Korean J Hematol.
2006 Dec;41(4):311-316. 10.5045/kjh.2006.41.4.311.
A Case of Chronic Active Epstein-Barr Virus Infection with Autoimmnune Hepatitis and a Coronary Aneurysm
- Affiliations
-
- 1Department of Pediatrics, College of Medicine, Chungnam National University, Daejeon, Korea. sunyoung@cnuh.co.kr
- KMID: 2305220
- DOI: http://doi.org/10.5045/kjh.2006.41.4.311
Abstract
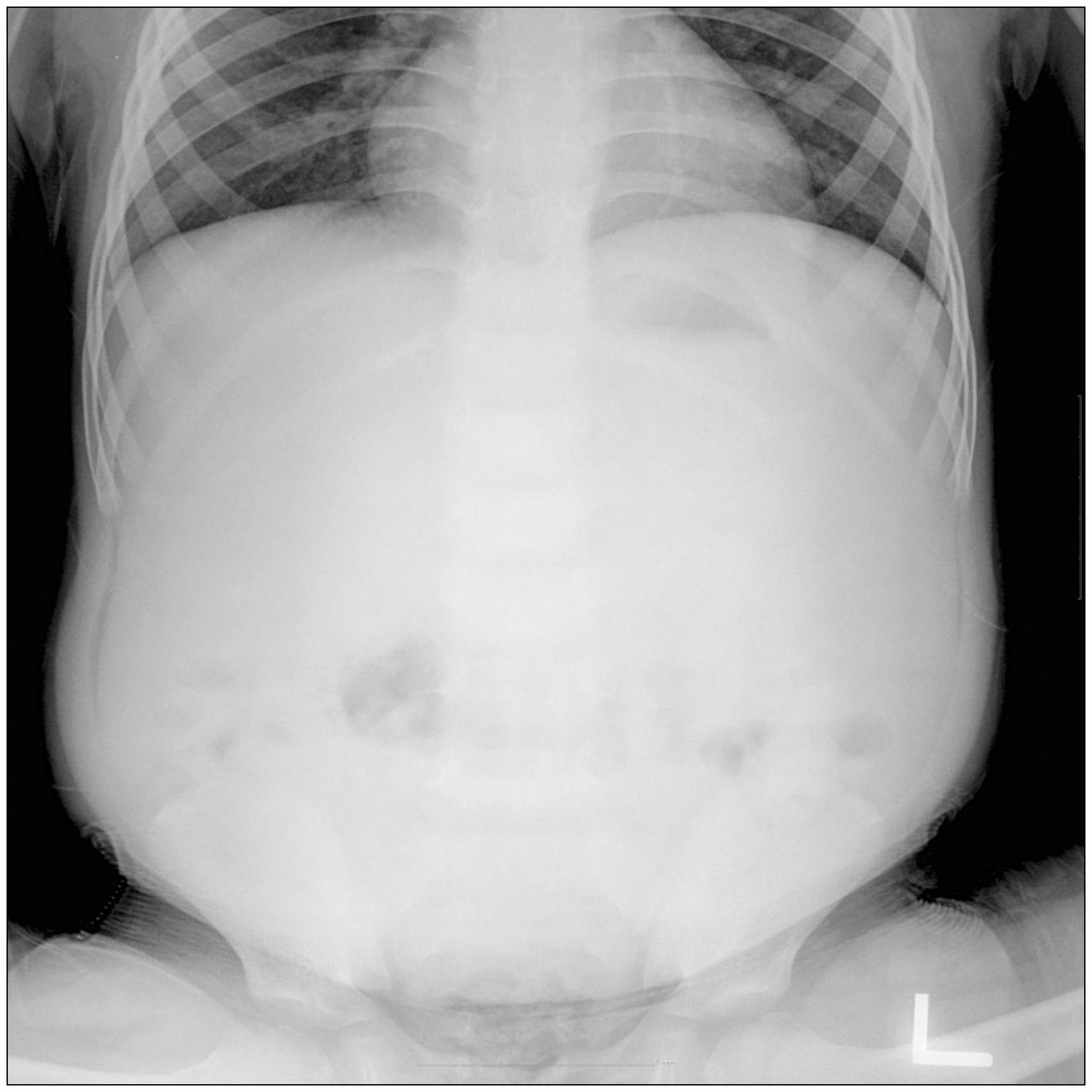
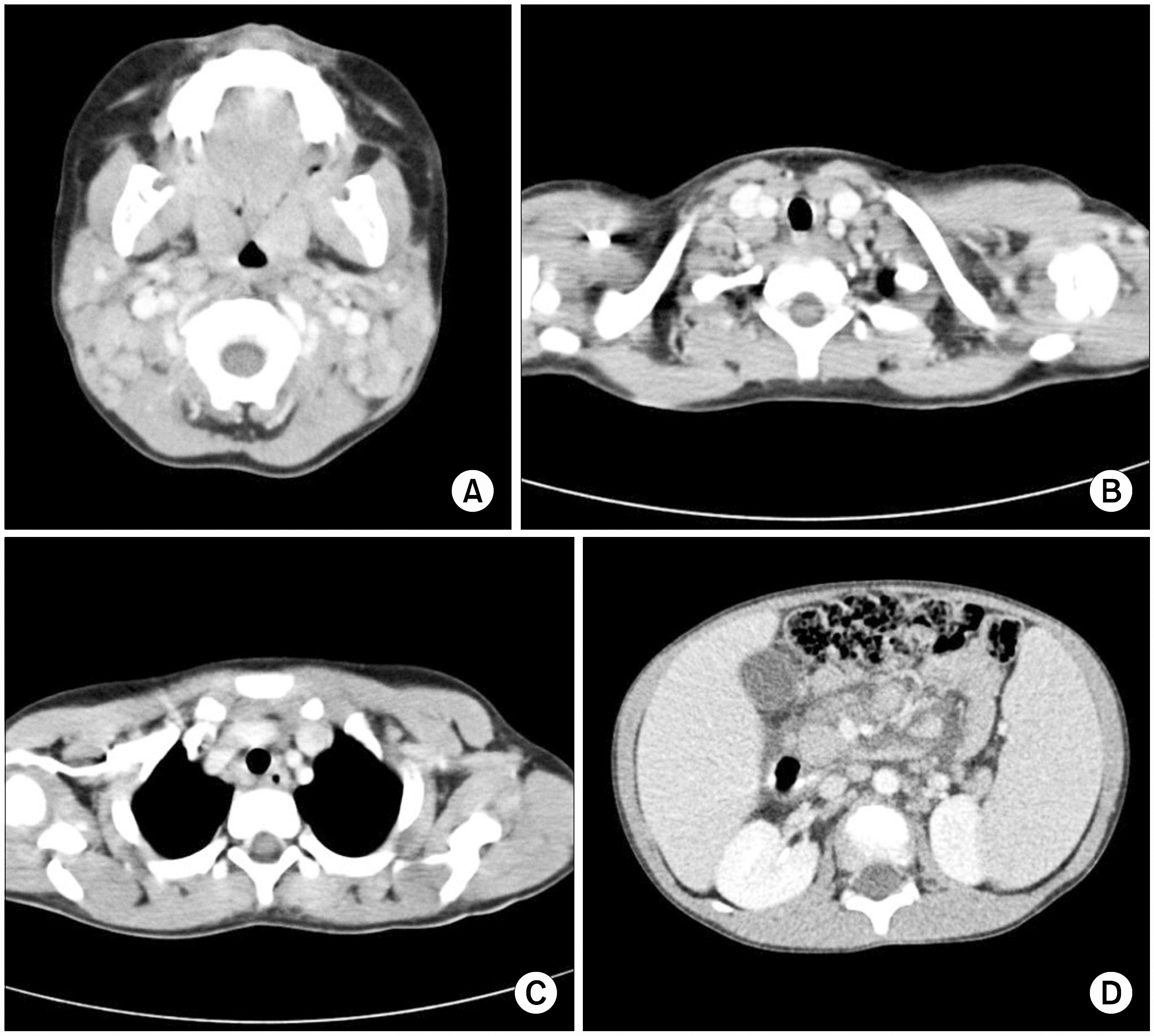
- Infectious mononucleosis caused by primary infection of Epstein-Barr virus (EBV) is a self-limiting lymphoproliferative disease, and shows concomitant clinical features such as pyrexia, anorexia, sore throat, cervical lymphadenopathy, liver dysfunction and hepatosplenomegaly. In rare cases, EBV establishes a latent infection in B lymphocytes and runs a chronic course and shows infectious mononucleosis-like symptoms repeatedly. This syndrome, named chronic active EBV infection, may trigger an autoimmune disease that mainly affectes the liver and red blood cells, and carries a very poor prognosis. The cardiovascular complications of chronic active EBV infection are very rare and may be associated with coronary arterial disease. This case describes a 5-year-old boy, who developed chronic active EBV infection and was diagnosed as having autoimmune hepatitis with a coronary aneurysm.
