J Korean Ophthalmol Soc.
2015 Dec;56(12):1831-1839. 10.3341/jkos.2015.56.12.1831.
Changes in Lower Eyelid Positions after Individualized Lower Blepharoplasty
- Affiliations
-
- 1Department of Ophthalmology, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea. eye@cha.ac.kr
- KMID: 2148742
- DOI: http://doi.org/10.3341/jkos.2015.56.12.1831
Abstract
- PURPOSE
Various forms and degrees of morphological changes in the lower eyelid are presented in this study. A comprehensive, individualized clinical approach based on sound anatomical principles and lower lid stability is needed. We evaluated morphological outcomes of lower blepharoplasty by measuring lower eyelid position.
METHODS
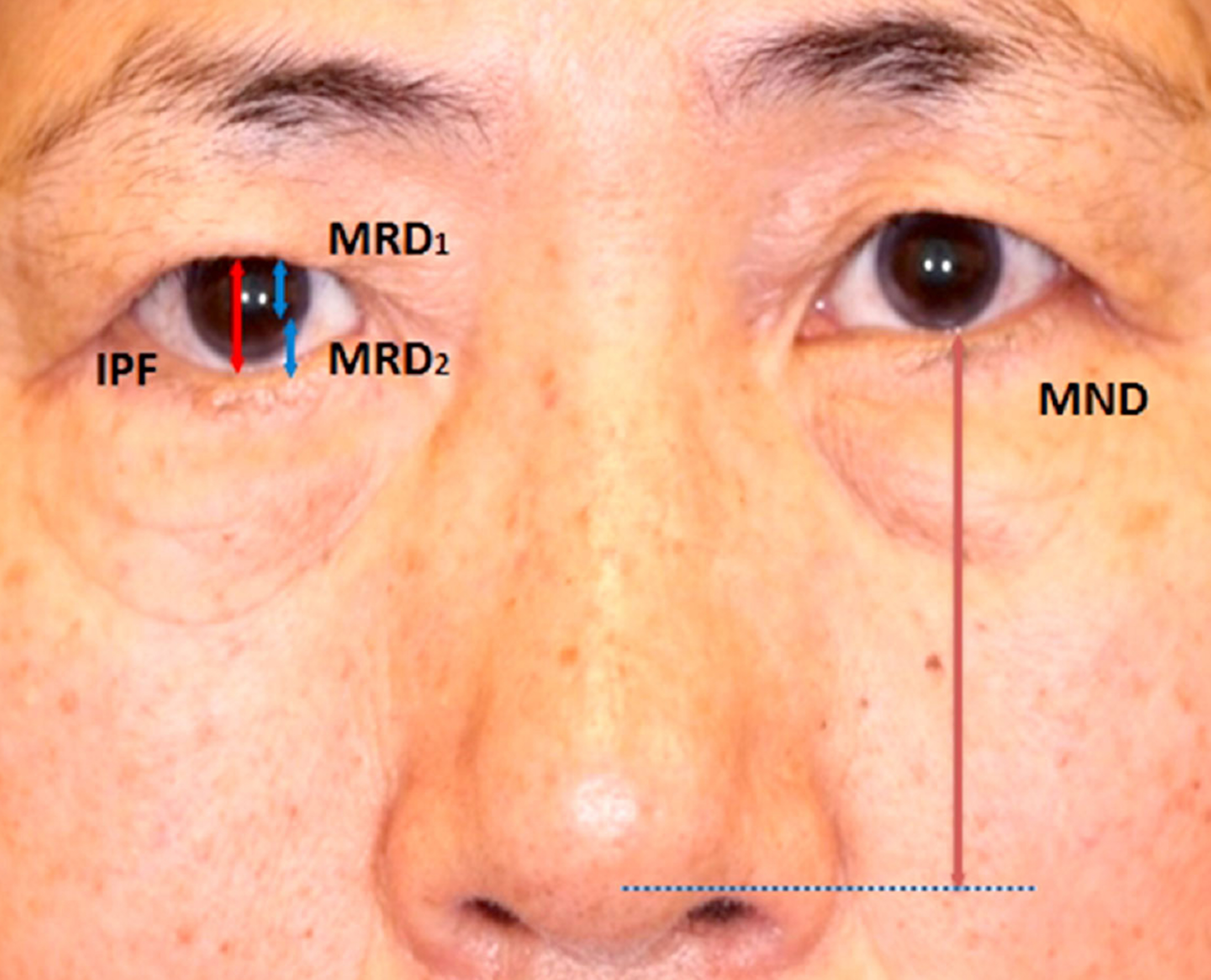
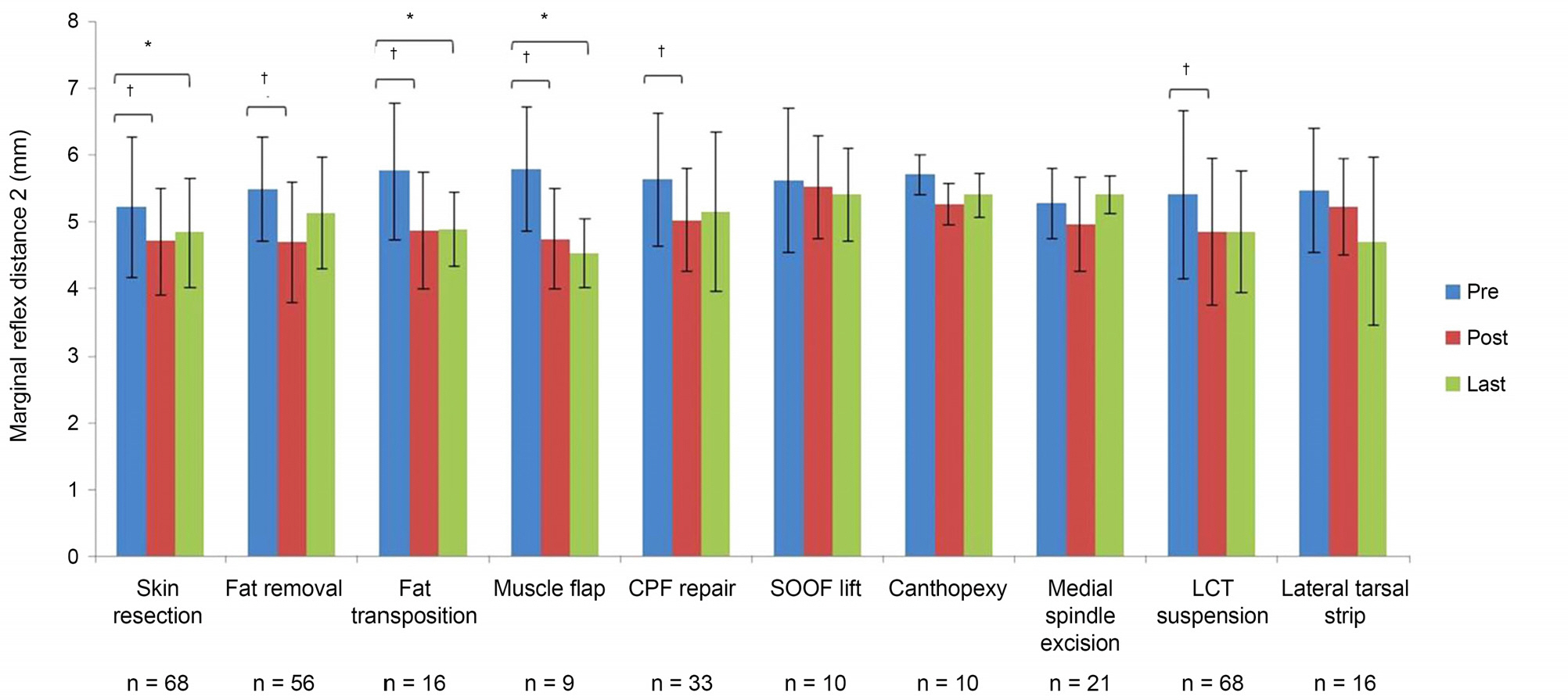
One hundred sixty-eight eyes underwent lower blepharoplasty between August 2009 and August 2014. The mean patient age was 62.1 +/- 13 years and mean follow-up period was 6.0 +/- 10.2 months. Lower eyelid position of 84 consecutive primary lower blepharoplasty patients (52 females and 32 males) was analyzed using digital images and measured with standardized data points using the Image J Program.
