J Korean Fract Soc.
2007 Oct;20(4):315-322. 10.12671/jkfs.2007.20.4.315.
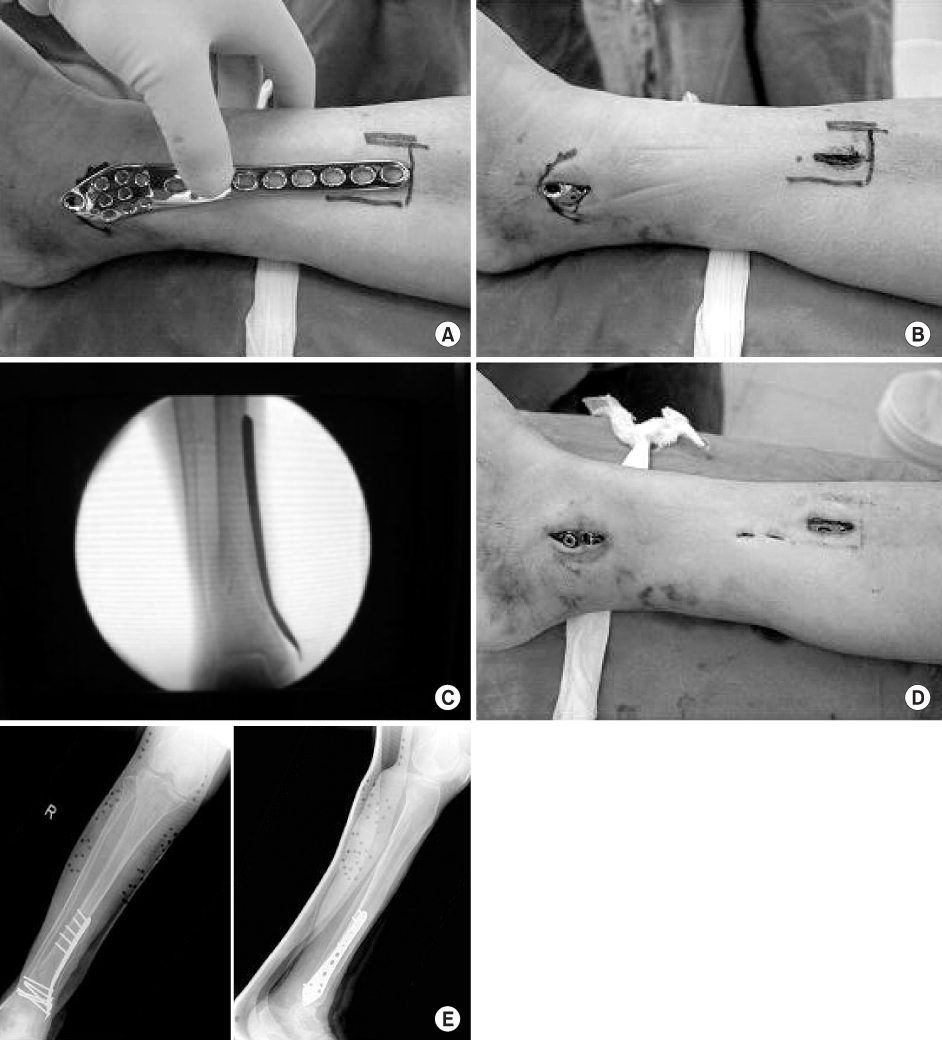
Minimally Invasive Percutaneous Plate Osteosynthesis Using Periarticular Plate for Distal Tibial Fractures
- Affiliations
-
- 1Department of Orthopaedic Surgery, Chungnam National University College of Medicine, Daejeon, Korea. osdr69@cnu.ac.kr
- KMID: 2297512
- DOI: http://doi.org/10.12671/jkfs.2007.20.4.315
Abstract
- PURPOSE
To evaluate the clinical results of minimally invasive percutaneous plate osteosynthesis using a periarticular plate (Zimmer, Warsaw, IN, USA) for distal tibia fractures.
MATERIALS AND METHODS
27 patients with distal tibia fractures were treated operatively by minimally invasive percutaneous plate osteosynthesis. The patients were followed for at least 1 year. The duration for bone union, complications after the surgery, the amount of skin irritation at the site of plate insertion was evaluated using the VAS score and the Olerud and Molander ankle score. The average age of the patients was 56 years old (range, 30~81 years) with an average follow up period of 21 months (range, 12~30 months).
RESULTS
The average time from trauma to surgery was 6 days (range, 2~19 days). 10 cases showed an associated distal fibular fracture. The average time for bone fusion was 14 weeks (range, 8~40 weeks) with 1 case of angular deformity with more than 5 degrees. The amount of skin irritation due to the periarticular plate resulted in a VAS score of 2.2 points. Evaluation of the ankle function test showed an average of 90.2 points, resulting in satisfactory.
CONCLUSION
The periarticular plate used in minimally invasive percutaneous plate osteosynthesis for distal tibia fractures was concluded to give a firm fixation of the fracture site as bony fusion could be acquired without any callus formation, and few skin irritation due to plate has seem to be an advantage.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Minimally Invasive Percutaneous Plate Osteosynthesis Using a Lateral Plate in Distal Tibial Fracture
Oog Jin Shon, Dae Sung Kim
J Korean Fract Soc. 2010;23(1):42-49. doi: 10.12671/jkfs.2010.23.1.42.Anatomically Percutaneous Wiring Reduction in Minimally Invasive Plate Osteosynthesis for Distal Tibial Fractures
Young-Mo Kim, Chan Kang, Deuk-Soo Hwang, Yong-Bum Joo, Woo-Yong Lee, Jung-Mo Hwang
J Korean Fract Soc. 2011;24(3):230-236. doi: 10.12671/jkfs.2011.24.3.230.Minimally Invasive Osteosynthesis with Locking Compression Plate for Distal Tibia Fractures
Sung-Kyu Kim, Keun-Bae Lee, Keun-Young Lim, Eun-Sun Moon
J Korean Fract Soc. 2011;24(1):33-40. doi: 10.12671/jkfs.2011.24.1.33.
