Korean J Androl.
2011 Apr;29(1):53-61. 10.5534/kja.2011.29.1.53.
Medical Profession's Awareness and Attitude Toward the Sexuality of Cancer Patients in South Korea
- Affiliations
-
- 1Department of Urology, Samsung Medical Center, Sungkyunkwan University College of Medicine, Seoul, Korea. drswlee@skku.edu
- 2Department of Urology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2298626
- DOI: http://doi.org/10.5534/kja.2011.29.1.53
Abstract
- PURPOSE
To investigate the practice and attitude of healthcare professionals toward the sexuality of cancer patients.
MATERIALS AND METHODS
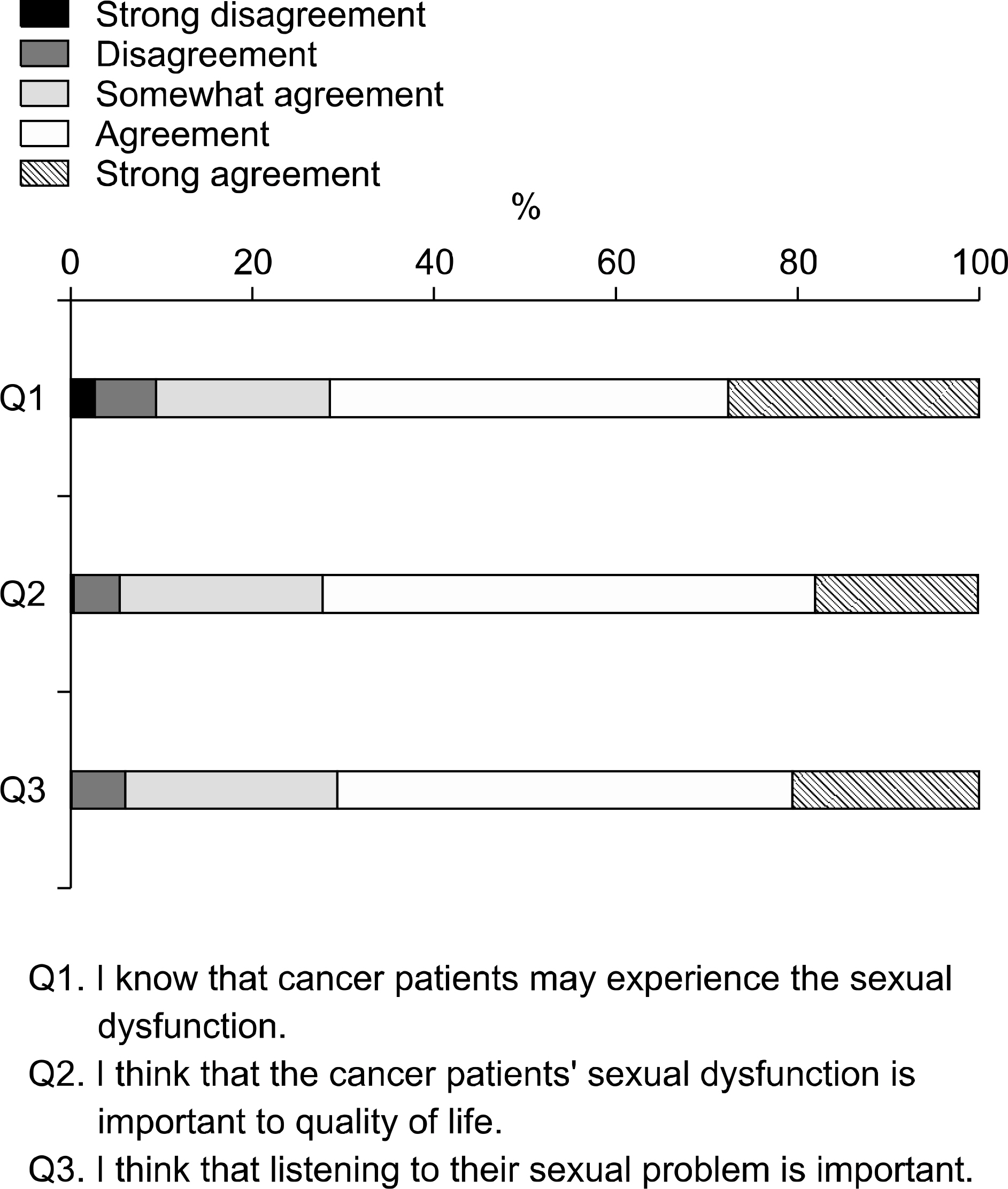
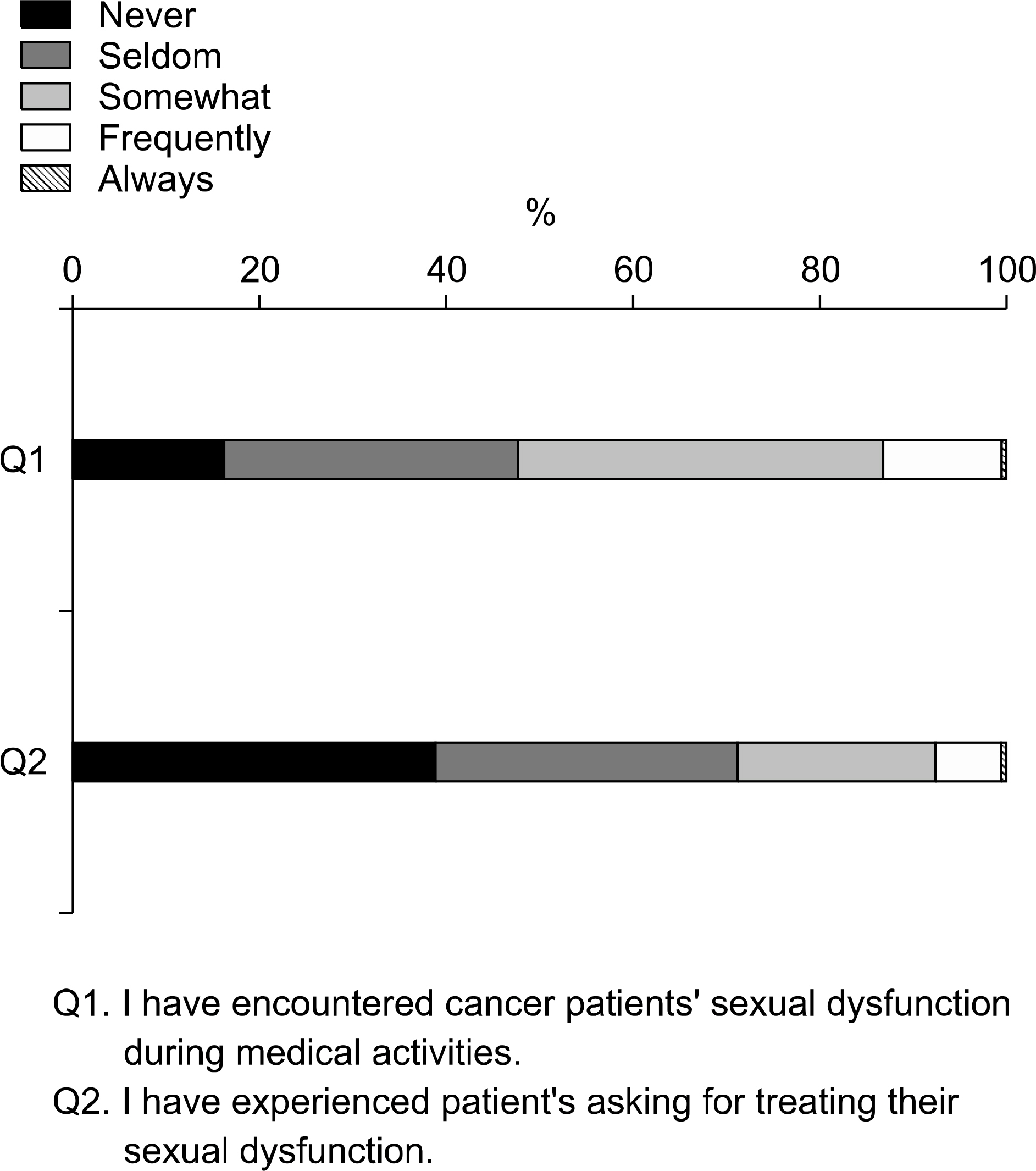
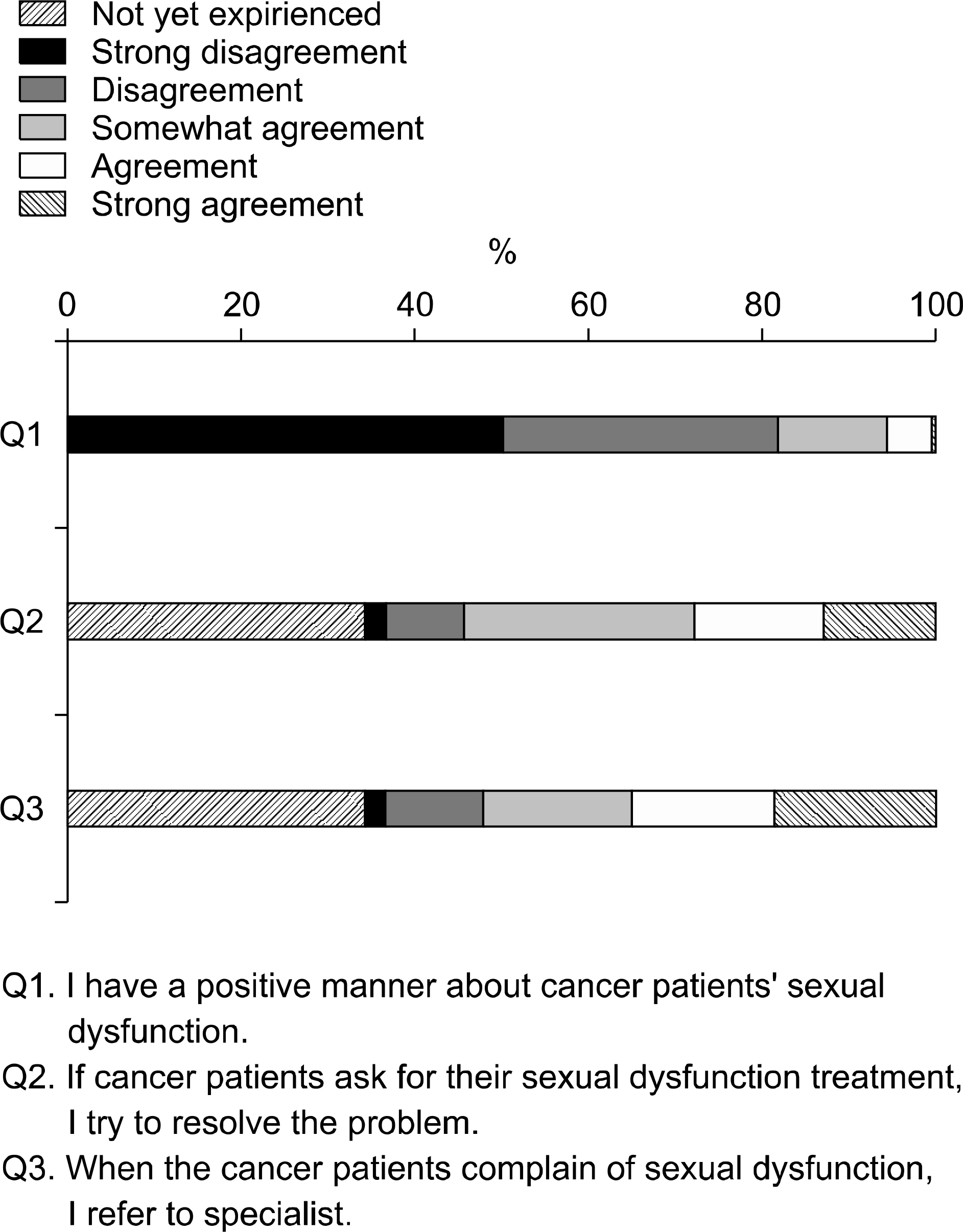
