Nutr Res Pract.
2015 Jun;9(3):268-277. 10.4162/nrp.2015.9.3.268.
Efficacy of mid-upper arm circumference in identification, follow-up and discharge of malnourished children during nutrition rehabilitation
- Affiliations
-
- 1Faculty of Bioscience Engineering, Ghent University, Coupure Links 653, B-9000 Ghent, Belgium. josephbirundu.mogendi@ugent.be
- 2School of Health and Related Research, University of Sheffield, (ScHARR); Regent Court, 30 Regent Street, Sheffield S1 4DA, UK.
- 3Department of Nutrition and Dietetics, School of Health Sciences, Mount Kenya University 342-01000, Thika, Kenya.
- 4Department of Food Science, Technology and Nutrition, Faculty of Agriculture, Jomo Kenyatta University of Agriculture and Technology, 62000-00200, Nairobi, Kenya.
- KMID: 2313840
- DOI: http://doi.org/10.4162/nrp.2015.9.3.268
Abstract
- BACKGROUND/OBJECTIVES
Although it is crucial to identify those children likely to be treated in an appropriate nutrition rehabilitation programme and discharge them at the appropriate time, there is no golden standard for such identification. The current study examined the appropriateness of using Mid-Upper Arm Circumference for the identification, follow-up and discharge of malnourished children. We also assessed its discrepancy with the Weight-for-Height based diagnosis, the rate of recovery, and the discharge criteria of the children during nutrition rehabilitation.
SUBJECTS/METHODS
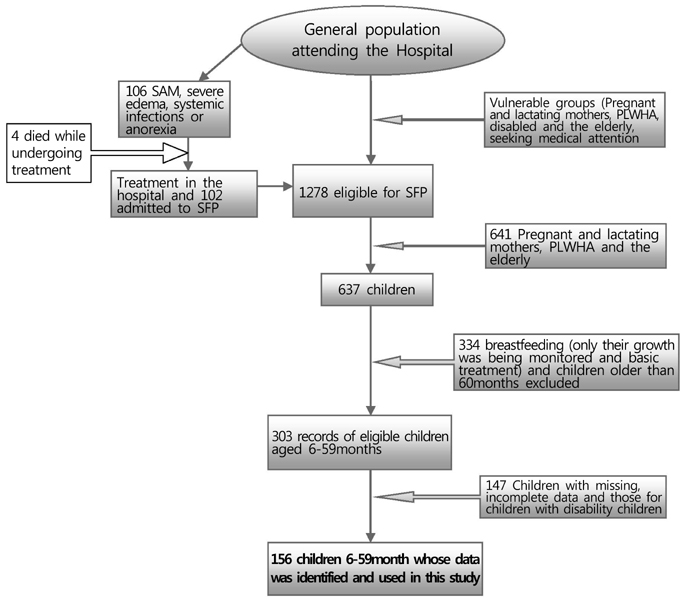
The study present findings from 156 children (aged 6-59 months) attending a supplementary feeding programme at Makadara and Jericho Health Centres, Eastern District of Nairobi, Kenya. Records of age, weight, height and mid-upper arm circumference were selected at three stages of nutrition rehabilitation: admission, follow-up and discharge. The values obtained were then used to calculate z-scores as defined by WHO Anthro while estimating different diagnostic indices.
RESULTS
Mid-upper arm circumference single cut-off (< 12.5 cm) was found to exhibit high values of sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood ratio, negative likelihood ratio at both admission and discharge. Besides, children recorded higher rate of recovery at 86 days, an average increment of 0.98 cm at the rate of 0.14mm/day, and a weight gain of 13.49gm/day, albeit higher in female than their male counterparts. Nevertheless, children admitted on basis of low MUAC had a significantly higher MUAC gain than WH at 0.19mm/day and 0.13mm/day respectively.
CONCLUSIONS
Mid-upper arm circumference can be an appropriate tool for identifying malnourished children for admission to nutrition rehabilitation programs. Our results confirm the appropriateness of this tool for monitoring recovery trends and discharging the children thereafter. In principle the tool has potential to minimize nutrition rehabilitation costs, particularly in community therapeutic centres in developing countries.
MeSH Terms
Figure
Reference
-
1. Blössner M, de Onis M. Malnutrition: Quantifying the Health Impact at National and Local Levels. Geneva: World Health Organization;2005.2. Caulfield LE, de Onis M, Blössner M, Black RE. Undernutrition as an underlying cause of child deaths associated with diarrhea, pneumonia, malaria, and measles. Am J Clin Nutr. 2004; 80:193–198.
Article3. de Onis M, Blössner M. The World Health Organization Global Database on Child Growth and Malnutrition: methodology and applications. Int J Epidemiol. 2003; 32:518–526.
Article4. Roberfroid D, Hammami N, Lachat C, Weise Prinzo Z, Sibson V, Guesdon B, Goosens S, Kolsteren P. Utilization of Mid-upper Arm Circumference Versus Weight-for-Height in Nutritional Rehabilitation Programmes: a Systematic Review of Evidence. Geneva: World Health Organization;2013.5. World Health Organization (CH). The World Health Report 2002. Reducing Risks, Promoting Healthy Life. Geneva: World Health Organization;2002.6. Goossens S, Bekele Y, Yun O, Harczi G, Ouannes M, Shepherd S. Mid-upper arm circumference based nutrition programming: evidence for a new approach in regions with high burden of acute malnutrition. PLoS One. 2012; 7:e49320.
Article7. Myatt M, Khara T, Collins S. A review of methods to detect cases of severely malnourished children in the community for their admission into community-based therapeutic care programs. Food Nutr Bull. 2006; 27:S7–S23.
Article8. Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, Mathers C, Rivera J. Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008; 371:243–260.