Reference
-
1. Asche G. Result of the treatment of femoral and tibial fractures following interlocking nailing and plate osteosynthesis. A comparative retrospective study. Zentralbl Chir. 1989; 114:1146–1154.2. Baumgaertel F, Buhl M, Rahn BA. Fracture healing in biological plate osteosynthesis. Injury. 1998; 29:Suppl 3. C3–6.
Article3. Bolhofner BR, Carmen B, Clifford P. The results of open reduction and internal fixation of distal femur fractures using a biological (indirect) reduction technique. J Orthop Trauma. 1996; 10:372–377.
Article4. Bostman O, Hanninen A. The fibular reciprocal fracture in tibial shaft fractures caused by indirect violence. Arch Orthop Trauma Surg. 1982; 100:115–121.
Article5. Bradley GW, Mckenna GB, Dunn HK, Daniels AU, Statton WO. Effects of flexural rigidity of plates on bone healing. J Bone Joint Surg Am. 1979; 61:866–872.
Article6. Brumback RJ, McGarvey WC. Fractures of the tibial plafond. Orthop Clin North Am. 1995; 26:273–285.
Article7. Chang SA, Ahn HS, Byun YS, Kim JH, Bang HH, Kwon DY. Minimally invasive plate osteosynthesis in unstable fractures of the distal tibia. J Korean Fract Soc. 2005; 18:155–159.
Article8. Chrisovitsinos JP, Xenakis T, Papakostides KG, Skaltsoyannis N, Grestas A, Soucacos PN. Bridge plating osteosynthesis of 20 comminuted fractures of the femur. Acta Orthop Scand Suppl. 1997; 275:72–76.
Article9. Claes L, Heitemeyer U, Krischak G, Braun H, Hierholzer G. Fixation technique influence osteogenesis of comminuted fractures. Clin Orthop Relat Res. 1999; 365:221–229.10. Farouk O, Krettek C, Miclau T, Schandelmaier P, Tscherne H. The topography of the perforating vessels of the deep femoral artery. Clin Orthop Relat Res. 1999; 368:255–259.
Article11. Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis: Dose percutaneous plating disrupt femoral blood supply less then the traditional technique. J Orthop Trauma. 1999; 13:401–406.
Article12. Gerber C, Mast JW, Ganz R. Biological internal fixation of fractures. Arch Orthop Trauma Surg. 1990; 109:295–303.
Article13. Johner R, Wruhs O. Classification of tibial shaft fractures and correlation with results after internal fixation. Clin Orthop Relat Res. 1983; 178:7–25.14. Khoury A, Liebergall M, Mosheiff R, London E. Percutaneous plating of distal tibia fracture. Foot Ankle Int. 2002; 23:818–824.15. Krettek C, Schandelmaier P, Miclau T, Tscherne H. Minimally invasive percutaneous plate osteosynthesis(MIPPO) using the DCS in proximal and distal femoral fractures. Injury. 1997; 28:Suppl 1. A20–30.16. McFerran MA, Smith SW, Boulas HJ, Schwartz HS. Complications encountered in the treatment of pilon fractures. J Orthop Trauma. 1992; 6:195–200.
Article17. Mckibbin B. The biology of fracture healing in long bones. J Bone Joint Surg Br. 1978; 60:150–162.
Article18. Melis GC, Sotgiu F, Lepori M, Guido P. Intramedullary nailing in segmental tibial fractures. J Bone Joint Surg Am. 1981; 63:1310–1318.
Article19. Olerud C, Molander H. A scoring scale for symptoms evaluation after ankle fracture. Arch Orthop Trauma Surg. 1984; 103:190–194.20. Park KC, Park YS. Minimally invasive plate osteosynthesis for distal tibial metaphyseal fracture. J Korean Fract Soc. 2005; 18:264–268.
Article21. Phieffer LS, Goulet JA. Delayed unions of the Tibia. J Bone Joint Surg Am. 2006; 88:206–216.
Article22. Puno RM, Teynor JT, Nagano J, Gustilo RB. Critical analysis of result of 201 tibial shaft fracture. Clin Orthop Relat Res. 1986; 212:113–121.23. Rozbruch SR, Muller U, Gautier E, Ganz R. The evolution of femoral shaft plating technique. Clin Orthop Relat Res. 1998; 354:195–208.
Article24. Wenda K, Runkel M, Degrief J, Rudig L. Minimally invasive plate fixation in femoral shaft fractures. Injury. 1997; 28:Suppl 1. A13–A19.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Percutaneous Plate Stabilization Using a Medial Locking Plate for Proximal Tibial Fractures: Technical Note
- Minimally Invasive Percutaneous Plate Osteosynthesis Using a Lateral Plate in Distal Tibial Fracture
- Comparison of Results of Minimally Invasive Plate Osteosynthesis according to Types of Locking Plate in Distal Femoral Fractures
- Minimally Invasive Plate Osteosynthesis for Periarticular Tibial Fractures
- Comparative Analysis of Minimally Invasive Plate Osteosynthesis Using Periarticular Plate and Intramedullary Nailing in Distal Tibial Metaphyseal Fractures