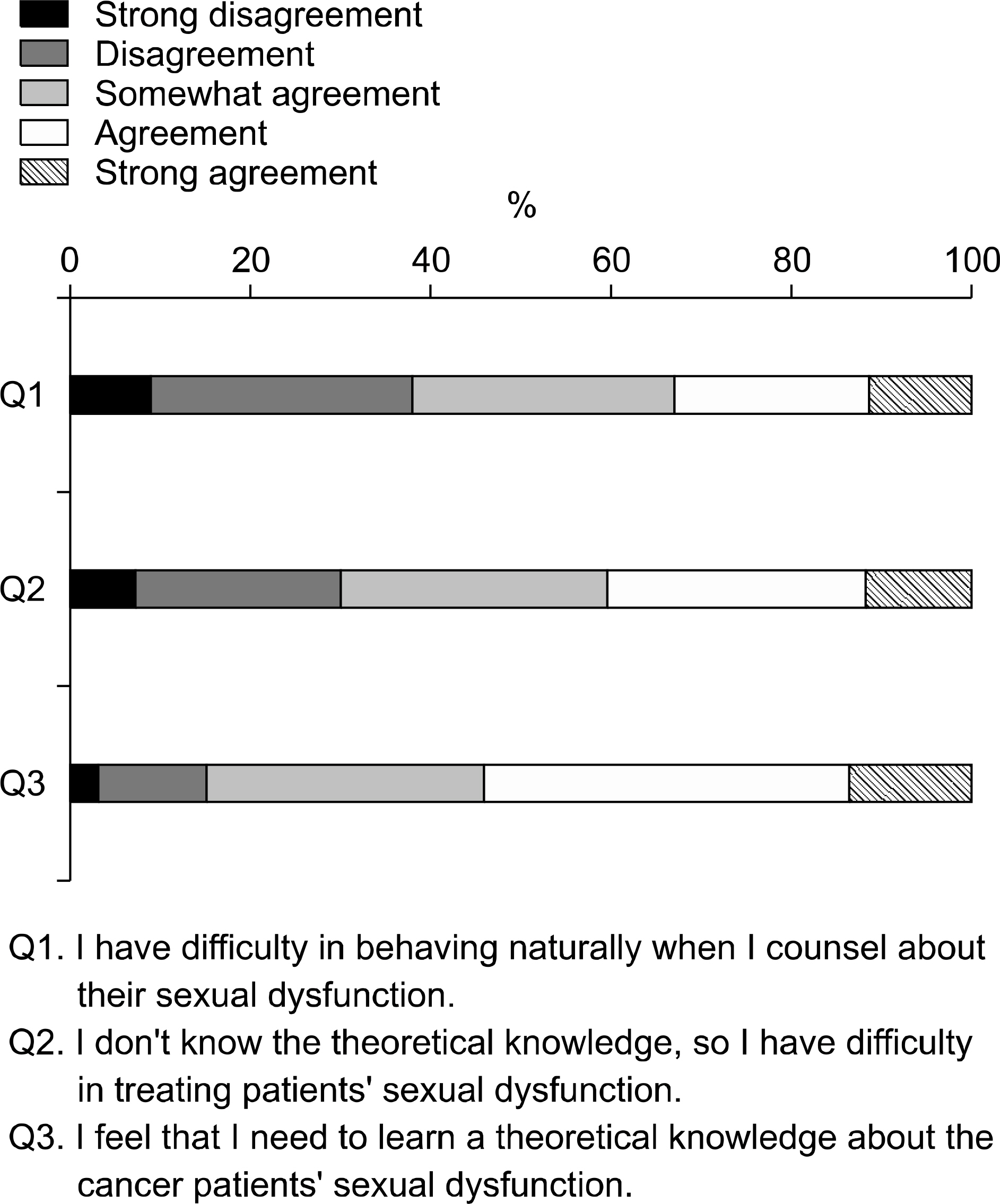
The subjects were comprised of doctors and nurses who served at two medical centers. Questionnaires consisted of five domains and fourteen questions were disseminated via emails in March 2009. The first domain (3 questions) pertained the recognition of sexual dysfunction in cancer patients, the second (2 questions) pertained cancer patients' experience of sexual dysfunction, the third (3 questions) pertained the attitude to cancer patients with sexual dysfunction, the fourth (3 questions) pertained capacity for sexual dysfunction treatment, and the fifth (3 questions) pertained problems or difficulties encountered when facing cancer patients' sexual dysfunction.