Article9. Tekeste A, Wondafrash M, Azene G, Deribe K. Cost effectiveness of community-based and in-patient therapeutic feeding programs to treat severe acute malnutrition in Ethiopia. Cost Eff Resour Alloc. 2012; 10:4.
Article10. Collins S. Changing the way we address severe malnutrition during famine. Lancet. 2001; 358:498–501.
Article11. World Health Organization. World Food Programme. United Nations System Standing Committee on Nutrition. The United Nations Children's Fund. Community-Based Management of Severe Acute Malnutrition [Internet]. Geneva: World Health Organization;2007. cited 2014 March 10. Available from: http://www.unicef.org/publications/files/Community_Based_Management_of_Sever_Acute__Malnutirtion.pdf.12. Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, Giugliani E, Haider BA, Kirkwood B, Morris SS, Sachdev HP, Shekar M. Maternal and Child Undernutrition Study Group. What works? Interventions for maternal and child undernutrition and survival. Lancet. 2008; 371:417–440.
Article13. Sadler K. Community-based therapeutic care: treating severe acute malnutrition in sub-Saharan Africa [doctoral thesis]. London: University of London;2009.14. Dale NM, Myatt M, Prudhon C, Briend A. Using mid-upper arm circumference to end treatment of severe acute malnutrition leads to higher weight gains in the most malnourished children. PLoS One. 2013; 8:e55404.
Article15. Shakir A. The surveillance of protein-calorie malnutrition by simple and economical means (a report to UNICEF). J Trop Pediatr Environ Child Health. 1975; 21:69–85.
Article16. Roy NC. Use of mid-upper arm circumference for evaluation of nutritional status of children and for identification of high-risk groups for malnutrition in rural Bangladesh. J Health Popul Nutr. 2000; 18:171–180.17. Bryce J, Coitinho D, Darnton-Hill I, Pelletier D, Pinstrup-Andersen P. Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: effective action at national level. Lancet. 2008; 371:510–526.
Article18. Briend A, Maire B, Fontaine O, Garenne M. Mid-upper arm circumference and weight-for-height to identify high-risk malnourished under-five children. Matern Child Nutr. 2012; 8:130–133.
Article19. Mwangome MK, Fegan G, Mbunya R, Prentice AM, Berkley JA. Reliability and accuracy of anthropometry performed by community health workers among infants under 6 months in rural Kenya. Trop Med Int Health. 2012; 17:622–629.
Article20. Lapidus N, Minetti A, Djibo A, Guerin PJ, Hustache S, Gaboulaud V, Grais RF. Mortality risk among children admitted in a large-scale nutritional program in Niger, 2006. PLoS One. 2009; 4:e4313.
Article21. Fernández MA, Delchevalerie P, Van Herp M. Accuracy of MUAC in the detection of severe wasting with the new WHO growth standards. Pediatrics. 2010; 126:e195–e201.
Article22. Myatt M, Duffield A, Seal A, Pasteur F. The effect of body shape on weight-for-height and mid-upper arm circumference based case definitions of acute malnutrition in Ethiopian children. Ann Hum Biol. 2009; 36:5–20.
Article23. Lagrone L, Cole S, Schondelmeyer A, Maleta K, Manary MJ. Locally produced ready-to-use supplementary food is an effective treatment of moderate acute malnutrition in an operational setting. Ann Trop Paediatr. 2010; 30:103–108.
Article24. Connor NE, Manary MJ, Maleta K. Monitoring the adequacy of catch-up growth among moderately malnourished children receiving home-based therapy using mid-upper arm circumference in southern Malawi. Matern Child Health J. 2011; 15:980–984.
Article25. Ciliberto MA, Sandige H, Ndekha MJ, Ashorn P, Briend A, Ciliberto HM, Manary MJ. Comparison of home-based therapy with ready-to-use therapeutic food with standard therapy in the treatment of malnourished Malawian children: a controlled, clinical effectiveness trial. Am J Clin Nutr. 2005; 81:864–870.
Article26. Smith LC, Haddad L. Explaining Child Malnutrition in Developing Countries: a Cross-Country Analysis. Washington, D.C.: International Food Policy Research Institute;2000.27. Lauritsen JM, Bruus M. EpiData (version 3): a Comprehensive Tool for Validated Entry and Documentation of Data. Odense: The EpiData Association;2008.28. StataCorp. Stata: Release 12. Statistical Software. College Station (TX): StataCorp LP.;2011.29. Hop le T, Gross R, Sastroamidjojo S, Giay T, Schultink W. Mid-upper-arm circumference development and its validity in assessment of undernutrition. Asia Pac J Clin Nutr. 1998; 7:65–69.30. Pelletier DL. The potentiating effects of malnutrition on child mortality: epidemiologic evidence and policy implications. Nutr Rev. 1994; 52:409–415.
Article31. Singh AS, Kang G, Ramachandran A, Sarkar R, Peter P, Bose A. Locally made ready to use therapeutic food for treatment of malnutrition a randomized controlled trial. Indian Pediatr. 2010; 47:679–686.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Performance of mid-upper arm circumference to diagnose acute malnutrition in a cross-sectional community-based sample of children aged 6–24 months in Niger
- Measurements of Mid-arm Circumference(MAC) and Mid-arm Circumference/Head Circumference(MAC/HC) Ratio as Indices of Nutritional Status in Newborn Infants
- Usefulness of Ultrasound Examination in Evaluation of Breast Cancer-Related Lymphedema
- Verification of the Appropriateness When a Shortened Version of the Mini Nutritional Assessment (MNA) Is Applied for Determining the Malnutrition State of Elderly Patients
- Utility of Subjective Global Nutritional Assessment Tool for the Assessment of Malnutrition in Pediatric Patients with Chronic Liver Disease