MeSH Terms
Figure
Reference
-
1). Cho HS., Kim IS., Park HC., Ahn MJ., Lee YY., Park CK. A case of severe chronic active Epstein-Barr virus infection with T-cell lymphoproliferative disorder. Korean J Intern Med. 2004. 19:124–7.
Article2). Cohen JI. Epstein-Barr virus infections. N Engl J Med. 2000. 343:481–92.
Article3). Jones JF., Shurin S., Abramowsky C, et al. T-cell lymphomas containing Epstein-Barr viral DNA in patients with chronic Epstein-Barr virus infections. N Engl J Med. 1988. 318:733–41.
Article4). Kawa-Ha K., Ishihara S., Ninomiya T, et al. CD3-negative lymphoproliferative disease of granular lymphocytes containing Epstein-Barr viral DNA. J Clin Invest. 1989. 84:51–5.
Article5). Nakagawa A., Ito M., Iwaki T., Yatabe Y., Asai J., Hayashi K. Chronic active Epstein-Barr virus infection with giant coronary aneurysms. Am J Clin Pathol. 1996. 105:733–6.
Article6). Murakami K., Ohsawa M., Hu SX., Kanno H., Aozasa K., Nose M. Large-vessel arteritis associated with chronic active Epstein-Barr virus infection. Arthritis Rheum. 1998. 41:369–73.
Article7). Kikuta H., Sakiyama Y., Matsumoto S, et al. Detection of Epstein-Barr virus DNA in cardiac and aortic tissues from chronic, active Epstein-Barr virus infection associated with Kawasaki disease-like coronary artery aneurysms. J Pediatr. 1993. 123:90–2.
Article8). Hsiao CC. Epstein-Barr virus associated with immune thrombocytopenic purpura in childhood: a retrospective study. J Pediatr Child Health. 2000. 36:445–8.
Article9). Nickerson C., Luthra H., David C. Antigenic mimicry and autoimmune disease. Int Rev Immunol. 1991. 7:205–24.10). Vento S., Guella L., Mirandola F, et al. Epstein-Barr virus as a trigger autoimmune hepatitis in susceptible individuals. Lancet. 1995. 346:608–9.11). Kikuta H., Mizuno F., Osato T, et al. Kawasaki disease and unusual primary infection with Epstein-Barr virus. Pediatrics. 1984. 73:413–4.12). Bernard O., Hadchouel M., Scotto J., Odievre M., Alagille D. Severe giant cell hepatitis with autoimmune hemolytic anemia in early childhood. J Pediatr. 1981. 99:704–11.
Article13). Melendez HV., Rela M., Baker AJ, et al. Liver trans-plant for giant cell hepatitis with autoimmune haemolytic anemia. Arch Dis Child. 1997. 77:249–51.14). Taketani T., Kikuchi A., Inatomi J, et al. Chronic active Epstein-Barr virus infection (CAEBV) successfully treated with allogenic peripheral blood stem cell transplantation. Bone Marrow Transplant. 2002. 29:531–3.15). Fujii N., Takenaka K., Hiraki A, et al. Allogenic peripheral blood stem cell transplatation for the treatment of chronic Epstein-Barr virus infection. Bone Marrow Transplant. 2000. 26:805–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Chronic Active Epstein-Barr Virus Infection with Coronary Aneurysm
- Several Cases of Epstein-Barr Virus Associated Hepatitis
- Epstein-Barr Virus Infection with Acute Pancreatitis Associated with Cholestatic Hepatitis
- A Case of Chronic Active Epstein-Barr Virus Infection Progressed to Peripheral T-cell Lymphoma of Lung
- A Case of Gianotti-Crosti Syndrome Associated with Epstein-Barr Virus Infection