Korean J Urol.
2006 Mar;47(3):287-292. 10.4111/kju.2006.47.3.287.
The Individualized Surgical Approach of Penoscrotal Transposition according to the Anatomical Position of the Penis
- Affiliations
-
- 1Department of Urology, Asan Medical Center, Seoul, Korea. kskim2@amc.seoul.kr
- 2Department of Urology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- KMID: 2294176
- DOI: http://doi.org/10.4111/kju.2006.47.3.287
Abstract
-
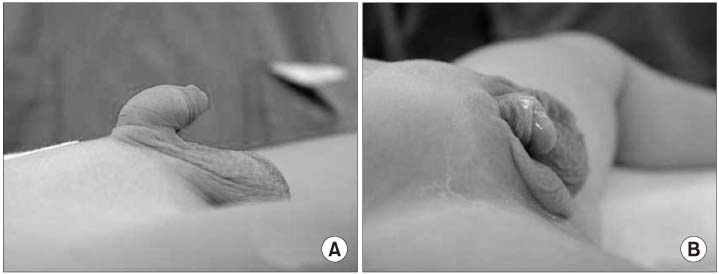
PURPOSE: Some patients still complain of a downward urine stream and a poor cosmetic result after the standard surgery, scrotoplasty because many patients with hypospadias basically have a low-set penis. We applied and evaluated a new concept for the surgery to improve the surgical results.
MATERIALS AND METHODS
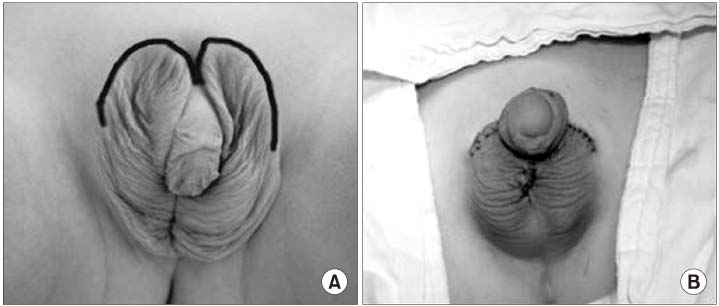
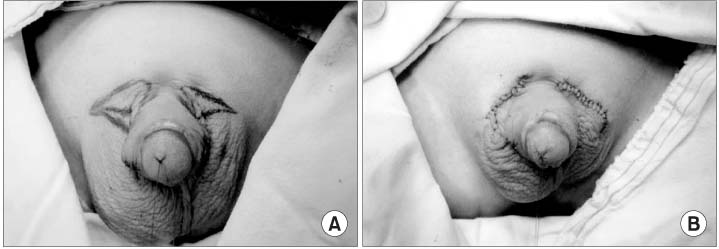
22 patients underwent surgery for PST from January 1997 to June 2004. We performed transposition of penis in 7 patients, scrotoplasty in 13 and partial wedge resection of the scrotum in 2 who had the mild form of PST. Transposition of the penis is a surgical technique in which the skin of the penoscrotal junction is incised circumferentially and phallus is delivered into the buttonhole that is created in the normal anatomical position for the penis. We evaluated the cosmetic results using a satisfaction scoring system (1 to 5 scores) that was completed by the parents and the functional results by checking the angle of the urine stream in the standing position.
RESULTS
There was no major complication for the 7 patients who underwent transposition of the penis. The mean satisfaction score was 4.6+/-0.8 and the angle of the urine stream was above 45 degrees in all patients. In the case of scrotoplasty, the mean satisfaction score was 3.6+/-0.9: half of them showed an angle of urine stream under 45 degrees and they complained of trouble when voiding.
CONCLUSIONS
As the anatomical location of the penis, scrotoplasty is good for the normally positioned penis with PST, transposition of the penis for the low-set penis, and partial resection of the scrotal skin for the mild form. This individualized approach could improve the cosmetic and functional results for patients with PST.
Keyword
Figure
Reference
-
1. Hoar RM, Calvano CJ, Reddy PP, Bauer SB, Mandell J. Unilateral suprainguinal ectopic scrotum: the role of the gubernaculum in the formation of an ectopic scrotum. Teratology. 1998. 57:64–69.2. Pinke LA, Rathbun SR, Husmann DA, Kramer SA. Penoscrotal transposition: review of 53 patients. J Urol. 2001. 166:1865–1868.3. Parida SK, Hall BD, Barton L, Fujimoto A. Penoscrotal transposition and associated anomalies; report of five new cases and review of the literature. Am J Med Genet. 1995. 59:68–75.4. Glenn JF, Anderson EE. Surgical correction of incomplete penoscrotal transposition. J Urol. 1973. 110:603–605.5. Kolligian ME, Franco I, Reda EF. Correction of penoscrotal transposition: a novel approach. J Urol. 2000. 164:994–997.6. Ware JE, Hays RD. Methods for measuring patient satisfaction with specific medical encounters. Med Care. 1988. 26:393–402.7. Levy JB, Darson MF, Bite U, Kramer SA. Modified pudendal-thigh flap for correction of penoscrotal transposition. Urology. 1997. 50:597–600.8. Perovic S, Vukadinovic V. Penoscrotal transposition with hypospadias: 1-stage repair. J Urol. 1992. 148:1510–1513.9. De Foor W, Wacksman J. Results of single staged hypospadias surgery to repair penoscrotal hypospadias with bifid scrotum or penoscrotal transposition. J Urol. 2003. 170:1585–1588.10. Jeong TY, Yoo SH, Lee JJ, Shin KY, Park HY, Lee TY, et al. Surgical outcome of proximal hypospadias with penoscrotal transposition. Korean J Urol. 1999. 40:756–759.11. Glassberg KI, Hansbrough F, Horowitz M. The Koyanagi-Nonomura 1-stage bucket repair of severe hypospadias without penoscrotal transposition. J Urol. 1998. 160:1104–1107.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Experiences in Surgical Correction of Incomplete Penoscrotal Transposition
- Two Cases of Congenital Scrotal Anomalies: Ectopic Scrotum, Accessory Scrotum
- Surgical Outcome of Proximal Hypospadias with Penoscrotal Transposition
- One Staged Pedicled Scrotal Skin Flap Urethroplasty for Perineal Hypospadias
- Changes in Lower Eyelid Positions after Individualized Lower Blepharoplasty