42.11. Epstein JI, Walsh PC, Carmichael M, Brendler CB. Pathologic and clinical findings to predict tumor extent of nonpalpable (stage T1c) prostate cancer. JAMA. 1994. 271:368–374.12. Song C, Kang T, Lee MS, Ro JY, Lee SE, Lee E, et al. Clinico-pathological characteristics of prostate cancer in Korean men and nomograms for the prediction of the pathological stage of the clinically localized prostate cancer: a multi-institutional update. Korean J Urol. 2007. 48:125–130.13. Xu DD, Sun SD, Wang F, Sun L, Stackhouse D, Polascik T, et al. Effect of age and pathologic Gleason score on PSA recurrence: analysis of 2911 patients undergoing radical prostatectomy. Urology. 2009. 74:654–658.14. Hull GW, Rabbani F, Abbas F, Wheeler TM, Kattan MW, Scardino PT. Cancer control with radical prostatectomy alone in 1,000 consecutive patients. J Urol. 2002. 167:528–534.15. Pound CR, Partin AW, Eisenberger MA, Chan DW, Pearson JD, Walsh PC. Natural history of progression after PSA elevation following radical prostatectomy. JAMA. 1999. 281:1591–1597.16. Stephenson AJ, Kattan MW, Eastham JA, Bianco FJ Jr, Yossepowitch O, Vickers AJ, et al. Prostate cancer-specific mortality after radical prostatectomy for patients treated in the prostate-specific antigen era. J Clin Oncol. 2009. 27:4300–4305.17. Porter CR, Kodama K, Gibbons RP, Correa R Jr, Chun FK, Perrotte P, et al. 25-year prostate cancer control and survival outcomes: a 40-year radical prostatectomy single institution series. J Urol. 2006. 176:569–574.18. Egawa S, Suyama K, Arai Y, Tsukayama C, Matsumoto K, Kuwao S, et al. Treatment outcome by risk group after radical prostatectomy in Japanese men. Int J Urol. 2001. 8:295–300.19. Hsu YS, Wang JS, Wu TT. E-cadherin expression in prostate adenocarcinomas in Chinese and its pathological correlates. Urol Int. 2004. 73:36–40.20. Khan MA, Han M, Partin AW, Epstein JI, Walsh PC. Long-term cancer control of radical prostatectomy in men younger than 50 years of age: update 2003. Urology. 2003. 62:86–91.21. D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998. 280:969–974.22. Freedland SJ, Aronson WJ, Kane CJ, Presti JC Jr, Amling CL, Elashoff D, et al. Impact of obesity on biochemical control after radical prostatectomy for clinically localized prostate cancer: a report by the Shared Equal Access Regional Cancer Hospital database study group. J Clin Oncol. 2004. 22:446–453.23. Han M, Partin AW, Pound CR, Epstein JI, Walsh PC. Long-term biochemical disease-free and cancer-specific survival following anatomic radical retropubic prostatectomy. The 15-year Johns Hopkins experience. Urol Clin North Am. 2001. 28:555–565.24. Wright JL, Dalkin BL, True LD, Ellis WJ, Stanford JL, Lange PH, et al. Positive surgical margins at radical prostatectomy predict prostate cancer specific mortality. J Urol. 2010. 183:2213–2218.25. Karakiewicz PI, Eastham JA, Graefen M, Cagiannos I, Stricker PD, Klein E, et al. Prognostic impact of positive surgical margins in surgically treated prostate cancer: multi-institutional assessment of 5831 patients. Urology. 2005. 66:1245–1250.26. Pettus JA, Weight CJ, Thompson CJ, Middleton RG, Stephenson RA. Biochemical failure in men following radical retropubic prostatectomy: impact of surgical margin status and location. J Urol. 2004. 172:129–132.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Tumor-Prostate Ratio on Biochemical Recurrence after Radical Prostatectomy
- External Validation of the Cancer of the Prostate Risk Assessment-S Score in Koreans Undergoing Radical Prostatectomy
- How can we best manage biochemical failure after radical prostatectomy?
- Influences of Neoadjuvant Androgen Ablation before Radical Prostatectomy on Positive Surgical Margin and Biochemical Recurrence Rate
- Comparison of biochemical recurrence in prostate cancer patients treated with radical prostatectomy or radiotherapy