Korean Diabetes J.
2008 Feb;32(1):53-59. 10.4093/kdj.2008.32.1.53.
Prevalence and Clinical Characteristics of Aspirin Resistance in the Patients with Type 2 Diabetes Mellitus
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Korea.
- 2Department of Laboratory Medicine, Seoul National University College of Medicine, Korea.
- KMID: 2298110
- DOI: http://doi.org/10.4093/kdj.2008.32.1.53
Abstract
-
BACKGROUND: We examined the prevalence and clinical characteristics of aspirin resistance in the Korean patients with type 2 diabetes mellitus.
METHODS
We studied 181 Korean patients with type 2 diabetes mellitus who were taking aspirin (100 mg/day for > or = 3 months) and no other antiplatelet agents. The VerifyNow System was used to determine aspirin responsiveness. Aspirin resistance was defined as an aspirin reaction unit (ARU) > or = 550. We measured the cardio-ankle vascular index (CAVI) and ankle-brachial index (ABI) to evaluate arteriosclerosis. The anthropometric parameters, electrocardiogram, blood pressure, fasting plasma glucose, lipid profiles, hemoglobin A1c, highly sensitive C-reactive protein (hsCRP), homocysteine, and microalbuminuria were measured in each patient.
RESULTS
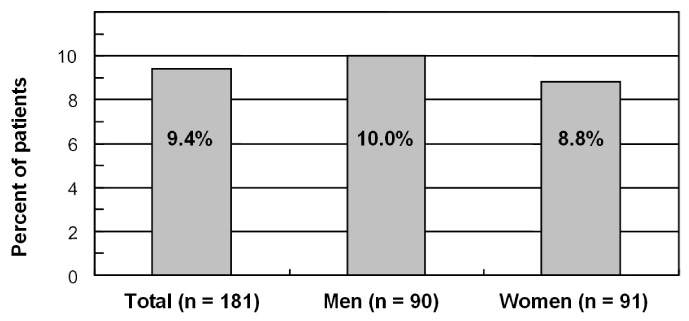
The prevalence of aspirin resistance in type 2 diabetic patients was 9.4% (17 of 181). Those who had aspirin resistance were older than those without aspirin resistance (64.6 +/- 10.6 vs. 59.8 +/- 8.1, P = 0.024). Aspirin resistance was not associated with fasting plasma glucose, total cholesterol, triglyceride, LDL-cholesterol, HDL-cholesterol, hemoglobin A1c, hsCRP, homocysteine, microalbuminuria, ABI, CAVI, and body mass index.
CONCLUSION
Prevalence of aspirin resistance in the Korean patients with type 2 diabetes mellitus was 9.4%. Although aspirin resistance was associated with old age, we could not find any good clinical parameter to predict it. Therefore, aspirin resistance should be evaluated in diabetic patients taking aspirin for prevention of cardiovascular complications.
MeSH Terms
-
Ankle Brachial Index
Arteriosclerosis
Aspirin
Blood Pressure
C-Reactive Protein
Cholesterol
Diabetes Mellitus, Type 2
Electrocardiography
Fasting
Glucose
Hemoglobins
Homocysteine
Humans
Plasma
Platelet Aggregation Inhibitors
Prevalence
Aspirin
C-Reactive Protein
Cholesterol
Glucose
Hemoglobins
Homocysteine
Platelet Aggregation Inhibitors
Figure
Reference
-
1. Nathan DM. Long-term complications of diabetes mellitus. N Engl J Med. 1993. 328:1676–1685.2. Ruderman NB, Haudenschild C. Diabetes as an atherogenic factor. Prog Cardiovasc Dis. 1984. 26:373–412.3. Collaborative Group of the Primary Prevention Project (PPP). Low-dose aspirin and vitamin E in people at cardiovascular risk: a randomised trial in general practice: Collaborative Group of the Primary Prevention Project. Lancet. 2001. 357:89–95.4. Anti-thrombotic Trialists Collaboration. Collaborative metaanalysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high-risk patients. BMJ. 2002. 324:71–86.5. Hankey GJ, Eikelboom JW. Aspirin resistance. Lancet. 2006. 367:606–617.6. Mckee SA, Sane DC, Deliargyris EN. Aspirin resistance in cardiovascular disease: A review of prevalence, mechanisms, and clinical significance. Thrombo Haemost. 2002. 88:711–715.7. Mehta J, Mehta P, Burger C, Pepine CJ. Platelet aggregation studies in coronary artery disease. Effect of aspirin. Atherosclerosis. 1978. 31:169–175.8. Buchanan MR, Brister SJ. Individual variation in the effects of ASA on platelet function: implications for the use of ASA clinically. Can J Cardiol. 1995. 