RESULTS
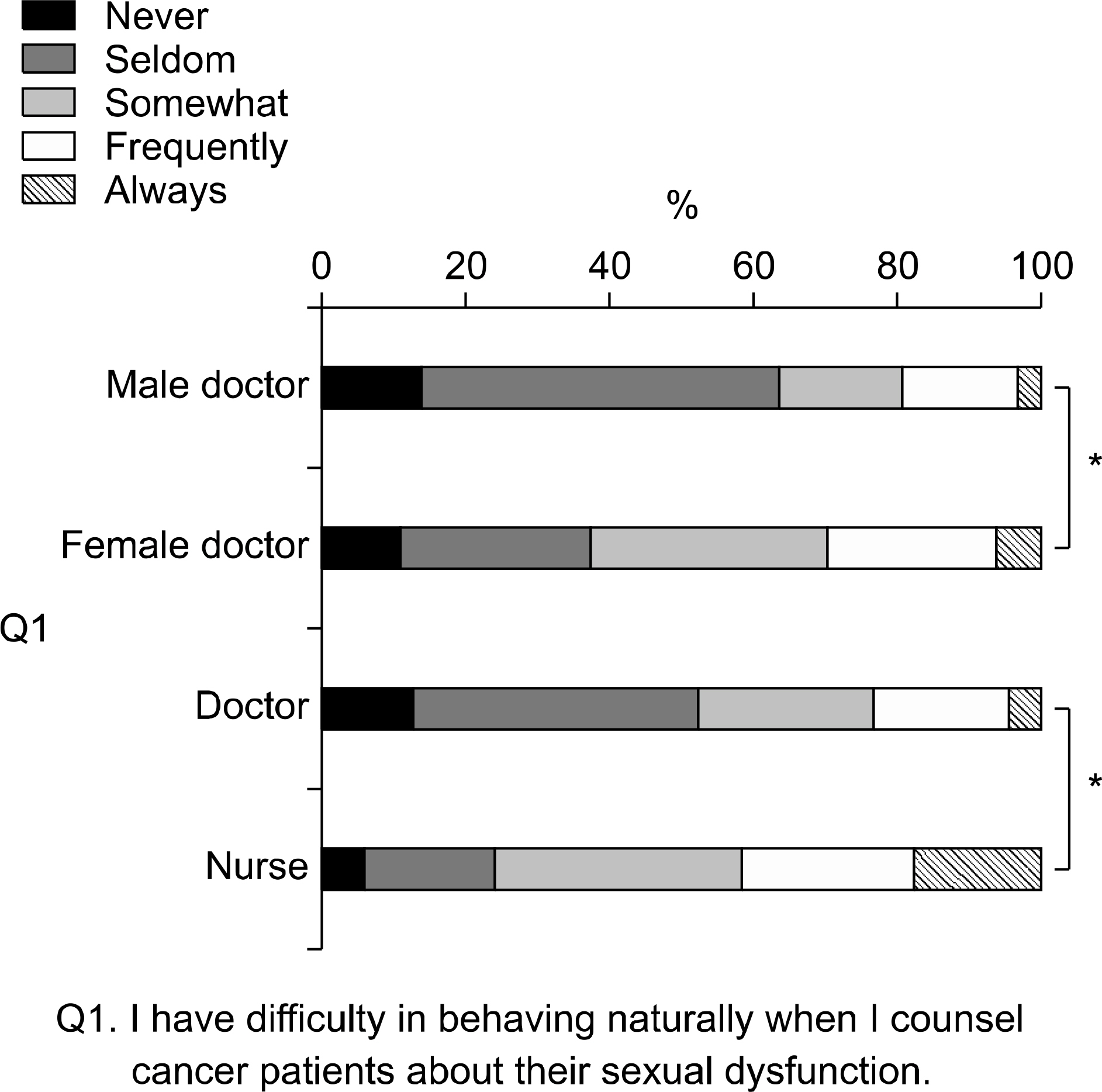
Three hundred and twenty-six men and women completed the questionnaires, giving a response rate of 85.4%. The mean age was 33.6 years. The proportion of doctors and nurses were respectively 48.2% and 51.8%. The proportion of males and females were 29.8%, and 70.2%, respectively. Ninety point five per cent (90.5%) of respondents answered that cancer patients' sexual dysfunction is important to quality of life. However, fewer medical professionals (27.4%) give an affirmative answer that patients requested sexual dysfunction therapy. The occurred particularly less frequently in physicians (13.2%) than in surgeons (55.6%). Fifty-four point six (54.6%) percent of respondents said that they tried to resolve the problem when patients asking for treatment of sexual dysfunction. Only 38.3% of respondents experienced little or no difficulty in behaving naturally when counseling cancer patients about their sexual dysfunction. Female doctors and nurses more often experience embarrassment when addressing sexuality with patients. In addition, most respondents (84.0%) felt that theoretical knowledge on cancer patients' problems is needed.
CONCLUSIONS
Most healthcare professionals agreed that sexual problems of cancer patients were important for quality of life. However, they frequently felt a lack of communicating skills and theoretical knowledge. Education programs on this issue and an appropriate contact system with specialists should be established.
Keyword
MeSH Terms
Figure
Reference
-
1). Won YJ, Sung J, Jung KW, Kong HJ, Park S, Shin HR, et al. Nationwide cancer incidence in Korea, 2003-2005. Cancer Res Treat. 2009; 41:122–31.