RESULTS
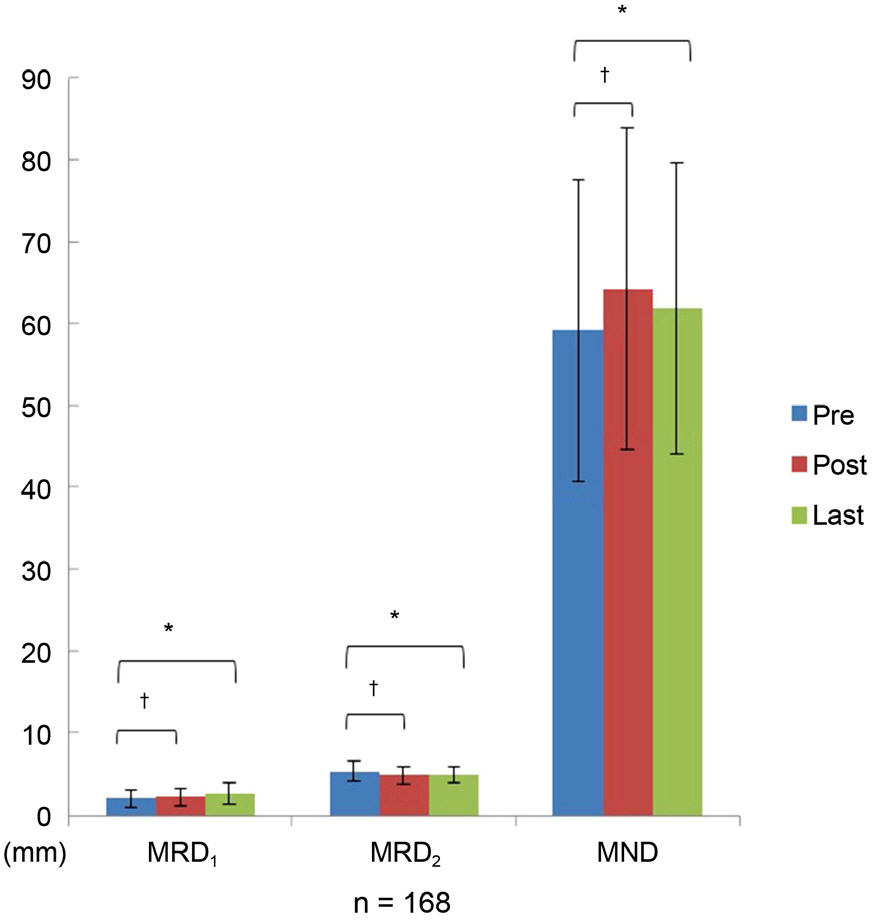
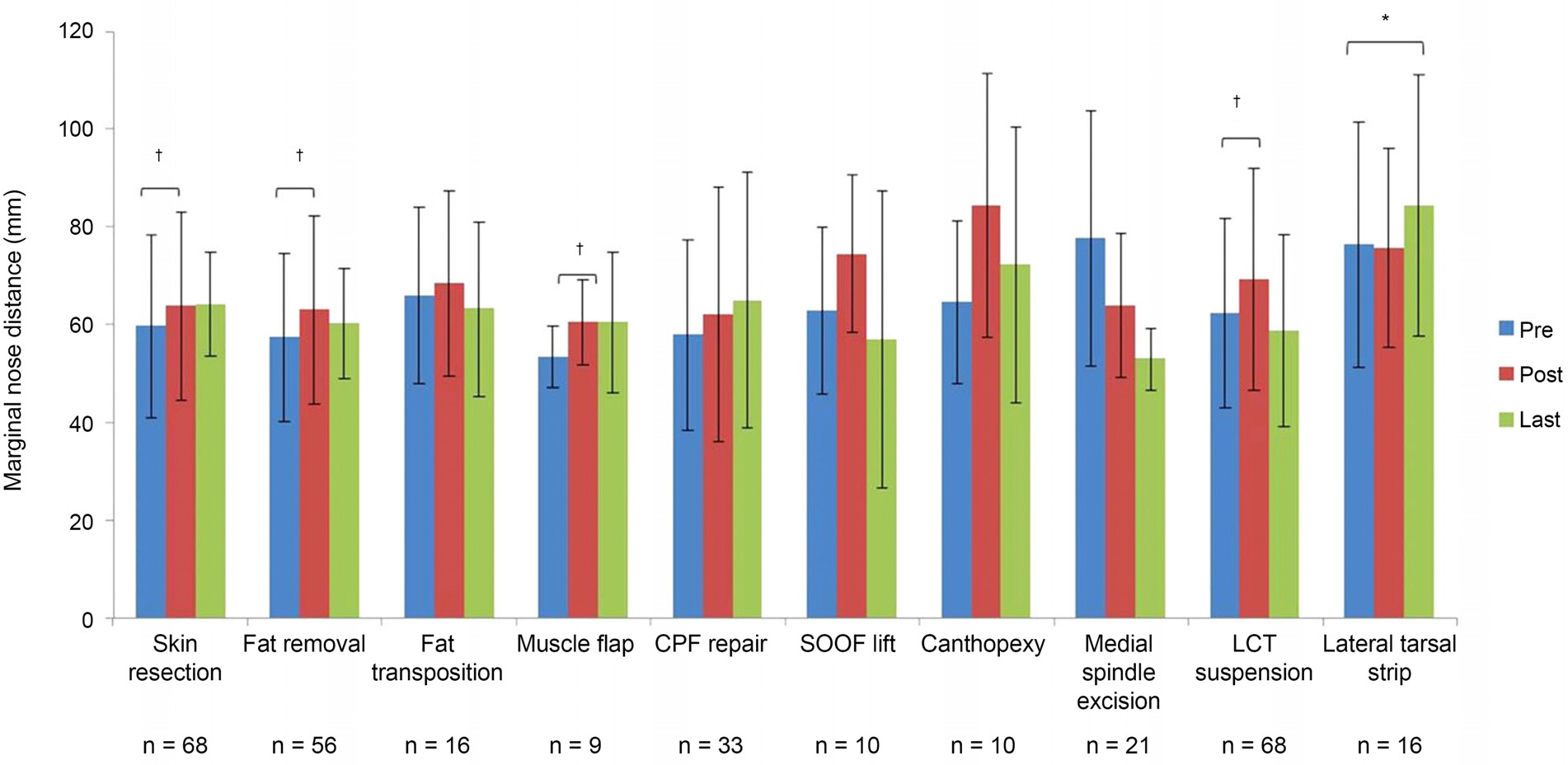
Of the 168 individualized lower eyelid blepharoplasties analyzed, margin reflex distance 2 (MRD2) decreased from 5.4 +/- 1.1 mm to 4.9 +/- 0.8 mm (p = 0.005) and marginal nose distance (MND) increased from 59.2 +/- 18.3 mm to 61.9 +/- 17.6 mm (p < 0.001). Complications after lower blepharoplasty were not observed.
CONCLUSIONS
The position of the lower eyelid improved after individualized lower blepharoplasty that addressed all the anatomical lower eyelid findings was performed.
Keyword
Figure
Cited by 3 articles
-
Upper and Lower Eyelid Positions in Several Korean Age Groups
Sukyeon Lee, Jinhwan Park, Janghoon Lee, Jaehoon Na, Hwa Lee, Sehyun Baek
J Korean Ophthalmol Soc. 2018;59(7):606-612. doi: 10.3341/jkos.2018.59.7.606.Effect of Transconjunctival Approach Lower Blepharoplasty Combined with Pinch Skin Excision Technique in Elderly Patients
Boyoon Choi, Sungwon Yang, Jinhwan Park, Hwa Lee, Sehyun Baek
J Korean Ophthalmol Soc. 2019;60(3):205-209. doi: 10.3341/jkos.2019.60.3.205.Changes in Tear Meniscus Height Following Lower Blepharoplasty as Measured by Optical Coherence Tomography
Sang Min Lee, Sok Joong Chung, Jong Seo Park, Helen Lew
Korean J Ophthalmol. 2018;32(5):344-352. doi: 10.3341/kjo.2017.0125.