11:221–227.9. Pappas JM, Westengard JC, Bull BS. Population variability in the effect of aspirin on platelet function. Arch Pathol Lab Med. 1994. 118:801–804.10. Mueller MR, Salat A, Stangl P, Murabito M, Pulaki S, Boehm D, Koppensteiner R, Ergun E, Mittlboeck M, Schreiner W, Losert U, Wolner E. Variable platelet response to low-dose aspirin and the risk of limb deterioration in patients submitted to peripheral arterial angioplasty. Thromb Haemost. 1997. 78:1003–1007.11. Eikelboom JW, Hirsh J, White JI, Johnston M, Yi Q, Yusuf S. Aspirin resistant thromboxane biosynthesis and the risk of myocardial infarction, stroke or cardiovascular death in patients at risk of high for cardiovascular event. Circulation. 2002. 105:1650–1655.12. Gum PA, Kottke-Marchant K, Welsh PA, White J, Topol EJ. A prospective, blinded determination of the natural history of aspirin resistance among stable patients with cardiovascular disease. J Am Coll Cardiol. 2003. 41:961–965.13. Fateh-Moghadam S, Plöckinger U, Cabeza N, Htun P, Reuter T, Ersel S, Gawaz M, Dietz R, Bocksch W. Prevalence of aspirin resistance in patients with type 2 diabetes. Acta Diabetol. 2005. 42:99–103.14. Mehta SS, Silver RJ, Aaronson A, Abrahamson M, Goldfine AB. Comparison of aspirin resistance in type 1 versus type 2 diaberes mellitus. Am J Cardiol. 2006. 97:567–570.15. Ultegra Rapid Platelet Function Assay-ASA (RPFA-ASA) [package insert]. 2002. San Diego, CA: Accumetrics Inc..16. Chen WH, Lee PY, Ng W, Tse HF, Lau CP. Aspirin resistance is associated with a high incidence of myonecrosis after nonurgent percutaneous coronary intervention despite clopidogrel pretreatment. J Am Coll Cardiol. 2004. 43:1122–1126.17. Schwartz KA, Schwartz DE, Pittsley RA, Mantz SL, Ens G, Sami A, Davis JM. A new method for measuring inhibition of platelet function by nonsteroidal antiinflammatory drugs. J Lab Clin Med. 2002. 139:227–233.18. Malinin A, Spergling M, Muhlestein B, Steinhubl S, Serebruany V. Assessing aspirin responsiveness in subjects with multiple risk factors for vascular disease with a rapid platelet function analyzer. Blood Coagulation and Fibrinolysis. 2004. 15:295–301.19. Lee PY, Chen WH, Ng W, Cheng X, Kwok JY, Tse HF, Lau CP. Low-dose aspirin increases aspirin resistance in patients with coronary artery disease. Am J Med. 2005. 118:723–727.20. Seok JI, Joo IS, Yoon JH, Choi YJ, Lee PH, Huh K, Bang OY. Can aspirin resistance be clinically predicted in stroke patients? Clin Neurol Neurosurg. 2008. 110:110–116.21. Pamukcu B. A review of aspirin resistance: definition, possible mechanisms, detection with platelet function tests, and its clinical outcomes. J Thromb Thrombolysis. 2007. 23:213–222.22. Michelson AD, Furman MI, Goldschmidt-Clermont P, Mascelli MA, Hendrix C, Coleman L, Hamlington J, Barnard MR, Kickler T, Christie DJ, Kundu S, Bray PF. Platelet GP IIIa Pl(A) polymorphisms display different sensitivities to agonists. Circulation. 2000. 101:1013–1018.23. Szczeklik A, Undas A, Sanak M, Frolow M, Wegrzyn W. Bleeding time, aspirin and the PlA1/A2 polymorphism of platelet glycoprotein IIIa. Br J Haematol. 2000. 110:965–967.24. Jefferson BK, Foster JH, McCarthy JJ, Ginsburg G, Parker A, Kottke-Marchant K, Topol EJ. Aspirin resistance and a single gene. Am J Cardiol. 2005. 95:805–808.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence and Clinical Characteristics of Aspirin Resistance in the Patients with Type 2 Diabetes
- Prevalence of aspirin resistance and related factors in patients with type-2 diabetes mellitus
- Pancreatogenic Diabetes
- Insulin Secretory Capacity and Insulin Resistance in Korean Type 2 Diabetes Mellitus Patients
- Genetic Diseases Associated with Diabetes Mellitus