Article2). Andersen BL. Sexual functioning morbidity among cancer survivors. Current status and future research directions. Cancer. 1985; 55:1835–42.
Article3). Catalona WJ, Carvalhal GF, Mager DE, Smith DS. Potency, continence and complication rates in 1,870 consecutive radical retropubic prostatectomies. J Urol. 1999; 162:433–8.
Article4). Fulmer BR, Bissonette EA, Petroni GR, Theodorescu D. Prospective assessment of voiding and sexual function after treatment for localized prostate carcinoma: comparison of radical prostatectomy to hor-monobrachytherapy with and without external beam radiotherapy. Cancer. 2001; 91:2046–55.5). Guillonneau B, Cathelineau X, Doublet JD, Baumert H, Vallancien G. Laparoscopic radical prostatectomy: assessment after 550 procedures. Crit Rev Oncol Hematol. 2002; 43:123–33.
Article6). Katz R, Salomon L, Hoznek A, de la Taille A, Vordos D, Cicco A, et al. Patient reported sexual function following laparoscopic radical prostatectomy. J Urol. 2002; 168:2078–82.
Article7). Kundu SD, Roehl KA, Eggener SE, Antenor JA, Han M, Catalona WJ. Potency, continence and complications in 3,477 consecutive radical retropubic prostatectomies. J Urol. 2004; 172:2227–31.
Article8). Potosky AL, Davis WW, Hoffman RM, Stanford JL, Stephenson RA, Penson DF, et al. Five-year outcomes after prostatectomy or radiotherapy for prostate cancer: the prostate cancer outcomes study. J Natl Cancer Inst. 2004; 96:1358–67.
Article9). Schover LR, Evans R, von Eschenbach AC. Sexual rehabilitation and male radical cystectomy. J Urol. 1986; 136:1015–7.
Article10). Krouse R, Grant M, Ferrell B, Dean G, Nelson R, Chu D. Quality of life outcomes in 599 cancer and non-cancer patients with colostomies. J Surg Res. 2007; 138:79–87.