Reference
-
References
1. Nishihira T, Ohjimi H, Eto A. A new digital image analysis system for measuring blepharoptosis patients’ upper eyelid and eyebrow positions. Ann Plast Surg. 2014; 72:209–13.
Article2. Macdonald KI, Mendez AI, Hart RD, Taylor S. Eyelid and brow asymmetry in patients evaluated for upper lid blepharoplasty. J Otolaryngol Head Neck Surg. 2014; 43:36.
Article3. Coombes AG, Sethi CS, Kirkpatrick WN. . A standardized dig-ital photography system with computerized eyelid measurement analysis. Plast Reconstr Surg. 2007; 120:647–56.
Article4. Chi MJ, Park MS, Baek SH. The effect of transconjunctival lower blepharoplasty combined with pinch skin excision technique. J Korean Ophthalmol Soc. 2007; 48:755–60.5. Jacono AA, Moskowitz B. Transconjunctival versus trans-cutaneous approach in upper and lower blepharoplasty. Facial Plast Surg. 2001; 17:21–8.
Article6. Zarem HA, Resnick JI. Expanded applications for transconjunctival lower lid blepharoplasty. Plast Reconstr Surg. 1999; 103:1041–3. discussion 1044-5.
Article7. Nassif PS. Lower blepharoplasty: transconjunctival fat repositioning. Facial Plast Surg Clin North Am. 2005; 13:553–9. vi.
Article8. Liu D, Stasior OG. Lower eyelid laxity and ocular symptoms. Am J Ophthalmol. 1983; 95:545–51.
Article9. Ko SJ, Kim SD. Involutional ectropion repair with the modified medial spindle and the lateral tarsal strip procedure. J Korean Ophthalmol Soc. 2012; 53:187–92.
Article10. Nowinski TS, Anderson RL. The medial spindle procedure for in-volutional medial ectropion. Arch Ophthalmol. 1985; 103:1750–3.
Article11. Levine MR. Manual of Oculoplastic Surgery, 4th ed. Thorofare: SLACK Inc.,. 2010; 173–82.12. White WL, Woog JJ. Lower eyelid malpositions. In: Albert DM, Jacobiec FA, eds. Principles and Practice of Ophthalmology, 2nd ed. Philadelphia: WB Saunders,. 1994; 596–693.13. Wright KA. Interactive ophthalmology on CD-ROM-textbook and review, 1st ed. Baltimore: Williams & Wilkins,. 1998; 5191–326.14. Bashour M, Harvey J. Causes of involutional ectropion and en-tropion-age-related tarsal changes are the key. Ophthal Plast Reconstr Surg. 2000; 16:131–41.
Article15. Stefanyszyn MA, Hidayat AA, Flanagan JC. The histopathology of involutional ectropion. Ophthalmology. 1985; 92:120–7.
Article16. Seo HR, Ahn HB. Morphological changes of the eyelid according to age. J Korean Ophthalmol Soc. 2009; 50:1461–7.
Article17. Ji JY, Kim YD. Acellular dermal allograft for the correction of eye-lid retraction. J Korean Ophthalmol Soc. 2005; 46:1–9.18. Chang EL, Rubin PA. Upper and lower eyelid retraction. Int Ophthalmol Clin. 2002; 42:45–59.
Article19. Kim SY, Shin SJ, Yang SW, Han SH. Microscopic anatomy of the lower eyelid in Koreans. J Korean Ophthalmol Soc. 2006; 47:292–6.20. Jeong WJ, Hur MC, Ahn HB. The characteristics of senile en-tropion of lower eyelid with kinked tarsus. J Korean Ophthalmol Soc. 2011; 52:777–82.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reconstruction of Lower Eyelid Defect using Neighboring Remnant Skin
- Case of Prominent Periorbital Vein after Lower Eyelid Blepharoplasty Treated with a Long-pulse 1,064-nm Neodymium: Yttrium-aluminum-garnet Laser
- The Importance of Lower Eyelid Position in Aging Blepharoplasty
- Tarsal Margin Rotation with Blepharoplasty to Correct Cicatricial Entropion of The Upper Eyelid
- Lower Blepharoplasty in Aged Persons