Article11). Jensen PT, Groenvold M, Klee MC, Thranov I, Petersen MA, Machin D. Early-stage cervical carcinoma, radical hysterectomy, and sexual function. A longitudinal study. Cancer. 2004; 100:97–106.12). Robinson JW. Sexuality and cancer. Breaking the silence. Aust Fam Physician. 1998; 27:45–7.13). Fobair P, Stewart SL, Chang S, D'Onofrio C, Banks PJ, Bloom JR. Body image and sexual problems in young women with breast cancer. Psychooncology. 2006; 15:579–94.
Article14). Barni S, Mondin R. Sexual dysfunction in treated breast cancer patients. Ann Oncol. 1997; 8:149–53.
Article15). Burwell SR, Case LD, Kaelin C, Avis NE. Sexual problems in younger women after breast cancer surgery. J Clin Oncol. 2006; 24:2815–21.
Article16). Ganz PA, Rowland JH, Desmond K, Meyerowitz BE, Wyatt GE. Life after breast cancer: understanding women's health-related quality of life and sexual functioning. J Clin Oncol. 1998; 16:501–14.
Article17). Al-Ghazal SK, Fallowfield L, Blamey RW. Does cosmetic outcome from treatment of primary breast cancer influence psychosocial morbidity? Eur J Surg Oncol. 1999; 25:571–3.
Article18). Walsh PC. Defining sexual outcomes after treatment for localized prostate carcinoma. J Urol. 2003; 169:1594–5.19). Carmack Taylor CL, Basen-Engquist K, Shinn EH, Bodurka DC. Predictors of sexual functioning in ovarian cancer patients. J Clin Oncol. 2004; 22:881–9.
Article20). Reese JB, Keefe FJ, Somers TJ, Abernethy AP. Coping with sexual concerns after cancer: the use of flexible coping. Support Care Cancer. 2010; 18:785–800.
Article21). Ganz PA, Kwan L, Stanton AL, Krupnick JL, Rowland JH, Meyerowitz BE, et al. Quality of life at the end of primary treatment of breast cancer: first results from the moving beyond cancer randomized trial. J Natl Cancer Inst. 2004; 96:376–87.
Article22). Schover LR. Sexual rehabilitation after treatment for prostate cancer. Cancer. 1993; 71(Suppl 3):1024–30.
Article23). Galbraith ME, Crighton F. Alterations of sexual function in men with cancer. Semin Oncol Nurs. 2008; 24:102–14.
Article24). Hughes MK. Alterations of sexual function in women with cancer. Semin Oncol Nurs. 2008; 24:91–101.
Article25). Schover LR. Sexuality and fertility after cancer. Hematology Am Soc Hematol Educ Program. 2005. 523–7.
Article26). Tierney DK. Sexuality: a quality-of-life issue for cancer survivors. Semin Oncol Nurs. 2008; 24:71–9.
Article27). Sadovsky R, Basson R, Krychman M, Morales AM, Schover L, Wang R, et al. Cancer and sexual problems. J Sex Med. 2010; 7:349–73.
Article28). Moreira ED Jr, Brock G, Glasser DB, Nicolosi A, Laumann EO, Paik A, et al. Help-seeking behaviour for sexual problems: the global study of sexual attitudes and behaviors. Int J Clin Pract. 2005; 59:6–16.
Article29). Williams HA, Wilson ME, Hongladarom G, McDonell M. Nurses' attitudes toward sexuality in cancer patients. Oncol Nurs Forum. 1986; 13:39–43.30). Williams HA, Wilson ME. Sexuality in children and adolescents with cancer: pediatric oncology nurses' attitudes and behaviors. J Pediatr Oncol Nurs. 1989; 6:127–32.
Article31). Stead ML, Brown JM, Fallowfield L, Selby P. Lack of communication between healthcare professionals and women with ovarian cancer about sexual issues. Br J Cancer. 2003; 88:666–71.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Study of Knowledge, Attitudes, and Importance of Sexuality in the Aged
- A Comparative Study of the Awareness of Sexual Violence between Male and Female College Student
- Pregnant Women's Attitude and Satisfaction for Sexuality
- Discriminant Factors of Attitude Pattern toward Sexual Violence of College Women
- Sexual Attitude Changes after Sex Education according to Family Environmental Factors in Middle School Students